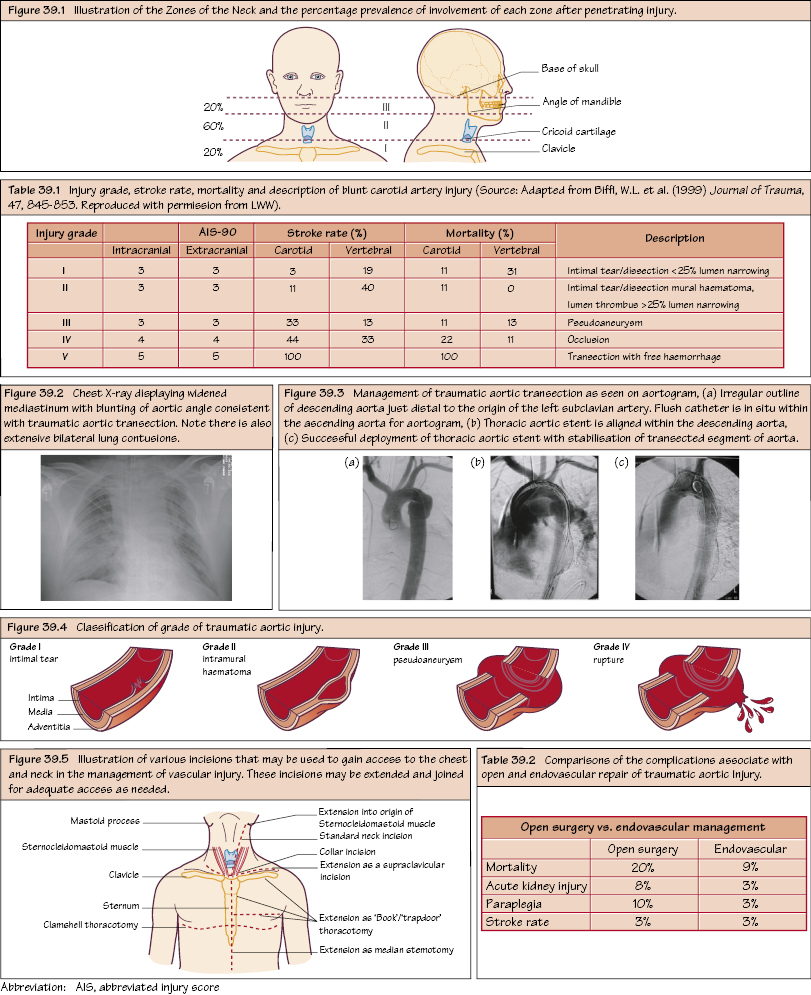
Vascular Trauma: Neck and Chest Carotid and subclavian artery injuries (blunt or penetrating) account for less than 2% of vascular trauma, but carry a high mortality and morbidity. The neck is divided into three distinct anatomical zones but more than one zone may be involved. All patients should be managed initially as per the advanced trauma life support (ATLS) guidelines. Blunt injury is associated with multiple competing injuries requiring treatment. If the patient is physiologically well, then a CT with contrast (arterial and portal venous phase) is the investigation of choice. These carry a high mortality and stroke rate and are associated with a high incidence of c-spine and head injuries (contributing to the high mortality and morbidity). Often the neurological injury has already occurred by the time of presentation (head trauma or embolic stroke).
Carotid, Vertebral and Subclavian Vessels
Blunt Carotid Trauma
Management
Penetrating Carotid Trauma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


