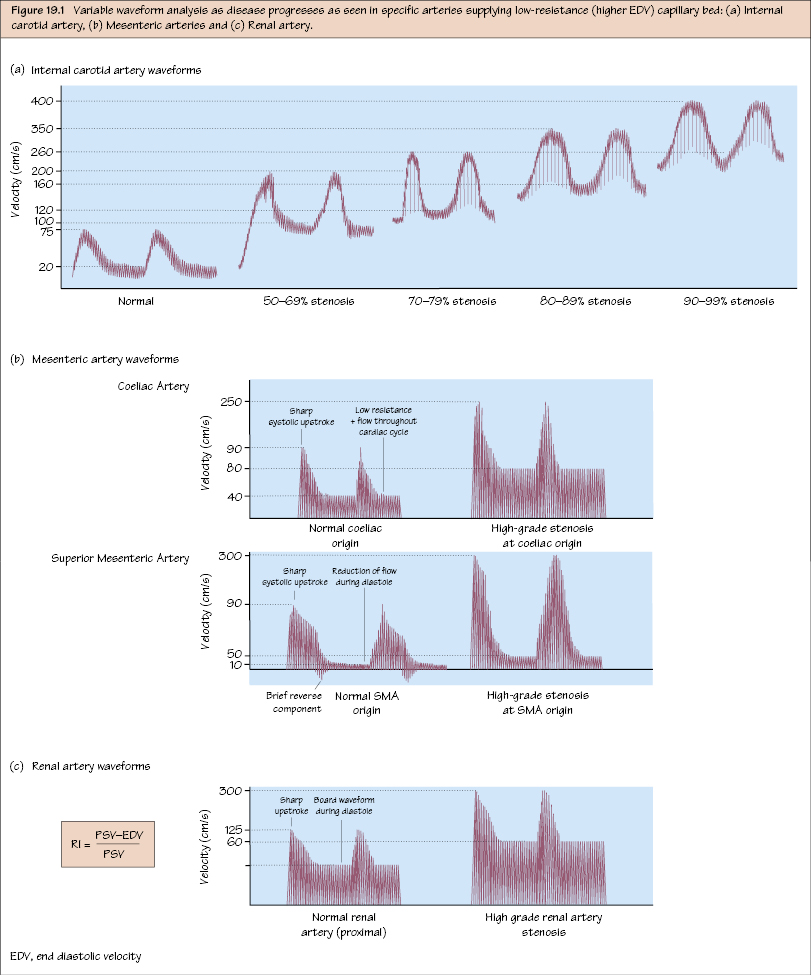
Vascular Ultrasound III: Specific Parameters As a ‘rule of thumb’ the mean velocity is 100 cm/s (±30–50%) including the aorta (peak systolic velocity [PSV] 100–150 cm/s) with triphasic morphology. There is a gradual decrease in velocities on moving distally down the arterial tree (loss of energy and increasing number of branches). The normal ratio is <2.0 and critical stenosis is defined as >2.5–3.0 (≥50% stenosis). Distal to a stenosis, there is loss of the reverse-flow component of the waveform with post-stenotic turbulence (spectral broadening). In addition, tandem lesions may have a greater magnitude effect than an isolated critical lesion (i.e. critical limb ischaemia due to multiple sub-critical lesions). Duplex examination includes simultaneous provocative testing (positional changes in the arm and head) if thoracic outlet syndrome is suspected. Lesions in the SCA are more difficult to visualise because of the presence of the clavicle. The flow in the ipsilateral vertebral artery should also be assessed for evidence of reversed flow (i.e. steal syndrome). The waveform is normally triphasic at rest, but with high diastolic flow rates on vasodilatation (e.g. post-exercise). The normal PSV is 80–120 cm/s for the SCA and axillary artery, 50–100 cm/s for the brachial and PSV 40–90 cm/s for the radial and ulnar arteries. The criteria for grading critical stenosis in the upper limb is not well established because of its resistance to ischaemia (profunda brachii) with patients often remaining asymptomatic. However, a doubling of the PSV corresponds to a 50% lumen reduction and may be considered haemodynamically significant (i.e. PSV > 180 cm/s). The carotid has high flow into a low resistance bed and therefore there is a significant amount of flow in diastole. Therefore, end-diastolic velocities (EDV) are also important along with PSV in assessments. The normal PSV and EDV in the ICA is <125 cm/s and <40 cm/s respectively with an ICA/common carotid artery (CCA) PSV ratio <2.0. A 50–69% stenosis corresponds to PSV 125–230 cm/s, EDV 40–100 cm/s and a ratio of 2.0–4.0. Surgery (+BMT) has superior long-term stroke prevention rates for critical stenosis (>70%): High flow into low resistance capillary bed and therefore there is higher diastolic flow and EDVs are also relevant. Flow varies enormously from fasting to post-prandial (especially SMA). Coeliac axis. Sharp systolic upstroke (narrow systolic window) with a very low resistance pattern (antegrade flow through the cardiac cycle). Typical PSV <125 cm/s. A significant stenosis (>70%): PSV > 200 cm/s, EDV ≥ 55 cm/s, mesenteric/aortic ratio >3.0. In addition, reversed flow in the common hepatic artery is always indicative of severe coeliac stenosis or occlusion. SMA (fasting). Sharp upstroke (narrow systolic window) with triphasic morphology. There is a brief reverse-flow phase and little or no flow at end of arterial cycle. Typical PSV <125 cm/s. A significant stenosis (≥70%): PSV >275 cm/s; mesenteric/aortic ratio >3.0 and EDV ≥ 45 cm/s. High flow into a low resistance capillary bed and therefore there is significant blood flow during diastole (waveforms more pulsatile proximally and dampen distally). The normal renal systolic velocity is 100–150 cm/s. A significant stenosis is PSV > 180–200 cm/s or renal-aortic ratio (RAR) ≥ 3.5. PSV > 400 cm/s corresponds to a 90% stenosis. In addition, the resistance index (RI) measured in an interlobar artery reflects diastolic flow and is calculated as:
Lower Limb Assessment
Upper Limb Arterial Assessment
Carotid Artery Assessment
Mesenteric Vessel Assessment
Renal Artery Assessment
Vascular Ultrasound III: Specific Parameters
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


