Fig. 14.1
Traditionally defined zones of the neck
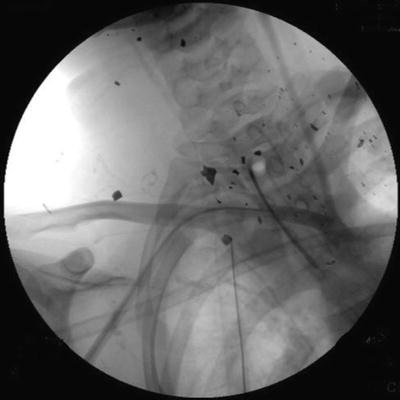
Fig. 14.2
This blast injury with multiple fragments bilaterally in zones I and II defies traditional classification
Initial Assessment
As with any significant trauma, initial assessment should proceed according the Advanced Trauma Life Support guidelines (the A, B, Cs) [5]. Patients with neck injuries can decompensate quickly, and the location of the injury puts the airway uniquely at risk. Therefore, securing an airway is essential in these patients, and there should be a very low threshold for intubation. Unfortunately, intubation can be difficult in a patient with a large neck hematoma, and advanced airway management techniques including early cricothyroidotomy or tracheostomy may be required.
While active arterial bleeding or an expanding hematoma can be dramatic, assessment for vascular injuries only occurs during the “C” portion of the primary survey. After the airway is secure, an immediate determination must be made as to whether the patient’s injuries require urgent surgical attention. If the patient has any hard signs of vascular injury (Table 14.1), prompt surgical intervention will be required, and the remainder of the evaluation can proceed on that basis.
Table 14.1
Hard signs of injury
Active bleeding with signs of hemorrhagic shock |
Expanding hematoma |
Bruit or thrill |
Pulse defect |
Evolving stroke |
Diagnostic Imaging
The evaluation and management of the stable patient with a penetrating neck injury has evolved over the last couple of decades; however, these cases can still generate some controversy. Historically, the potential for a devastating missed vascular injury was the primary focus, and any Zone II penetrating injury deep to the platysma mandated prompt surgical exploration. Some studies reported injuries in as many as 30 % of patients undergoing surgery, and given the relatively limited morbidity of a neck incision, diagnostic exploration remains a safe course of action [6]. The drawback of mandatory neck exploration is a high rate of nontherapeutic surgery. One study reported a negative neck exploration rate of 98 % in asymptomatic patients [7]. In the mid-1990s, many trauma centers began using a selective approach to Zone II penetrating injuries. Stable patients with minimal symptoms may benefit from additional diagnostic imaging to determine if surgery is necessary. Catheter angiography continues to be the gold standard for detecting arterial pathology, with a sensitivity and specificity for major injuries approaching 100 % [8]. Angiography can accurately evaluate for injuries in all zones of the neck and has the advantage of being therapeutic as well as diagnostic. In the traditional approach to cervical vascular trauma, stable patients with Zone I and III injuries underwent diagnostic angiography, while all patients with Zone II were surgically explored. Despite its advantages, angiography is an invasive procedure with a 1–2 % risk of complications, including puncture site hematomas, distal embolization of atheromatous plaques or thrombus, and arterial dissection [9]. Catheter angiograms also require technical expertise to perform, and trained personnel may not always be immediately available on-site. Waiting for the requisite support personnel to arrive may delay the diagnosis and treatment of an unstable patient. These limitations coupled with the relatively high negative angiography rates (ranging from 10 to 30 %) have allowed noninvasive imaging modalities to supplant catheter angiography as the preferred initial diagnostic study.
Helical computed tomographic angiography (CTA) has become faster and more available over the last decade allowing it to play a more prominent role in the assessment of penetrating neck trauma. A recent review on imaging for neck trauma which included multiple prospective studies comparing helical CTA to catheter angiography reported that the sensitivity and specificity for helical CTA ranged from 90 to 100 % [10]. A helical CTA of the neck can be done in minutes, with no need for direct physician intervention, thereby reducing the time to diagnose and treat cervical vascular injuries. Widely used standardized protocols have also made this test reproducible, and high-quality studies can be obtained in almost any institution. CTA enables the physician to assess soft-tissue injuries documenting any damage in the head or chest and potentially determine the trajectory of the missile. Tracing the trajectory of injury can facilitate prompt evaluation of injuries to other vital structures in the area including the spinal column and aerodigestive tract [4]. With 64-slice scanners and the most current software, multiplanar reformations and 3-dimensional reconstructions are immediately available, increasing the diagnostic yield of these studies. There have been only occasional reports of major vascular injuries that were missed by CT scan; however, the majority of these have involved venous injuries without significant hemorrhage [11]. Given its speed, immediate availability, and accuracy, CTA has become the de facto first-line study in most institutions for the stable patient with a penetrating neck injury.
Metallic implants or projectile fragments create imaging artifacts which degrade the diagnostic accuracy of CT scans. In these cases, catheter-based arteriography may be required to reach a definitive diagnosis. When multiple studies are required, patients can receive a large contrast load, which may adversely affect renal function. Rarely is there time to assess renal function in a rapidly evolving trauma situation, but if a trauma patient has known renal insufficiency, a directed catheter arteriogram can minimize overall contrast volume.
Although other noninvasive imaging modalities exist, they have a limited role in the evaluation of cervical trauma. Color Doppler ultrasonography has the potential advantage of being a portable, cheap, noninvasive test that does not require the intravenous contrast dye. Its drawbacks include the fact that it is operator-dependent, requires a long examination time, and can rarely evaluate for injuries to Zone I or III. Artifacts within the scanning field and bone or soft-tissue injuries also reduce the ability of ultrasound to evaluate cervical vascular structures. Magnetic resonance angiography (MRA) has occasionally been used to assess vascular injury following penetrating trauma, but it is a time-consuming study that requires MR-compatible equipment and on-site technical expertise for scanning protocols and interpretation. The potential presence of ferromagnetic fragments in the neck after trauma is a contraindication to MRA in many trauma situations.
Blunt Injuries
Incidence and Presentation
Although blunt cerebrovascular injuries occur in less 0.75 % of all trauma patients, they can have devastating consequences. Mortality rates of blunt carotid injuries range from 16 to 59 %, with 24 to 58 % of survivors having severe neurological deficits [12–17]. The extremely variable clinical presentation of blunt cerebrovascular injuries may account for their high morbidity and mortality. Traditional hard signs of vascular trauma are rarely apparent, and concomitant facial and head injuries can limit the physician’s ability to pick up subtle alterations in the neurologic exam. There may also be a latent period between time of injury and the appearance of symptoms. Studies suggest that 25–50 % of patients develop symptoms more than 12 h after the traumatic event, and there have even been reports of symptoms presenting several days after the initial injury [13, 16, 17]. In contrast, some patients with minimal trauma due to a minor fender bender or sports injury can sustain a carotid dissection and present with a severe neurologic deficit. Such wide variability in presentation means a blunt cerebrovascular injury may not be readily appreciated or considered in the context of an unstable patient with multisystem blunt injury. While a stab or bullet wound to the neck immediately draws attention to the possibility of a cervical vascular injury, the differential diagnosis for a polytrauma patient with a low Glasgow Coma Score (GCS) is quite long. Evaluation and management should ideally focus on screening the appropriate patient cohort to detect this type of injury early.
Blunt cerebrovascular injury results from one of four mechanisms: hyperextension/rotation, direct force to the vessel, intraoral trauma, or laceration by bony fragments. These forces most commonly cause intimal damage with dissection and thrombus formation. Thrombus can either occlude the vessel completely or embolize to the cerebral circulation, while dissection can lead to pseudoaneurysm formation. In very rare cases, complete transection and exsanguination occurs. Motor vehicle accidents are the most common cause of blunt cerebrovascular injuries (41–70 %), while other mechanisms include pedestrians struck (17–33 %), assault (10–20 %), hanging, and sports injuries [14, 17]. Bilateral injuries occur in 18–41 % of cases [12, 16, 17]. Not surprisingly, blunt cerebrovascular injury is associated with injuries to other important structures, including closed head injuries (48–65 %), facial fractures (22–60 %), thoracic injuries (19–63 %), intra-abdominal injuries (16–30 %), and extremity fractures (25–39 %) [4, 13, 16, 17]. Not only do these associated injuries contribute to the delay in diagnosis, they also complicate subsequent management. A patient’s carotid dissection might cause ischemic injury in some cases, but class IV hemorrhagic shock or a tension pneumothorax will cause death in short order, and management of these injuries takes precedence.
Although a majority of patients with blunt cerebrovascular injury have no obvious symptoms upon presentation, there are certain findings that should prompt immediate diagnostic imaging. These symptoms include arterial bleeding from the neck, mouth, ear, or nose; expanding hematoma, a cervical bruit in a patient less than 50 years old; and any lateralizing neurological deficits or Horner syndrome. Other findings on initial evaluation which may not have a high correlation with vascular injury include: high-energy mechanism, near hanging, seat-belt abrasion, cervical vertebral fracture, and diffuse axonal injury. As a general rule, a patient with neurologic deficits not explained by the findings on the initial head CT requires further evaluation. Liberal use of vascular imaging of the neck can avoid missing a cervical vascular injury in the clinical setting of severe blunt trauma and a decreased GCS.
For the asymptomatic blunt force trauma patient, the decision to proceed with neurovascular imaging is more difficult. A number of factors involving mechanism of injury, as well as certain physical findings, have been associated with blunt cerebrovascular injury (Table 14.2). Given the high morbidity and mortality associated with a missed blunt cerebrovascular injury, screening protocols have been developed to help identify asymptomatic patients at risk for these injuries (Table 14.3). The first widely implemented screening protocol was developed at the Denver Health Medical Center [13]. Based on this criteria, 4.8 % of trauma patients were screened, of which 18 % were found to have an injury [14]. Having one of the risk factors predicted a carotid injury in 33–48 % of patients, while all four risk factors predicted 93 % of injuries [14]. The second screening protocol, developed at the University of Tennessee in Memphis, resulted in 3.5 % of all trauma patients getting screened, with 29 % of screened patients found to have an injury [18]. Despite aggressive screening, over 20 % of patients with a blunt cerebrovascular injury will have none of the risk factors identified by these protocols (Table 14.4) [14–17]. A recent meta-analysis of common diagnostic screening criteria (basilar skull fracture, cervical abrasion, GCS <8 with head or neck injury, neurological deficit, and head, cervical spine, thoracic, or abdominal injury) found that only cervical spine and thoracic injury were significantly associated with blunt cerebrovascular injury [19]. This study does not advocate screening only patients with cervical spine or thoracic injuries, as occult blunt cerebrovascular injuries would certainly be missed. Instead, these studies emphasize the importance of considering the possibility of a cerebrovascular injury in a blunt force trauma patient with unexplained symptoms referable to the head and neck. Figure 14.6 demonstrates a carotid dissection in a patient who presented only with neck pain after sustaining a very minor sports-related trauma.
Table 14.2
Risk factors for blunt cerebrovascular injury
Arterial bleeding from neck, mouth, ear, or nosea |
Expanding hematomaa |
Cervical bruit (if patient less than 50 years old)a |
Focal neurological deficit (e.g., hemiparesis, vertebrobasilar insufficiency, Horner syndrome)a |
Unexplained neurologic symptomsa |
Basilar skull fracture |
Facial fractures |
Closed head injury |
Spinal cord injury (especially cervical spine) |
Neck soft-tissue injury |
– Stable hematoma |
– Hanging or near hanging |
– Clothesline-type injury |
– The “seat-belt sign” |
Table 14.3
Screening protocols for blunt cerebrovascular injury
Memphis criteria [18] | |
|---|---|
Signs/symptoms | Cervical spine fracture |
Cervical hematoma | Unexplained neurologic deficit |
Cervical bruit | Horner syndrome |
Focal neurological deficit | Leforte II or III fracture pattern |
Unexplained neurological deficit | Basilar skull fracture with involvement of the carotid canal |
Risk factors | Neck soft-tissue injury (i.e., seat-belt sign, hanging, or hematoma) |
Leforte II or III fracture pattern | |
Basilar skull fracture with involvement of the carotid canal | |
Head injury with GSC <6 | |
Near hanging with anoxic brain injury | |
Any cervical spine fracturea |
Table 14.4
Grading system for blunt cerebrovascular injury [23]
Injury grade | Criteria | Stroke incidence (%) |
|---|---|---|
I | Luminal irregularity with <25 % narrowing | 3 |
II | Intraluminal thrombus, dissection or intramural hematoma with >25 % narrowing | 11 |
III | Pseudoaneurysm | 33 |
IV | Occlusion | 44 |
V | Transection with extravasation | 100 |
Diagnostic Imaging
Although arteriography remains the gold standard, CTA has become the screening test of choice for suspected blunt cerebrovascular injury, as evidenced by its integration into the practice guidelines of both the Eastern Association for the Surgery of Trauma [20] and the Western Trauma Association [21]. Most patients who have risk factors for blunt cerebrovascular injury have indications for scanning other regions of the body, and a CTA protocol can easily be incorporated into the imaging plan. The entire noninvasive study can be completed in less than 5 min with a contrast load which is not excessive. While initial studies questioned the sensitivity and specificity of CTA [18], more recent studies with experienced radiologists using 16- or 64-slice CT scanners found that the accuracy of CTA approached that of angiography [15, 22]. Accordingly, CTA has emerged as the test of choice for screening patients with suspected cerebrovascular injuries, with arteriography reserved for equivocal results or high clinical suspicion.
As with penetrating neck trauma, other noninvasive imaging modalities play a limited role in the evaluation of blunt cerebrovascular trauma. Duplex ultrasound by an experienced sonographer will often pick up flow abnormalities due to dissection, but it is an operator-dependent test that can only detect injury in Zone II. Small intimal tears and nonocclusive dissections usually go undetected by duplex ultrasound. MRA provides high resolution images free of bony artifact without the use of IV contrast. Although MRA may detect cerebral infarction earlier, the time required for image acquisition and logistical issues with unstable, ventilated trauma patients make it impractical for general use in the setting of trauma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


