Vascular lung disorders
Vascular lung disorders affect the vascular structures of the lungs. Normal pulmonary vasculature is a low-pressure, lowresistance system. It includes pulmonary arteries, pulmonary veins, pulmonary capillaries, pulmonary lymphatics, and bronchial circulation.
Conditions that affect any of these vascular components can result in a vascular lung disorder and compromised respiratory function.
COR PULMONALE
The World Health Organization defines chronic cor pulmonale as “hypertrophy of the right ventricle resulting from diseases affecting the function or the structure of the lungs, except when these pulmonary alterations are the result of diseases that primarily affect the left side of the heart or of congenital heart disease.” Invariably, cor pulmonale follows some disorder of the lungs, pulmonary vessels, chest wall, or respiratory control center. For example, chronic obstructive pulmonary disease (COPD) produces pulmonary hypertension, which leads to right ventricular hypertrophy and right-sided heart failure. Because cor pulmonale usually occurs late during the course of COPD and other irreversible diseases, the prognosis is generally poor.
About 85% of patients with cor pulmonale have COPD, and 25% of patients with COPD eventually develop cor pulmonale.
Other respiratory disorders that produce cor pulmonale include:
chronic mountain sickness (living at high altitudes)
loss of lung tissue after extensive lung surgery
obesity hypoventilation syndrome (pickwickian syndrome) and upper airway obstruction
obstructive lung diseases—for example, bronchiectasis and cystic fibrosis
pulmonary vascular diseases—for example, recurrent thromboembolism, primary pulmonary hypertension, schistosomiasis, and pulmonary vasculitis
respiratory insufficiency without pulmonary disease—for example, in chest wall disorders such as kyphoscoliosis, neuromuscular incompetence resulting from muscular dystrophy and amyotrophic lateral sclerosis, polymyositis, and spinal cord lesions above the sixth cervical vertebra
restrictive lung diseases—for example, pneumoconiosis, interstitial pneumonitis, scleroderma, and sarcoidosis.
Cor pulmonale accounts for about 25% of all types of heart failure. It’s most common in areas of the world where the incidence of cigarette smoking and COPD is high; cor pulmonale affects middle-age to elderly men more commonly than women, but its incidence in women is increasing. In children, cor pulmonale may be a complication of cystic fibrosis, hemosiderosis, upper airway obstruction, scleroderma, extensive bronchiectasis, neurologic diseases affecting respiratory muscles, or abnormalities of the respiratory control center.
Pathophysiology
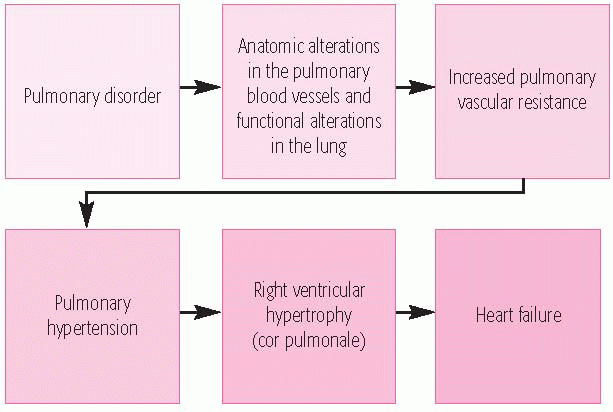
Pulmonary capillary destruction and pulmonary vasoconstriction (usually secondary to hypoxia) reduce the area of the pulmonary vascular bed. Thus, pulmonary vascular resistance is increased, causing pulmonary hypertension. To compensate for the extra work needed to force blood through the lungs, the right ventricle dilates and hypertrophies. In response to low oxygen content, the bone marrow produces more red blood cells, causing erythrocytosis. When hematocrit exceeds 55%, blood viscosity increases, further aggravating pulmonary hypertension and increasing the hemodynamic load on the right ventricle.
Right-sided heart failure is the result. (See What happens in cor pulmonale.)
Right-sided heart failure is the result. (See What happens in cor pulmonale.)
Complications
Right- and left-sided heart failure
Hepatomegaly
Edema
Ascites
Pleural effusions
Thromboembolism
Assessment findings
As long as the heart can compensate for the increased pulmonary vascular resistance, clinical features reflect the underlying disorder and occur mostly in the respiratory system.
They include chronic productive cough, exertional dyspnea, wheezing, fatigue, and weakness.
Progression of cor pulmonale is associated with dyspnea (even at rest) that worsens on exertion, tachypnea, orthopnea, edema, weakness, and right upper quadrant discomfort.
Signs of cor pulmonale and right-sided heart failure include dependent edema, distended jugular veins, prominent parasternal or epigastric cardiac impulse, hepatojugular reflux, ascites, tachycardia, and an enlarged, tender liver.
Decreased cardiac output may cause a weak pulse and hypotension.
Chest examination yields various findings, depending on the underlying cause of cor pulmonale.
In COPD, auscultation reveals wheezing, rhonchi, and diminished breath sounds.
When the disease is secondary to upper airway obstruction or damage to central nervous system respiratory centers, chest findings may be normal, except for a right ventricular lift, gallop rhythm, and loud pulmonic component of S2.
Tricuspid insufficiency produces a pansystolic murmur heard at the lower left sternal border; its intensity increases on inspiration, distinguishing it from a murmur resulting from mitral valve disease.
A right ventricular early murmur that increases on inspiration can be heard at the left sternal border or over the epigastrium.
A systolic pulmonic ejection click may also be heard.
Alterations in level of consciousness may occur.
Diagnostic test results
Arterial blood gas (ABG) analysis shows decreased partial pressure of arterial oxygen (PaO2) (typically less than 70 mm Hg and usually no more than 90 mm Hg on room air).
Chest X-ray shows large central pulmonary arteries and suggests right ventricular enlargement by rightward enlargement of the heart’s silhouette on an anterior chest X-ray.
Echocardiography or angiography demonstrates right ventricular enlargement; echocardiography can estimate pulmonary
artery pressure (PAP) while also ruling out structural and congenital lesions.
Electrocardiogram frequently shows arrhythmias, such as premature atrial and ventricular contractions and atrial fibrillation during severe hypoxia; it may also show right bundlebranch block, right axis deviation, prominent P waves and inverted T waves in right precordial leads, and right ventricular hypertrophy.
PAP measurements show increased right ventricular and pulmonary artery pressures, stemming from increased pulmonary vascular resistance. Right ventricular systolic and pulmonary artery systolic pressures will exceed 30 mm Hg. Pulmonary artery diastolic pressure will exceed 15 mm Hg.
Pulmonary function tests show results consistent with the underlying pulmonary disease. Hematocrit is typically greater than 50%.
Treatment
Treatment of cor pulmonale is designed to reduce hypoxemia, increase the patient’s exercise tolerance and, when possible, correct the underlying condition.
In addition to bed rest, treatment may include:
antibiotics when respiratory infection is present; culture and sensitivity of sputum specimens aid in selection of antibiotics
anticoagulants, as indicated, to reduce the risk of thromboembolism
low-sodium diet, restricted fluid intake, and diuretics such as furosemide [Lasix] to reduce edema
oxygen by mask or cannula in concentrations ranging from 24% to 40%, depending on PaO2, as necessary; in acute cases, therapy may also include mechanical ventilation; patients with underlying COPD generally shouldn’t receive high concentrations of oxygen because of possible subsequent respiratory depression
phlebotomy to reduce the red blood cell count if polycythemia is present
COR PULMONALE TEACHING TOPICS
Make sure the patient understands the importance of maintaining a low-sodium diet, weighing himself daily, and watching for increased edema. Teach him to detect edema by pressing the skin over a shin with one finger, holding it for a second or two, then checking for a finger impression. Increased weight, increased edema, or respiratory difficulty should be reported to the practitioner.
Instruct the patient to plan for frequent rest periods and to perform breathing exercises regularly.
If the patient needs supplemental oxygen therapy at home, refer him to an agency that can help obtain the required equipment and, as necessary, arrange for follow-up examinations.
If the patient has been placed on anticoagulant therapy, emphasize the need to watch for bleeding (epistaxis, hematuria, bruising) and to report signs to the physician. Also encourage him to return for periodic laboratory tests to monitor International Normalized Ratio, platelet count, hematocrit, hemoglobin level, and prothrombin time.
Because pulmonary infection commonly exacerbates chronic obstructive pulmonary disease and cor pulmonale, tell the patient to watch for and immediately report early signs of infection, such as increased sputum production, change in sputum color, increased coughing or wheezing, chest pain, fever, fatigue, and tightness in the chest. Tell the patient to avoid crowds and anyone known to have pulmonary infections, especially during the flu season. Patients should receive Pneumovax and an annual influenza vaccine.
Warn the patient to avoid substances that may depress the ventilatory drive, such as sedatives and alcohol.
potent pulmonary artery vasodilators (such as diazoxide [Proglycem], nitroprusside [Nitropress], hydralazine [Apresoline], angiotensin-converting enzyme inhibitors, calcium channel blockers, or prostaglandins) in primary pulmonary hypertension.
Depending on the underlying cause, some variations in treatment may be indicated. For example, a tracheotomy may be necessary if the patient has an upper airway obstruction. Steroids may be used in patients with a vasculitis autoimmune phenomenon or acute exacerbations of COPD.
Nursing interventions
Plan the diet carefully with the patient and the staff dietitian. Because the patient may lack energy and tire easily when eating, plan for small, frequent meals rather than three heavy ones.
Prevent fluid retention by limiting the patient’s fluid intake to 1 to 2 qt (1 to 2 L)/day and providing a low-sodium diet.
Monitor serum potassium levels closely if the patient is receiving diuretics.
Reposition bedridden patients often to prevent atelectasis.
Provide meticulous respiratory care, including oxygen therapy and, for COPD patients, pursed-lip breathing exercises. Periodically measure ABG levels and watch for signs of impending respiratory failure, such as change in pulse rate, labored respirations, changes in mental status, and fatigue. (See Cor pulmonale teaching topics.)
PULMONARY EDEMA
Pulmonary edema is a common complication of cardiac disorders. It’s marked by an accumulation of fluid in extravascular spaces of the lung. The disorder may occur as a chronic condition, or it may develop quickly and rapidly become fatal.
Pulmonary edema usually results from left-sided heart failure caused by arteriosclerotic, cardiomyopathic, hypertensive, or valvular heart disease. (See How pulmonary edema develops, page 304.)
Other factors that may predispose the patient to pulmonary edema include:
barbiturate or opiate poisoning
heart failure
infusion of excessive volumes of I.V. fluids or an overly rapid infusion
impaired pulmonary lymphatic drainage (from Hodgkin’s disease or obliterative lymphangitis after radiation)
inhalation of irritating gases
mitral stenosis and left atrial myxoma (which impair left atrial emptying)
pneumonia
pulmonary venoocclusive disease.
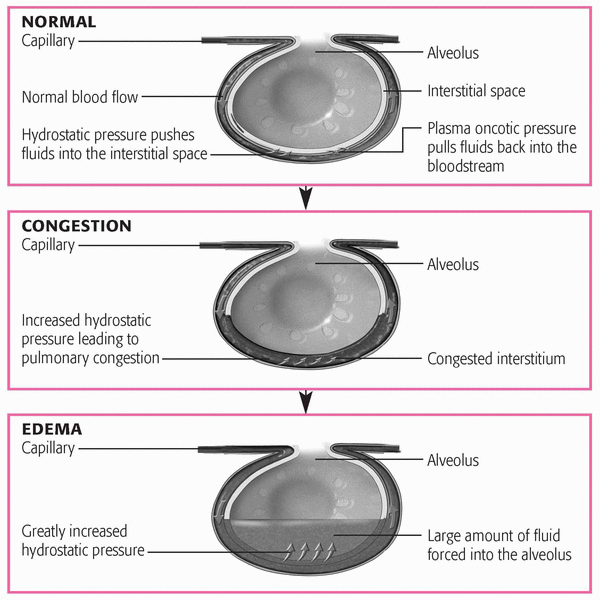
Normally, pulmonary capillary hydrostatic pressure, capillary oncotic pressure, capillary permeability, and lymphatic drainage are in balance. When this balance changes or the lymphatic drainage system is obstructed, fluid infiltrates into the lung and pulmonary edema results. If pulmonary capillary hydrostatic pressure increases, the compromised left ventricle requires increased filling pressures to maintain adequate cardiac output. These pressures are transmitted to the left atrium, pulmonary
veins, and pulmonary capillary bed, forcing fluids and solutes from the intravascular compartment into the interstitium of the lungs. As the interstitium overloads with fluid, fluid floods the peripheral alveoli and impairs gas exchange.
veins, and pulmonary capillary bed, forcing fluids and solutes from the intravascular compartment into the interstitium of the lungs. As the interstitium overloads with fluid, fluid floods the peripheral alveoli and impairs gas exchange.
If colloid osmotic pressure decreases, the hydrostatic force that regulates intravascular fluids (the natural pulling force) is lost because there’s no opposition. Fluid flows freely into the interstitium and alveoli, impairing gas exchange and leading to pulmonary edema.
Blockage of the lymph vessels can result from compression by edema or tumor fibrotic tissue and by increased systemic venous pressure. Hydrostatic pressure in the large pulmonary veins increases, the pulmonary lymphatic system can’t drain correctly into the pulmonary veins, and excess fluid moves into the interstitial space. Pulmonary edema then results from fluid accumulation.
Capillary injury, such as occurs in acute respiratory distress syndrome (ARDS) or with inhalation of toxic gases, increases capillary permeability. The injury causes plasma proteins and water to leak out of the capillary and move into the interstitium, increasing the interstitial oncotic pressure, which is normally low. As interstitial oncotic pressure begins to equal capillary oncotic pressure, the water begins to move out of the capillary and into the lungs, resulting in pulmonary edema.
Complications
Respiratory acidosis
Metabolic acidosis
Cardiac or respiratory arrest
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree