Venous Ablation Procedures
Kathleen D. Gibson
Aaron Ebert
Venous insufficiency is arguably the most common condition evaluated in an outpatient vascular laboratory setting. Varicose veins and deep venous insufficiency cause leg fatigue, pain, and swelling in millions of patients and are two of the most common conditions treated by vascular surgeons. In Western populations, 20% to 34% of women and 7% to 28% of men have visible varicose veins.1,2,3 The prevalence of varicose veins increases significantly with age.4 Incompetence of the great saphenous vein (GSV) is the most common cause of varicose veins; however, the small saphenous vein (SSV) shows valvular incompetence in up to 20% of affected limbs.5
The most common treatment for truncal saphenous incompetence historically was high ligation and stripping. This surgical procedure required general or spinal anesthesia in a hospital-based setting. With the advent of the less invasive endovenous thermal ablation techniques utilizing radiofrequency (RF)6 and laser (EVLT)7,8 energy sources, patients are now treated with a relatively quick in-office procedure under local anesthesia. Advances in venous imaging and endovascular techniques made the application of this technology clinically successful, and endovenous techniques are now essentially the standard of care.
Ultrasound-guided foam sclerotherapy (UGFS) has been extensively used in Europe to treat both saphenous vein incompetence and tributary incompetence.9,10,11 The use of UGFS to treat superficial venous insufficiency in the United States is increasingly being practiced,12 and interdisciplinary quality improvement guidelines for the use of physician-created foam have been developed.13 Phase III clinical trials using proprietary endovenous microfoam (BTG, West Conshohocken, PA) to treat GSV incompetence have been completed, and a new drug application has been recently submitted to the FDA.14 Highly accurate ultrasound imaging is critical to the performance of successful UGFS. Ultrasound is used to guide venous access and to follow the progress of the foamed agent within the vein to ensure that it effectively treats the intended vein target and does not reach unintended veins in any significant volume.
A number of emerging technologies rely on duplex ultrasound imaging for safe and effective treatment of truncal superficial venous insufficiency. These include mechanical-chemical ablation (MOCA, Clarivein, Vascular Insights, Madison, CT),15 steam ablation (Cermavein, Cerma, Archamps, France),16 and ablation using cyanoacrylate glue (Venaseal, Sapheon Inc., Morrisville, NC).17 All endovenous techniques require duplex ultrasound imaging for their successful application and therefore offer a unique opportunity to partner vascular technologists with physicians in the treatment of venous insufficiency. In our practice, each step in treating patients with varicose veins—from pretreatment imaging to treatment and postoperative follow-up—requires a close and rewarding partnership with the vascular laboratory.
PRETREATMENT EVALUATION
Preoperative planning is the key to successful treatment of varicose veins using any of the ablation techniques. Patients first undergo a thorough history and physical examination. They are queried regarding any previous vein procedures (sclerotherapy, ablation, or stripping), history of deep venous thrombosis (DVT), superficial thrombophlebitis, or personal or family history of thrombophilia. This information is passed on to the vascular laboratory prior to duplex scanning and can guide the vascular technologist on what to look out for while scanning. Patients with recurrent varicose veins after procedures such as stripping often do not have straightforward venous anatomy and may require additional time for their study. Because care must also be taken in performing venous procedures on patients with peripheral arterial disease, pedal pulses should always be palpated during the initial physical examination. If these pulses are abnormal, the vascular laboratory may be called upon to perform a concomitant arterial evaluation.
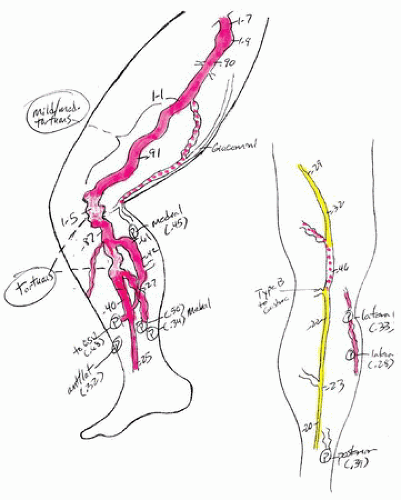
A meticulous duplex ultrasound examination is the next step in preprocedure planning. A detailed “roadmap” of incompetent saphenous trunks and other sources of varicose veins is important. Failure to address nonsaphenous sources of varicosities such as perforators, accessory branches, and pelvic veins can lead to immediate or early treatment failure and patient dissatisfaction (see Chapter 25). In our practice, along with the formal report, the vascular technologist draws a “map” of the varicose veins including the diameters of the GSV and the SSV and the presence of any relevant accessory branches and perforator veins (Fig. 29.1). Incompetent anterolateral and posteromedial branches from the GSV are common, and if untreated, these may be associated with an unsatisfactory clinical result. It is not uncommon for the GSV or the SSV to terminate in the distal thigh or calf, with continuation as a branch above the superficial fascia. Such a branch is referred to not as the GSV or the SSV but as a tributary.18 Incompetent tributaries above the fascial layer in any part of the limb should be noted. Depth of the veins under the skin has potential ramifications for endovenous treatment. “Shallow” veins require more local anesthetic, and patients often have more discomfort after the procedure. Some suprafascial veins are close enough to the skin to preclude thermal ablation, and other techniques such as ambulatory phlebectomy or UGFS can be considered
on these veins. An assessment of the deep system is particularly important in patients with a history of DVT, edema, skin changes, or ulceration or in young patients with severe varicosities and suspicion for Klippel-Trenaunay syndrome.
on these veins. An assessment of the deep system is particularly important in patients with a history of DVT, edema, skin changes, or ulceration or in young patients with severe varicosities and suspicion for Klippel-Trenaunay syndrome.
In patients presenting with groin, medial thigh, and upper posterior thigh varicose veins, a pelvic source from an incompetent internal iliac vein branch should be considered (Fig. 29.2). This varicose vein pattern is almost invariably seen only in female patients, and it is most often present during or after pregnancy. It is common in these cases that the terminal valve of the GSV is competent, and the GSV becomes incompetent when a varicose vein branch from the pelvic veins empties into it. When performing a varicose vein study, if the GSV is incompetent and yet the terminal valve is competent, an alternative source for the reflux should be investigated such as a perforator vein, a pelvic branch, or a branch from an incompetent accessory vein.
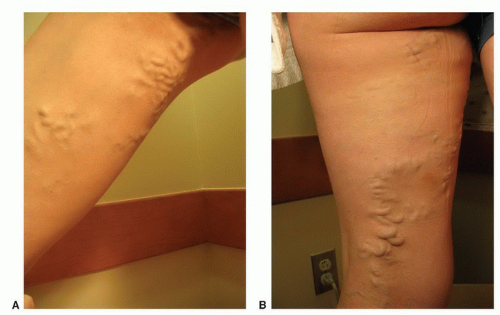 FIGURE 29.2. A, B, Nonsaphenous sources of varicose veins. A pelvic source of reflux should be considered in patients presenting with groin, medial thigh, or upper posterior thigh varicose veins. |
Precise near-field resolution is the most important feature for diagnostic imaging and treatment of varicose veins. In our practice, we use a GE Logic 9 machine with a 12-MHz “hockey stick” probe and a 10-MHz linear probe for preoperative mapping. Documentation of deep and superficial venous incompetence, as well as the presence of any clinically significant refluxing perforator veins, is noted.
TREATMENT
After the surgeon is provided with a report and a detailed vein map, a treatment plan can be made. Endovenous ablation techniques can be used to treat the GSV, SSV, accessory branches, and even perforator veins. An incompetent anterolateral branch from the saphenofemoral junction (SFJ) is a common cause of lateral thigh and calf varicosities, with the varicosities often terminating in an incompetent lateral calf perforator. Depending on the distribution and size of side branches, adjunctive treatments such as microphlebectomy, perforator ligation, and UGFS can be considered and performed at the same time as the EVLT or RF procedure.
The importance of good duplex imaging in ensuring the safety and efficacy of endovenous techniques cannot be overstated. Each step of the procedure from initial access of the vein to adequate tumescent anesthesia to proper placement of the laser or RF catheter requires accurate imaging. In many practices, the treating physician holds the ultrasound probe with one hand and accesses the vein with the other, and a vascular
technologist is either not involved or simply adjusts the controls on the ultrasound machine. Our team includes a registered vascular technologist (RVT) who holds the probe and plays an integral role in the procedure. We find this two-person approach increases the speed and efficiency of the procedure, and we also find it to be less ergonomically fatiguing for the surgeon. This team approach has been very rewarding in our practice, increasing collegiality between the RVT and physician, as well as improving the diagnostic skills of our vascular technologists. Being an active member of the treatment team helps the vascular technologist to think “like a surgeon” during venous examinations—anticipating what information will be needed for successful treatment of the venous abnormalities.
technologist is either not involved or simply adjusts the controls on the ultrasound machine. Our team includes a registered vascular technologist (RVT) who holds the probe and plays an integral role in the procedure. We find this two-person approach increases the speed and efficiency of the procedure, and we also find it to be less ergonomically fatiguing for the surgeon. This team approach has been very rewarding in our practice, increasing collegiality between the RVT and physician, as well as improving the diagnostic skills of our vascular technologists. Being an active member of the treatment team helps the vascular technologist to think “like a surgeon” during venous examinations—anticipating what information will be needed for successful treatment of the venous abnormalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree