Fig. 9.2
Relationship of conus muscle to outflow tracts and ventricular septum in normal anatomy, anterior malalignment in tetralogy of Fallot, and posterior malalignment in interrupted aortic arch. CS conal septum, MV mitral valve, TV tricuspid valve, VS ventricular septum (By permission of: Weinburg [47])
When there is malalignment or displacement of the conus and conal septum from the remainder of the plane of muscular trabecular septum, specifically the portion of ventricular septum comprised by the two limbs (the ‘Y’) of septal band (or trabecula septomarginalis), the resultant defect is oftentimes referred to as a malalignment VSD. This type of defect is usually characterized by anterior or posterior malalignment of the conal septum. Such defects can have a more complex three-dimensional nature, with the surrounding margins not completely oriented in the same plane. In these defects the borders of the VSD can variously comprise muscular (trabecular septum), conal septum, a semilunar valve (or valves), ventriculo-infundibular fold, or intervalvular fibrosa (Fig. 9.3). Since the surgical repair of such defects can involve a complex re-routing of blood flow to the appropriate semilunar valve, closure of a ventricular communication in such instances often occurs by attachment of the patch to muscular rims that differ from those that comprise the actual borders of the VSD [10]. Thus, the “true” VSD can differ from the “surgical” VSD. Moreover, in this type of VSD the malaligned conal septum can impinge upon the outflow tract beneath a semilunar valve, resulting in obstruction of the affected outflow tract and hypoplasia of the associated semilunar valve and great artery. With in tetralogy of Fallot and some cases of double outlet right ventricle, the conal septum is malaligned anteriorly and superiorly resulting in narrowing of the right ventricular outflow tract (RVOT) and possibly hypoplasia of the pulmonary valve. This malalignment also results in the aorta overriding the remaining plane of the interventricular septum, hence the aortic valve forms the “roof” of the VSD. Conversely, posterior malalignment of the conal septum results in narrowing of the left ventricular outflow tract (LVOT) and possible accompanying hypoplasia of the aortic valve. This type of defect has a high association with aortic arch obstruction, including coarctation or interruption of the aorta.
Fig. 9.3
Diagram showing three communications (A–S, B–S, C–S) potentially termed the “ventricular septal defect” in a patient with an overriding semilunar valve. (A) Infundibular septum; (B) Coapted leaflets of overriding semilunar valve; (C) Ventriculoinfundibular fold or area of arterial-atrioventricular valve fibrous continuity. S septal crest (By permission of: Macartney et al. [10])
Perimembranous (also known as conoventricular, membranous, infracristal, or paramembranous) VSDs involve the membranous portion of ventricular septum. The membranous septum is a specific region seen best by pathology as a thin region of the ventricular septum adjacent to the tricuspid valve and aortic valve. There is no muscle in this region and the superior portion is bordered by the aortic valve. As its name suggests, in pathologic specimens, this region is thin and almost transparent, easily transilluminated when held up to light. The term peri-membranous implies that such VSDs often represent not only a deficiency of membranous septum, but also extension to areas surrounding the membranous septum. Defects in this region can extend to the right and left aortic valve cusps as well, due to their proximity to the membranous septum. There can also be redundant, aneurysmal tricuspid valve tissue, which sometimes partially (or even completely) occludes the underlying defect. At times, the true defect in the septum may be large but the effective orifice quite small secondary to the tricuspid valve tissue. Thus, the tricuspid valve should be assessed for any incompetence. In some instances, VSD flow travels through the perimembranous VSD directly into the right atrium, or alternatively it is deflected via tricuspid valve tissue into the right atrium. This condition results in a left ventricle (LV) to right atrial shunt, also known as a “Gerbode” defect.
The remainder of the trabecular septum is considered just that—the trabecular or muscular septum. Defects in this portion of the septum are known as muscular VSDs, and can occur anywhere along the muscular septum—mid, anterior, apical, and posterior. Both posterior muscular and inlet/AV canal defects are situated close to the posterior border of ventricular septum, but the posterior muscular VSDs are located more inferiorly. Muscular VSDs can be of any size and shape; they can be single or multiple. When there are numerous separate muscular VSDs of varying size, the ventricular septum is popularly referred to as the so-called “Swiss cheese” septum. Upon surgical inspection, these multiple defects may in fact be a single large defect that has flow seen through multiple trabeculations on the right ventricular side by color flow Doppler. Indeed, due to the heavy trabeculations and oftentimes associated right ventricular hypertrophy from a large and longstanding shunt, the individual defects can be very difficult to assess surgically or challenging to address if they are located deep in the right ventricular (RV) apex as the surgeon is inspecting from the RV side.
There are two additional considerations regarding VSDs. First, combinations of different types of VSDs can occur together, such as a large perimembranous VSD coexisting with one or more muscular VSDs. Second, despite the specific locations of each type of VSD, in some instances a large enough defect will extend and overlap into various regions, such as a large perimembranous VSD extending into the inlet septum. The TEE examiner should be aware of both of these possibilities.
Evaluation of Ventricular Septal Defects by TEE
The ventricular septum can be well imaged by TEE [11]. Starting from the standard transverse plane at 0° or so in the mid esophageal four chamber (ME 4 Ch) view, the crux of the heart, the inlet septum, and most of the muscular trabecular septum can be well seen from the AV valves down to the apex as previously described. By withdrawing the probe and flexing anteriorly (anteflexing) from the crux, we pass through the perimembranous region adjacent to the tricuspid valve when the LVOT is in view. From here, a perimembranous defect can be seen by two-dimensional (2D) imaging and any involvement of tricuspid valve aneurysmal tissue can be detected (Fig. 9.4, Video 9.1). Color flow Doppler demonstrates the shunting through a perimembranous VSD well, and there is usually a favorable angle of interrogation for spectral Doppler (pulsed and continuous wave). If there is any LV to right atrial shunting through the perimembranous VSD, it can be adequately seen in the ME 4 Ch view (multiplane angle 0°). It is also important to assess for any prolapse of tissue into the LVOT or for any other evidence of sub-aortic obstruction such as a discrete membrane or ridge. Another important consideration is that the size of the defect in the septum as noted by imaging, and the effective orifice as shown by color flow Doppler, can be quite different if aneurysmal tricuspid valve tissue causes partial obstruction of the defect. If anteflexion is continued with slight withdrawal of the probe, the image can be brought to that of a mid esophageal right ventricular inflow-outflow (ME RV In-Out) view (multiplane angle 60–90°). This view (Chap. 4) is comparable to an inverted transthoracic parasternal short axis view, and images perimembranous as well as outlet septal (supracristal) defects quite nicely (Fig. 9.5, Video 9.2).
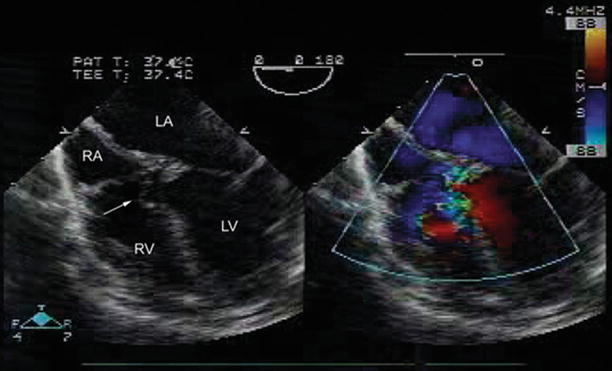
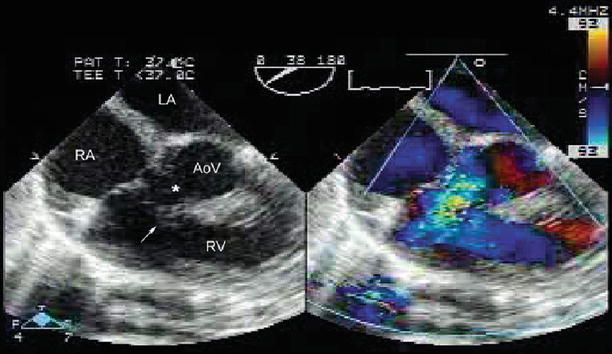
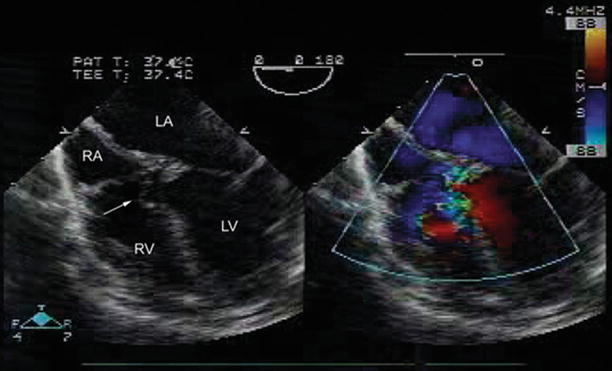
Fig. 9.4
Left sided image from mid esophageal four chamber view (multiplane angle 0°) shows a perimembranous ventricular septal defect (VSD) with tricuspid valve aneurysmal tissue as noted by the arrow. Right sided image demonstrates left to right shunting by color flow Doppler across the VSD. LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
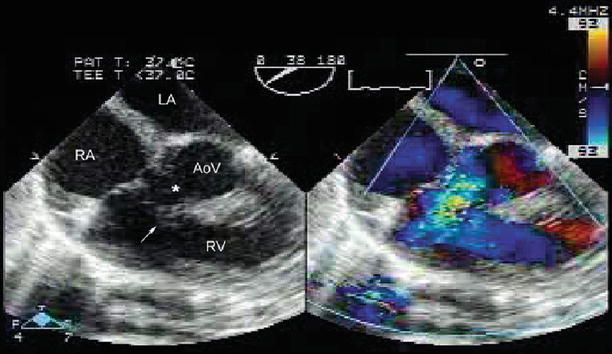
Fig. 9.5
Modified mid esophageal right ventricular inflow-outflow view with multiplane angle ~40° shows a perimembranous VSD (asterisk) with aneurysmal tricuspid valve tissue shown by arrow. This view is comparable to a parasternal short axis view of the aortic valve. AoV aortic valve, LA left atrium, RA right atrium, RV right ventricle
Evaluation of the muscular (trabecular) septum can be performed effectively from the ME 4 Ch view, multiplane angle 0°. Retroflexion of the probe allows evaluation of inlet and muscular VSDs. With probe anteflexion, the mid and anterior muscular VSD can be visualized. Imaging should be used in conjunction with color flow Doppler mapping, as many muscular VSDs (particularly smaller defects) might not be well seen solely with 2D imaging. It is important to maintain an adequate size color flow Doppler sector, and carefully evaluate all portions of the muscular ventricular septum. This is particularly important with apical muscular VSDs, which are generally farther from the TEE probe and can be easily missed if the color flow sector is not extended completely to the apex (Fig. 9.6). Representative muscular VSDs are displayed in Videos 9.3 through 9.7 as follows: Video 9.3-large inlet defect; Video 9.4a-moderate size mid-muscular defect; Video 9.4b-a mid-muscular VSD in a patient with D-transposition of the great arteries and RV to LV shunting; Video 9.5-a small apical muscular VSD seen more readily with color flow Doppler; Videos 9.6 and 9.7-several defects in different locations of the muscular septum. Additional visualization of the mid and apical portions of muscular septum can also be provided by advancing the TEE probe into the stomach (transgastric position) while maintaining probe anteflexion, to obtain the transgastric basal short axis (TG Basal SAX) and mid short axis (TG Mid SAX) views (Video 9.4a). These views can be useful for visualizing postero-inferior and apical muscular VSDs that are sometimes difficult to image from other TEE windows.
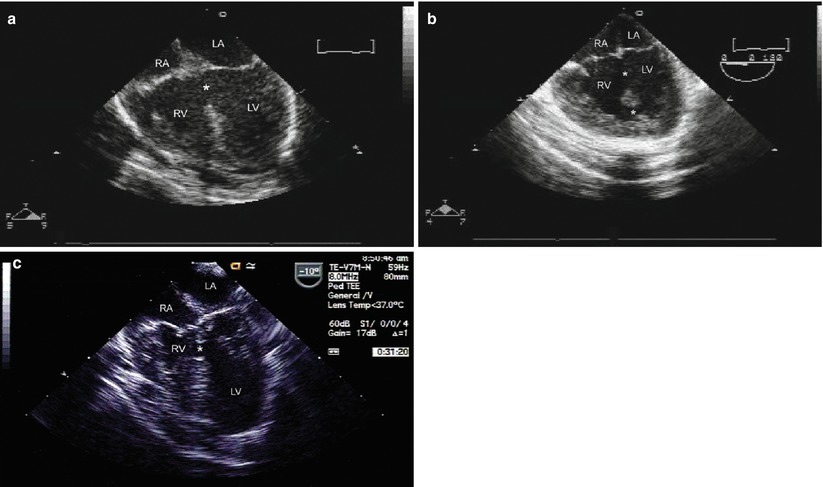
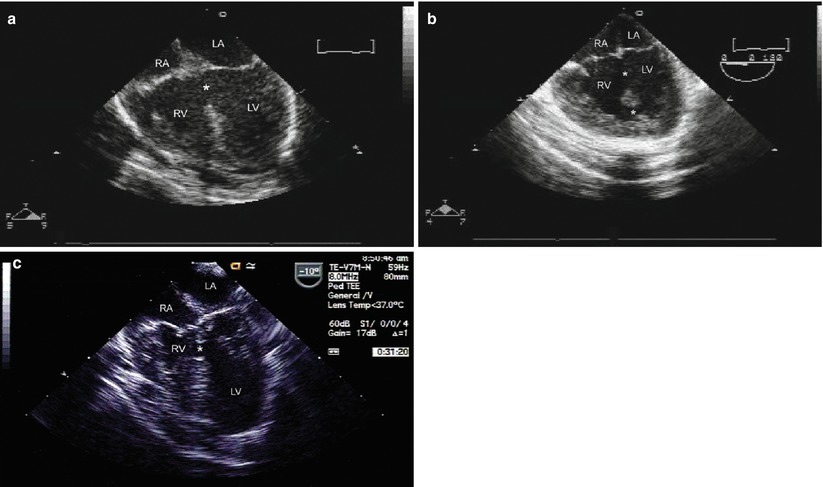
Fig. 9.6
Examples of muscular ventricular septal defect (VSD), shown from mid esophageal four chamber view. (a) Shows a large inlet VSD at the level of the crux of the heart. (b) Shows large inlet and apical muscular VSDs. (c) shows right ventricular hypoplasia with small posterior muscular VSD. For all figures, multiplane angle is approximately 0°. LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
As with any type of imaging, all anatomy should be evaluated from more than one plane. With modern multiplane TEE transducers, there is the luxury of being able to sweep from a transverse (0°) plane to the sagittal (90°) plane and beyond (even to 180°), while evaluating all planes in between. It should be remembered that every heart is different and, as often seen with congenital heart disease, the heart might not occupy its usual position. Therefore the multiplane angles given in this text are not absolute, and might need to be adjusted to obtain an optimal visualization of the VSD. Some patients have a better sagittal view at 80° or 110° rather than directly at 90°. Each patient must be assessed individually.
With the transducer oriented in a long axis plane (multiplane angle 100–130°), the mid esophageal long axis (ME LAX) view is obtained, providing excellent visualization of the LVOT. With slight rightward (counterclockwise) rotation, the RVOT can be visualized, and more anterior superior VSDs, as well as defects in the outlet septum (see below), can be well seen. This particular view, in association with the complementary mid esophageal RV inflow-outflow (ME RV In-Out) view (multiplane angle 60–90°), provides excellent visualization of any LV or RV outflow tract obstruction, either valvar or subvalvar (Video 9.8). In the case of the RV outflow tract, subpulmonary obstruction due to a superiorly displaced moderator band and/or anomalous muscles bundles, also known as double chambered RV, becomes much more visible when utilizing these TEE views. Double chambered RV carries a well-known association with perimembranous VSDs [12].
Supracristal VSDs can be visualized in several planes. Using the ME (Chap. 4) view and with the multiplane angle at 0° the defect can be seen although probe anteflexion is often necessary because of the more anterior and superior location of the defect (Fig. 9.7a). As noted previously, the standard ME RV In-Out view can also be helpful for distinguishing perimembranous from supracristal defects; when viewed as a clock face, perimembranous defects are seen between 7 and 10 o’clock, and supracristal defects from 3 to 6 o’clock, analogous to the views obtained with an inverted transthoracic parasternal short axis view. The supracristal defect is often seen very well seen from a near sagittal plane in the mid esophageal window, using the ME RV In-Out view, with a multiplane angle between 80 and 90°. With this view, the deficient conal septum becomes readily apparent, along with the location of the VSD directly adjacent to both semilunar valves. The semilunar valves can sometimes be seen in fibrous continuity with each other. If an aortic cusp prolapses through the defect, the protruding cusp is readily seen by both imaging and color flow Doppler (Fig. 9.7b, Video 9.9). During the evaluation of supracristal VSDs, the LVOT and aortic valve should also be evaluated, with special attention paid to any possible aortic valve distortion and/or aortic valve insufficiency. For this type of VSD, the ME RV In-Out view provides a good angle of interrogation for spectral Doppler quantification of the VSD jet.
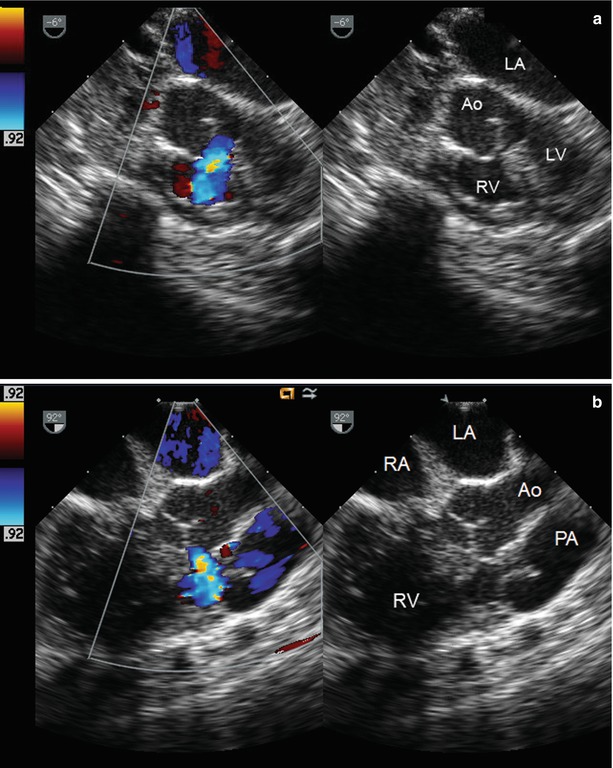
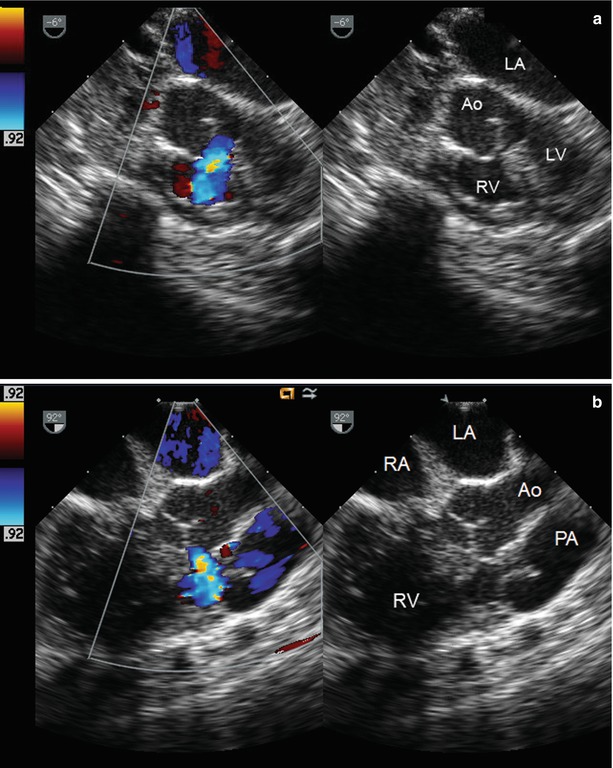
Fig. 9.7
Supracristal ventricular septal defect visualized from mid esophageal position, with a multiplane angle of 0° (a) and 90° (b). Note the right coronary cusp of aortic valve partly protruding through the defect. Ao aorta, LA left atrium, LV left ventricle, PA main pulmonary artery, RA right atrium, RV right ventricle
The ME LAX view (multiplane angle 100–130°) is also excellent for assessing malalignment VSDs. As mentioned previously, these defects may be categorized as being anteriorly or posteriorly malaligned depending on the positioning of the conal septum. Posterior malalignment of the conal septum will result in protrusion of the conal septum into the LVOT resulting in varying degrees of sub-aortic narrowing and obstruction; this type of defect is often associated with aortic arch hypoplasia, coarctation, or interruption. Anterior malalignment of the conal septum often results in an aorta that overrides the VSD, with varying degrees of subpulmonary and pulmonary valve narrowing and obstruction due to to the conal septum protruding into the RVOT—namely, tetralogy of Fallot (Fig. 9.8, Video 9.10). With a posterior malalignment VSD, a significant degree of LVOT obstruction might not be fully recognized since some blood can flow left to right through the VSD into the low resistance pulmonary vascular bed, and a significant gradient might not be seen across the LVOT by Doppler assessment. In such cases, evaluation by 2D imaging of the LVOT and aortic valve, including linear measurements of LVOT structures such as aortic valve annulus, plays an important role [13]. It is imperative to recognize and understand this anatomy and physiology at the time of the preoperative study so that these issues may be discussed with the surgeon prior to initiating the surgery.
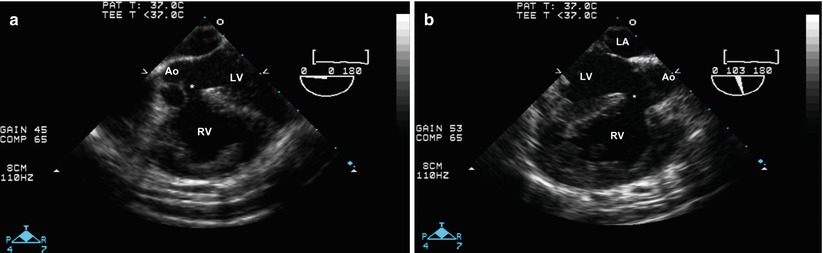
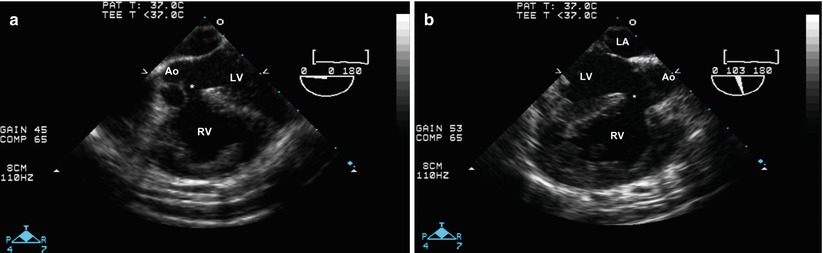
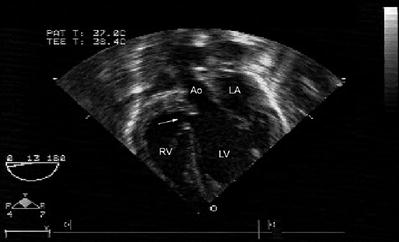
Fig. 9.8
Modified mid esophageal aortic valve short axis view at 0° (a) and modified mid esophageal long axis view at a multiplane angle of 100° (b). These views show the overriding aorta with anteriorly malaligned conal septum and large malalignment ventricular septal defect in a patient with tetralogy of Fallot. Ao aorta, LA left atrium, LV left ventricle, RV right ventricle
Certain TEE views produce images that closely resemble their transthoracic counterparts (e.g. parasternal short axis view, noted above). Thus, keeping the probe in an anteflexed position (multiplane angle 0°) and advancing into the lower esophageal and transgastric positions will produce the TG Basal SAX and TG Mid SAX views, which are analogous to the parasternal short axis views of the mid and apical portions of the ventricles. As noted above, these views can be useful for visualizing mid and apical muscular VSDs, both by imaging and color flow Doppler (Video 9.4a). In addition, the LV can be quantitatively assessed for function and septal wall motion. Thus the muscular septum can be thoroughly interrogated as the evaluation extends towards the apex (Fig. 9.9) and then superiorly towards the lower and mid esophagus. These views can be obtained with a combination of withdrawing and advancing the probe while retro or anteflexing.
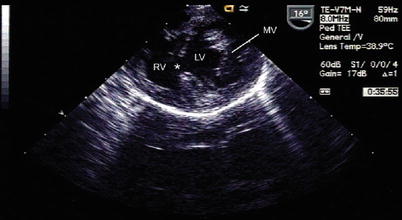
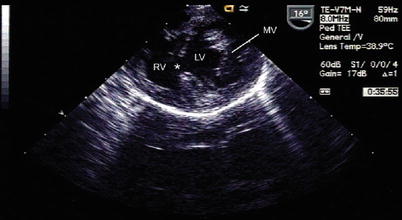
Fig. 9.9
Transgastric mid short axis view of the ventricles with en-facevisualization of the mitral valve and small mid-muscular ventricular septal defect. LV left ventricle, MV mitral valve, RV right ventricle
With further advancement and anteflexion of the TEE probe, the deep transgastric views can produce excellent images comparable to the subcostal (subxiphoid) views in transthoracic imaging [14–16]. As with much of pediatric subcostal imaging, the image should be inverted on the screen. In the deep transgastric position with multiplane angle at 0–10°, the deep transgastric long axis (DTG LAX) view produces images comparable to that of a subcostal coronal plane. The crux of the heart and inlet septum can be visualized as well as most of the muscular septum, including lower muscular and apical septum. With further advancement and anteflexion of the probe, the imaging plane steers more posteriorly to visualize the LVOT and the membranous septum. Perimembranous VSDs can be well seen from the coronal sections produced by the DTG LAX view as well as the deep transgastric sagittal (DTG Sagittal) view (multiplane angle 80–110°), the latter with clockwise rotation of the probe to angle slightly away from the RVOT. Often, redundant aneurysmal tissue can be noted partially occluding the defect (Fig. 9.10, Video 9.11). Again, the LVOT should be assessed for associated subaortic stenosis or aortic regurgitation. When available, the deep transgastric position provides an excellent viewpoint from which to assess the LVOT in cases of sub-aortic or aortic valve obstruction. These views afford the best angle to obtain spectral Doppler interrogation since the LVOT is directly in line with the cursor. When using the DTG LAX view, further withdrawal of the probe will bring the RVOT into view but oftentimes optimal contact with the stomach can be lost at this point since the RVOT is fairly anterior. Transitioning to a DTG Sagittal view with a multiplane angle of 80–110° is comparable to the transthoracic subcostal sagittal plane, and this view can sometimes provide better imaging of the anterior RVOT. The short axis plane of the ventricles can be seen, and this view usually provides the best planes to image the RVOT in cases of tetralogy of Fallot and double chambered RV since the malaligned conal septum and anomalous muscle bundles can be clearly seen (Fig. 9.11, Video 9.12). This TEE view also provides an excellent angle for spectral Doppler assessment of RVOT obstruction. When increased velocities are obtained in the RVOT, a detailed 2D evaluation should also be performed for anatomic correlation, because in addition to RVOT obstruction, increased velocities in the outflow tract can occur for other reasons: (a) flow-related increases in velocity due to the presence of a significant left to right shunt, and (b) a high velocity flow transmitted from the adjacent VSD.