FIGURE 6.1. Pressure-volume relationships in collapsible tubes. During the “bending” phase of venous distension, large changes in volume are accommodated without significant changes in pressure. As the vein becomes elliptical and enters the “stretching” phase, pressures rise and increase further as the vein becomes circular.
(Adapted from Katz AI, Chen Y, Moreno AH. Flow through a collapsible tube: Experimental analysis and mathematical model. Biophysical J 1969;9:1261–1279.) Ref. (56)
Despite the importance of this reservoir capacity, the primary function of the venous circulation is to return blood to the heart. Lower extremity venous return is determined by the interaction of the dynamic pressure gradient between the lower extremities and the right atrium, respiratory-dependent changes in intra-abdominal and intrathoracic pressure (the respiratory pump), and the skeletal muscle pumps. In the resting supine position, the pressure is 12 to 18 mm Hg at the venous end of the capillary and falls steadily toward atrial pressures of 4 to 7 mm Hg.1 In the supine position, this dynamic pressure gradient is augmented by the effects of the respiratory pump. Although venous return is usually regarded as being augmented during inspiration, the situation is complex and depends on breathing mechanics.8 With diaphragmatic breathing, femoral venous return is abolished during inspiration and augmented during expiration (Fig. 6.2). This pattern is dictated by changes in intra-abdominal pressure rather than other factors such as constriction of the inferior vena cava at the diaphragmatic hiatus. In contrast, femoral venous blood flow is always positive during ribcage breathing, being slightly augmented during inspiration. The capacitance of the thigh veins appears to be the most important contributor to augmentation of venous flow induced by respiration.
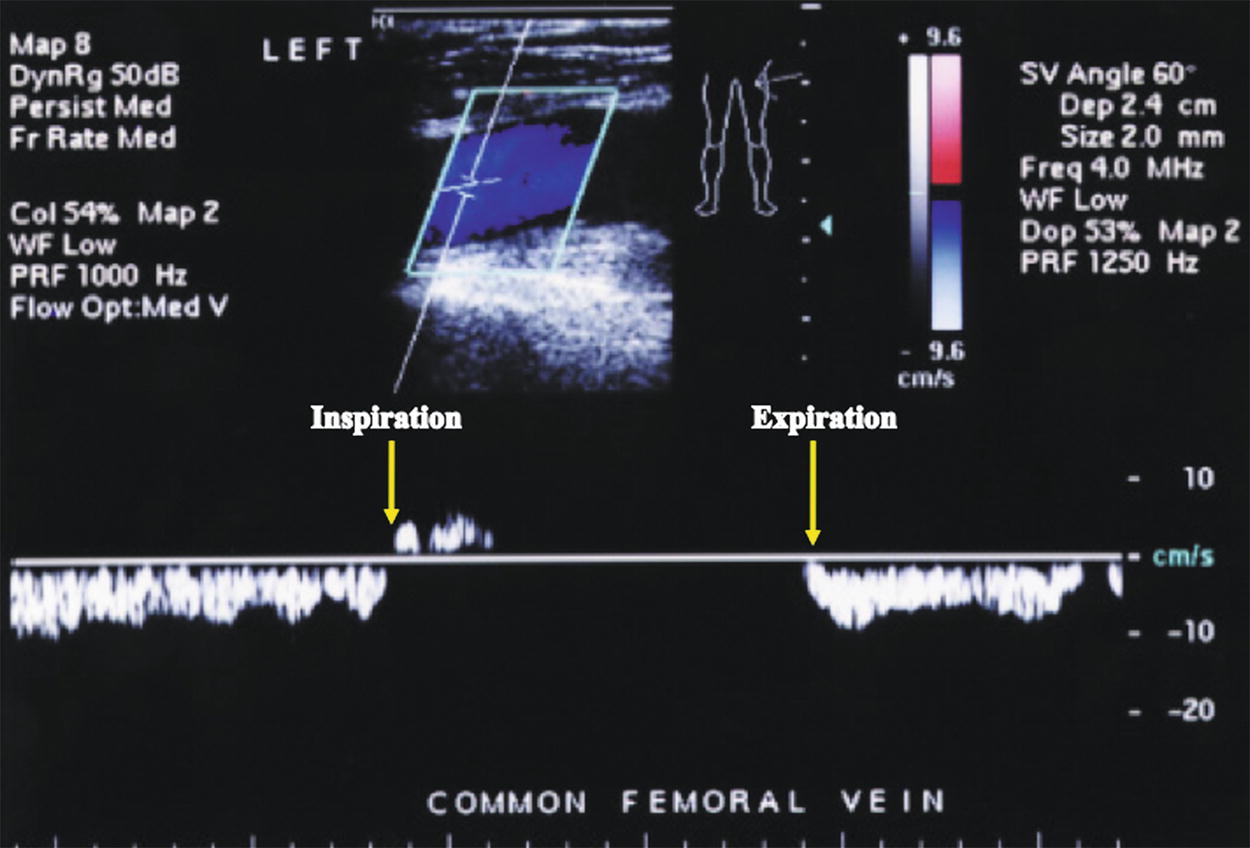
FIGURE 6.2. Common femoral Doppler waveform with quiet breathing in the supine position. With diaphragmatic breathing, unobstructed venous flow (displayed below the baseline) in the lower extremities decreases or ceases as abdominal pressure rises during inspiration and increases with expiration.
In the upright position, the physiological effects of gravity and hydrostatic pressure oppose venous return. Resting venous pressure in the upright position rises by approximately 0.8 mm Hg per centimeter below the right atrium and reaches 80 to 100 mm Hg at the ankle, varying with height, weight, and calf muscle volume.9,10 At rest, arterial inflow is balanced by the action of the respiratory pump, and pressure in the deep and superficial veins is equal. However, as arterial inflow rises with activity, effective venous return requires the interaction of the peripheral venous pumps and competent venous valves.11–15 Despite the importance of the skeletal muscle pumps, there continues to be some respiratory modulation of venous return during exercise.8
The valves function to divide the hydrostatic column of blood into segments and to insure unidirectional, antegrade venous flow. The superficial, deep, and most perforating veins contain bicuspid valves consisting of folds of endothelium supported by a thin layer of connective tissue. Although often believed to be oriented parallel to the skin, the angle between the free edges of adjacent valves averages 84 degrees in the great saphenous vein and 88 degrees in the femoral vein.16 The offsetting of adjacent valves likely induces rotational momentum and helical flow in the veins, a strategy that limits flow instability and decreases energy dissipation elsewhere in the circulation. The valve cups lie within the valve sinus, which is always wider than the adjacent vein. The valve sinus enlarges and assumes a more spherical shape at the time of valve closure.17 Distension of the valve sinus separates the commissures, tightening the edge of the cusps and resulting in valve closure.
Within the deep venous system, there are an average of 5 venous valves between the inguinal ligament and popliteal fossa, although the number varies from 2 to 9.18 These valves are usually 3 to 5 cm apart and tend to be consistently positioned at major venous junctions.16 Their arrangement is variable elsewhere, but in general, the inferior vena cava and common iliac veins have no valves; the external iliac and common femoral veins above the saphenofemoral junction have one valve at most; the femoral vein above the adductor canal has three or more valves; the distal femoral and popliteal veins have one or two valves; and the tibial/peroneal veins have numerous valves spaced at approximately 2 cm intervals.6,18 Although the muscle venous sinusoids are valveless, they frequently empty into profusely valved draining veins.18 Within the superficial venous system, a valve is present at the saphenofemoral junction in 94% to 100% of individuals19 and there are usually one or two subterminal valves within 2 cm of the terminal valve.4 The great saphenous vein usually has at least 6 valves, while the small saphenous vein has 7 to 10 closely spaced valves.6 Although the perforating veins of the calf generally direct flow from superficial to deep, most evidence suggest that only the larger perforating veins have valves.6,20
The valves of the lower extremity veins open and close at a cycle frequency of 34 to 36 per minute in the supine position and 19 to 20 per minute in the standing position.21 Knowledge regarding the mechanism of valve closure is largely derived from duplex observations of valves in response to nonphysiological provocative maneuvers such as Valsalva’s maneuver or distal calf compression. Under such conditions, valve closure is initiated by reversal of the normal, antegrade transvalvular pressure gradient during the relaxation or diastolic phase after calf muscle compression.22 As this pressure gradient reversal gradually increases, there is initially a short period of retrograde flow until the gradient becomes sufficient to cause valve closure. Rather than simple cessation of antegrade flow, valve closure under these artificial conditions requires retrograde flow at a velocity of at least 30 cm/s. Under such conditions, reverse flow duration is less than 0.5 seconds in 95% of normal valves.
Recent ultrasound observations under physiologic conditions, without augmentation or provocative maneuvers, suggest a different mechanism of valve closure.17,21 The valve cycle can be divided into four phases: opening, equilibrium, closing, and closed. At equilibrium, the valves are open but not apposed to the venous wall, causing a luminal narrowing of approximately 35% in comparison to the distal vein (Fig. 6.3A and B). This relative stenosis causes flow acceleration at the valve cusp with flow separation at the leading edge producing a vortex in the valve sinus. According to Bernoulli’s law, pressure decreases as velocity increases. Therefore, as luminal velocity increases at the end of the equilibrium phase, luminal pressure accordingly decreases, causing the valve to close when the vortex pressure behind the cusp exceeds the luminal pressure (Fig. 6.4). Among 12 normal subjects examined at rest in the upright position, flow reversal during valve closure occurred in only 1 subject. In this setting, cusp closure is initiated by an increase in forward flow velocity that is followed by a dilation of the valve sinus and subsequent valve closure. In distinct contrast to the mechanism of valve closure under the artificial conditions of a provocative maneuver, reverse flow is not necessary under normal physiologic conditions, and valve closure occurs despite ongoing antegrade flow.

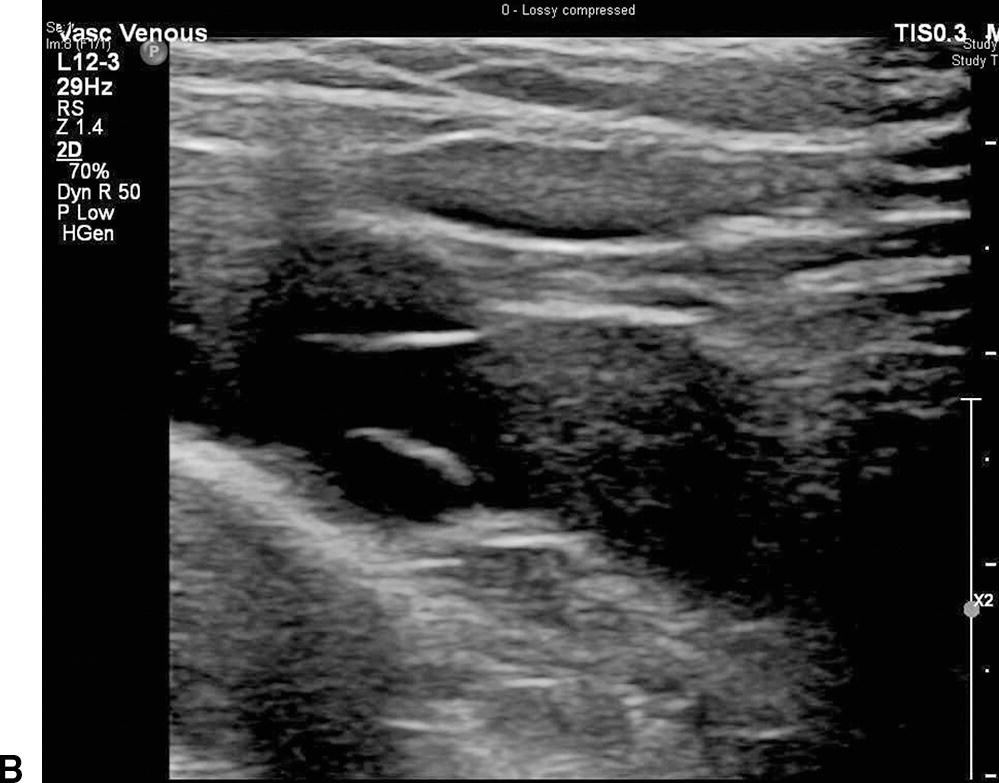
FIGURE 6.3. Cross-sectional (A) and longitudinal (B) B-mode images of a venous valve during the equilibrium phase of the valve cycle. During equilibrium, the valve cusps are open, but not fully opposed to the wall. This results in a relative stenosis at the leading edge of the valve cusps.
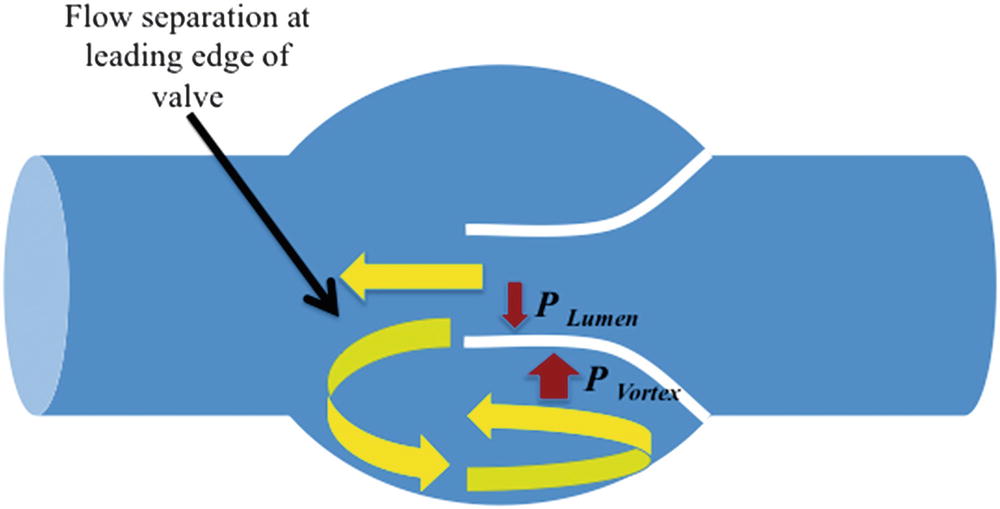
FIGURE 6.4. Mechanism of venous valve closure. The relative stenosis produced by the leading edge of the valve cusps leads to flow separation and vortex formation in the valve sinus. As luminal flow velocity changes at the end of the equilibrium phase of valve closure, vortex pressure exceeds luminal pressure resulting in valve closure.
(Adapted from Lurie F, Kistner RL, Eklof B, et al. Mechanism of venous valve closure and role of the valve in circulation: A new concept. J Vasc Surg 2003;38:955–961.) Ref. (21)
Approximately 90% of the venous return in the lower extremities is via the deep veins through the action of the foot, calf, and thigh muscles pumps.23 The action of these valved pumps is dependent on normally functioning muscle groups, a full range of joint mobility, and the deep fascia of the leg which constrains the muscles during contraction and allows high pressures to be generated within the muscular compartments.24 Among these, the calf muscle pump is the most important as it is the most efficient, has the largest capacitance, and generates the highest pressures.5,13 The normal calf pump ejects over 40% to 60% of the venous volume with a single contraction.12,13,25 The thigh muscle pump, which has an ejection fraction of only 15%, is thought to be substantially less important, while compression of the plantar venous plexus likely functions to prime the calf muscle pump.15
With contraction of the calf muscle (systole), pressure in the posterior compartment rises to as high as 250 mm Hg13 and the gastrocnemius and soleus veins are emptied of blood. With subsequent muscle relaxation (diastole), resting venous pressure is lowered as the valves prevent retrograde flow. Efficient function of the calf muscle pump requires not only the presence of competent valves but, as importantly, the presence of distal conduits, which have normal compliance and collapse as blood is ejected forward, thereby reducing pressure as the valves close.7 Pressure in the posterior tibial veins accordingly decreases from 80 to 100 mm Hg to less than 30 mm Hg. The degree to which venous pressure is reduced increases with a more rapid pace and decreases with restricted mobility of the knee and ankle.10 The reduction in deep venous pressure during calf muscle diastole favors flow from the superficial to the deep system through the perforating veins. In contrast to the ambulatory pressure reduction in the superficial and calf veins, pressure in the femoral and popliteal veins does not fall, producing an ambulatory pressure gradient between the thigh and calf veins of approximately 35 mm Hg.9 However, retrograde flow into the calf is prevented by competent valves, with capillary inflow causing a slow return of pressure in the calf veins to resting levels.
THE DETERMINANTS OF AMBULATORY VENOUS PRESSURE
The clinical manifestations of chronic venous insufficiency result from ambulatory venous hypertension, or the failure to adequately reduce venous pressure with activity (Fig 6.5). Ambulatory venous pressure (AVP) can be determined using a 21-gauge needle inserted into a dorsal foot vein to measure the response to 10 tiptoe movements, usually at a rate of 1 per second. The AVP is the lowest pressure achieved at the end of this exercise. Under normal circumstances, lower extremity venous pressure is reduced from approximately 100 mm Hg (depending on individual height) to a mean of 22 mm Hg within 7 to 12 steps.14 Chronic venous insufficiency is associated with elevated AVPs as well as shortened refilling times after exercise ceases. The severity of chronic venous disease is closely related to the magnitude of venous hypertension. Ulceration usually does not occur at AVPs of less than 30 mm Hg, while the incidence is 100% at pressures greater than 90 mm Hg.26
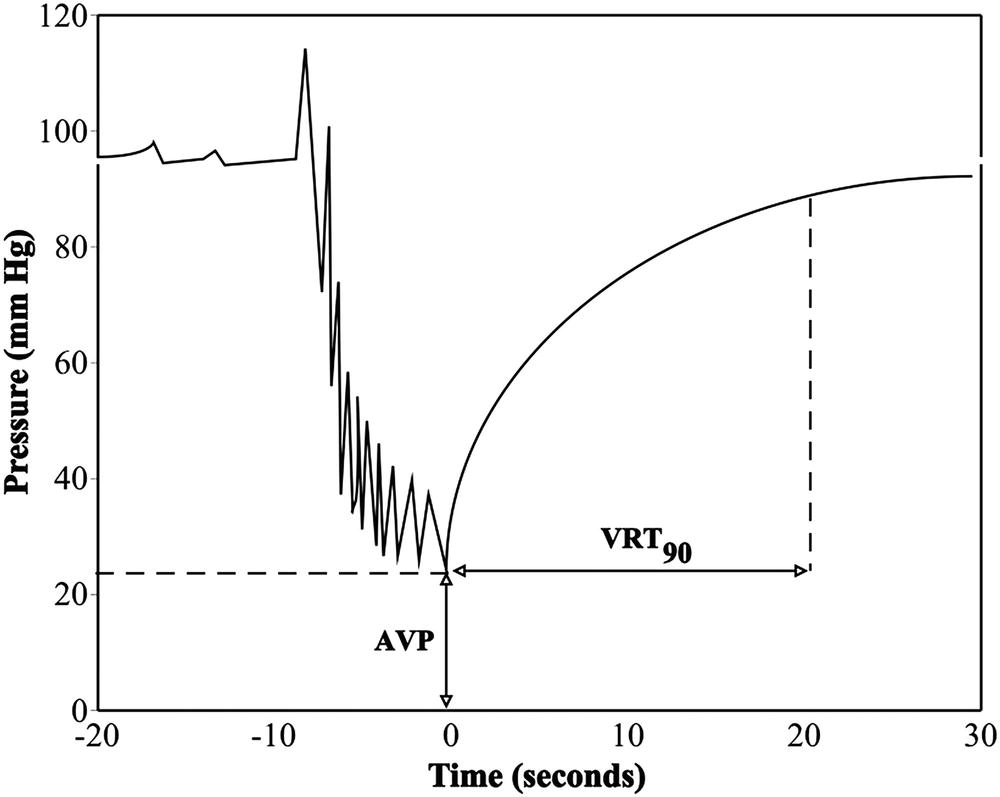
FIGURE 6.5. Ambulatory venous pressure measured from cannulation of a dorsal foot vein. In the normal limb, pressure declines with plantar flexion. Ambulatory venous pressure (AVP) at the end of ten tiptoe maneuvers is less than 30 mm Hg in normal limbs. The time required for return to baseline is measured as the 90% venous refilling time (VRT). Limbs with hemodynamically significant reflux have an elevated AVP and rapid 90% VRT.
Although commonly attributed to venous reflux, ambulatory venous hypertension may result from failure of any component of the lower extremity venous system—valvular incompetence, venous outflow obstruction, skeletal muscle pump failure, or limited range of ankle motion.9,27,28 Reflux, or pathologic retrograde flow, occurs when the valves are absent or rendered incompetent by degenerative processes (primary venous disease) or an episode of DVT (secondary venous disease). Under these circumstances, retrograde flow during calf muscle relaxation prevents the usual reduction in pressure and rapid venous refilling occurs. While reflux in asymptomatic and mildly symptomatic patients is usually isolated and segmental, that in patients with skin changes and ulceration is usually multisegmental and frequently involves the deep, superficial, and perforating veins.29 Approximately two-thirds of patients with ulcers have multisystem venous disease.30 Although reflux in superficial and distal deep veins appears to be important in the pathogenesis of venous ulceration, it is likely the axial reflux volume, rather than the precise localization that is of greatest hemodynamic importance.9
Despite its importance, reflux is hardly the sole determinant of ambulatory venous hypertension. For any given volume of reflux, AVP will be higher in the presence of venous obstruction.31 Postthrombotic limbs with edema, hyperpigmentation, or ulceration are more likely to have a combination of reflux and residual obstruction than either abnormality alone (Table 6.1).31,32 However, despite these observations, reflux has, in the past, often been regarded as more important than obstruction. This is likely related to the observation that the hemodynamic effects of chronic venous obstruction are difficult to quantify. Although acute venous obstruction can be detected using a variety of plethysmographic techniques, chronically obstructed limbs have a larger residual volume and are well collateralized, often with near normal venous outflow. Thus, there are no reliable physiologic tests for diagnosis of a hemodynamically significant chronic venous obstruction.
TABLE 6.1 Ultrasound Findings in Asymptomatic and Postthrombotic Limbs
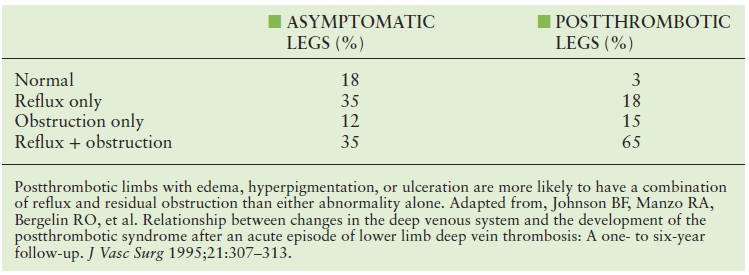
Postthrombotic limbs with edema, hyperpigmentation, or ulceration are more likely to have a combination of reflux and residual obstruction than either abnormality alone. Adapted from, Johnson BF, Manzo RA, Bergelin RO, et al. Relationship between changes in the deep venous system and the development of the postthrombotic syndrome after an acute episode of lower limb deep vein thrombosis: A one- to six-year follow-up. J Vasc Surg 1995;21:307–313.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


