Chapter 4 Valvular heart disease
Introduction
Cine imaging using SSFP and velocity mapping sequences are the cornerstone of CMR valvular assessment. Breath-hold high-resolution FSE can be useful for valve morphology and developments such as moving slice velocity mapping and real-time imaging will improve evaluation in the near future. CMR reporting in valvular heart disease generally includes:
Aortic stenosis
AS has a long asymptomatic period after which clinical symptoms such as angina, exertional dyspnoea and effort syncope may result. Since symptoms develop late in the pathophysiology of AS, clinical deterioration soon follows if valve replacement is not undertaken. Obstruction to the LVOT leads to elevated LV pressures and compensatory LVH which initially maintains cardiac output and reduces LV wall stress, but ultimately decreases LV compliance and increases end-diastolic pressure. Increased myocardial oxygen demand causes myocardial ischaemia and later LV failure.
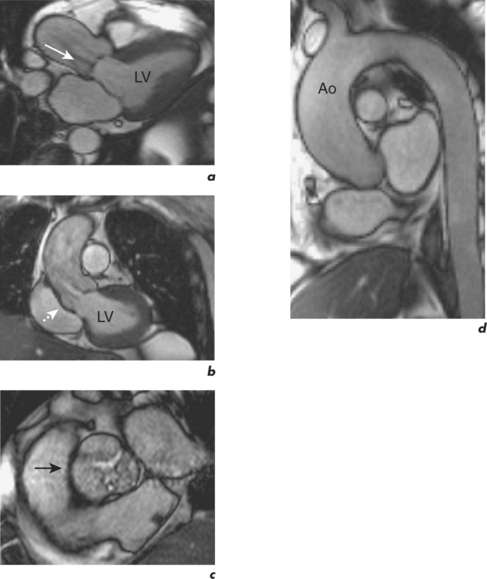
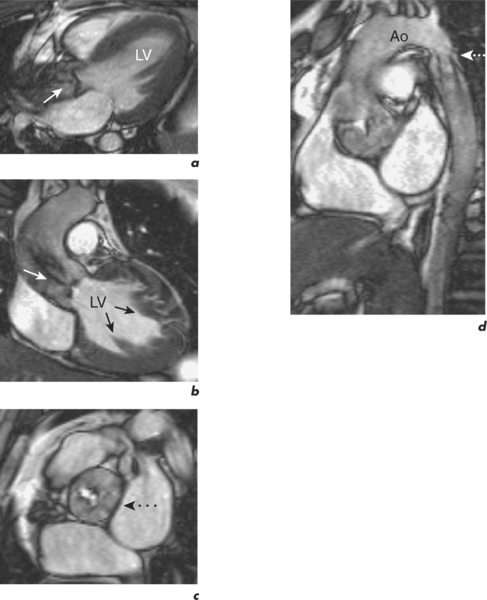
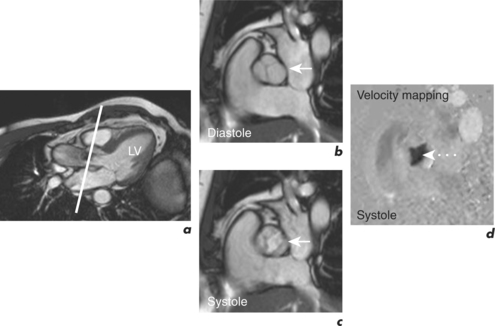
CMR is a robust method of calculating the severity of AS and correlates well with continuous wave Doppler echocardiography. However, it is far superior to echocardiography in identifying the cardiovascular functional and morphological sequelae of AS, such as post-stenotic dilatation of the ascending aorta, degree of LVH, and myocardial viability (Figures 4.1 and 4.2). These are important factors in the assessment of patients prior to valve replacement surgery, which often includes CABG and aortic root replacement. CMR also provides an excellent modality for serial surveillance of parameters such as LV function, volumes and mass in patients under follow-up and post operatively. This is done using the pre-contrast part of the protocol outlined in Chapter 1. Cines can demonstrate thickening and bulging of the aortic cusps and turbulent flow in the aorta. Imaging in an oblique sagittal plane parallel to the valve may demonstrate restricted opening and closure of the valve, and is frequently satisfactory for direct planimetry of the valve orifice and evaluation of bicuspid valve morphology. Direct planimetry can be performed using cine imaging or velocity mapping sequences (Figure 4.3).
Velocity mapping is primarily used, however, to calculate the pressure gradient across the AV using the modified Bernoulli equation;
where ΔP (mmHg) is the pressure drop across the stenosis, and Vmax is the peak velocity (m/s) determined by velocity mapping 1 to 1.5 cm above and parallel to the valve plane (Figure 4.3d). The typical Venc setting for the LVOT is 2 m/s, and 2.5 to 4 m/s for the aorta. An initial Venc of 2.5 m/s is often used and adjusted upwards if there is velocity aliasing (Figure 1.3). The velocity of blood flow through the AV is greater than that through the MV.
Severity of AS is graded as: mild >1.5 cm2, moderate 1.0–1.5 cm2, severe <1.0 cm2, and critical <0.8 cm2. In severe AS, the peak transvalvular gradient is usually >50 mmHg.
Specific CMR reporting features for AS include: