Chapter 27 Ventilatory failure
 Ventilatory failure occurs when alveolar ventilation becomes too low to maintain normal arterial blood gas partial pressures.
Ventilatory failure occurs when alveolar ventilation becomes too low to maintain normal arterial blood gas partial pressures. There are many causes, involving the respiratory centre, the respiratory muscles or their nerve supply and abnormalities of the chest wall, lung or airways.
There are many causes, involving the respiratory centre, the respiratory muscles or their nerve supply and abnormalities of the chest wall, lung or airways.Definitions
Respiratory failure is defined as a failure of maintenance of normal arterial blood gas partial pressures. Hypoxia as a result of cardiac and other extra-pulmonary forms of shunting are excluded from this definition. Respiratory failure may be subdivided according to whether the arterial Pco2 is normal or low (type 1) or elevated (type 2). Mean of the normal arterial Pco2 is 5.1 kPa (38.3 mmHg) with 95% limits (2 s.d.) of±1.0 kPa (7.5 mmHg). The normal arterial Po2 is more difficult to define because it decreases with age (page 194), and is strongly influenced by the concentration of oxygen in the inspired gas. Mechanisms that contribute to respiratory failure include ventilatory failure (reduced alveolar ventilation) and venous admixture as a result of either pure intrapulmonary shunt or ventilation perfusion mismatch (Chapter 8).
Pattern of Changes in Arterial Blood Gas Tensions
Figure 27.1 shows, on a Po2/Pco2 diagram, the typical patterns of deterioration of arterial blood gases in respiratory failure. The shaded area indicates the normal range of values with increasing age corresponding to a leftward shift. Pure ventilatory failure in a young person with otherwise normal lungs would result in changes along the broken line. Chronic obstructive pulmonary disease (COPD), the most common cause of predominantly ventilatory failure, occurs in older people, and the observed pattern of change is shown within the upper arrow in Figure 27.1. The limit of survival, while breathing air, is reached at a Po2 of about 2.7 kPa (20 mmHg) and Pco2 of 11 kPa (83 mmHg). The limiting factor is not Pco2 but Po2. This prevents the rise of Pco2 to higher levels except when the patient’s inspired oxygen concentration is increased. It may also be raised above 11 kPa by the inhalation of carbon dioxide. In either event, a Pco2 in excess of 11 kPa may be considered an iatrogenic disorder. Figure 27.1 also shows the pattern of blood gas changes caused by shunting or pulmonary venous admixture (Chapter 8).
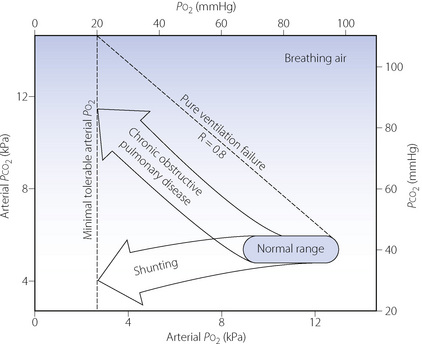
Fig. 27.1 Pattern of deterioration of arterial blood gases in chronic obstructive pulmonary disease and pulmonary shunting. The shaded area indicates the normal range of arterial blood gas partial pressures from 20 to 80 years of age. The oblique broken line shows the theoretical changes in alveolar Po2 and Pco2 resulting from pure ventilatory failure. In chronic obstructive pulmonary disease, the arterial Po2 is always less than the value that would be expected in pure ventilatory failure at the same Pco2 value. Discussion of shunting is to be found in Chapter 8 and further discussion of chronic obstructive pulmonary disease in Chapter 28.
In general, the arterial Po2 indicates the severity of respiratory failure (assuming that the patient is breathing air), while the Pco2 indicates the differential diagnosis between ventilatory failure and shunting as shown in Figure 27.1. In respiratory disease it is, of course, common for ventilatory failure and shunting to coexist in the same patient, and the relative contribution of each mechanism will determine whether type 1 or 2 respiratory failure develops.
Time Course of Changes in Blood Gas Tensions in Acute Ventilatory Failure
Although the upper arrow in Figure 27.1 shows the effect of established ventilatory failure on arterial blood gas tensions, short-term deviations from this pattern occur in acute ventilatory failure. This is because the time courses of changes of Po2 and Pco2 in response to acute changes in ventilation are quite different.
Body stores of oxygen are small, amounting to about 1550 ml while breathing air. Therefore, following a step change in the level of alveolar ventilation, the alveolar and arterial Po2 rapidly reach the new value and the half-time for the change is only 30 seconds (see page 205 and Figure 11.19). In contrast, the body stores of carbon dioxide are very large: of the order of 120 litres. Therefore, following a step change in the level of alveolar ventilation, the alveolar and arterial Pco2 only slowly attain the value determined by the new alveolar ventilation. Furthermore, the time course is slower following a reduction of ventilation than an increase (Figure 10.11) and the half-time of rise of Pco2 following a step reduction of ventilation is of the order of 16 minutes.
Causes of Ventilatory Failure1,2
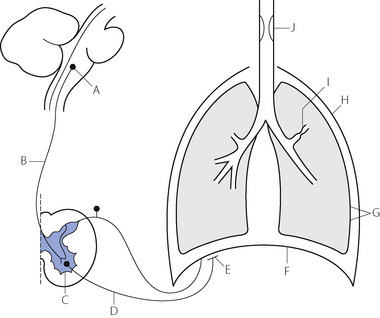
The causes of ventilatory failure may be conveniently considered under the headings of the anatomical sites where they arise. These sites are indicated in Figure 27.2. Lesions or malfunctions at sites A to E result in a reduction of input to the respiratory muscles. Dyspnoea may not be apparent and the diagnosis of ventilatory failure may be overlooked on superficial inspection of the patient. Lesions or malfunctions at sites G to J result in evident dyspnoea and no one is likely to miss the diagnosis of hypoventilation. The various sites will now be considered individually.
A wide variety of drugs may cause central apnoea or respiratory depression (page 77) and these include opioids, barbiturates and most anaesthetic agents, whether intravenous or inhalational. The respiratory neurones may also be affected by a variety of neurological conditions such as raised intracranial pressure, stroke, trauma or neoplasm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree