General considerations
Development
Cardiac valves develop from the mesodermal germ layer between the 4th and 7th week of gestation. Any factors affecting embryogenesis during this time can affect development of valves and include infection (German measles/rubella), drugs, etc.
Key points
Mitral valve
Aortic valve
Tricuspid valve
Acute rheumatic fever
Epidemiology
Pathology
Clinical features
Treatment
See Table 3.1.
Table 3.1 Treatment of rheumatic fever
| Drug/treatment | Dose |
| Antibiotics | Oral phenoxymethylpenicillin for 10 days (250 mg qds (four times a day) in children and 500 mg tds in adults) |
| Or intramuscular benzylpenicillin (single dose of 1.2 million units) to treat the acute infection | |
| Oral erythromycin, if penicillin allergic, for 10 days (20–40 mg/kg/day qds in children and 250 mg qds in adults) | |
| Alternatives include clarithromycin, azithromycin, or cefalexin | |
| Oral aspirin | 4–8 g daily until erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are normal |
| Prednisolone | 2 mg/kg/day for 2–4 weeks if moderate–severe carditis. |
| Oral haloperidol for chorea | 0.5–2 mg tds in adults and 0.05–0.15 mg/kg/day in 3–12-year-old children |
| Use diuretics, angiotensin-converting enzyme inhibitors (ACE-Is), and digoxin for heart failure | |
| Surgery for chronic, severe rheumatic valve disease (results are less durable in acute phase) |
Prognosis
Diagnostic criteria for rheumatic fever (Jones criteria)
Evidence of group A streptococcal pharyngitis
Either a positive throat culture or rapid streptococcal antigen test, or an elevated or rising streptococcal antibody titre (samples taken two weeks apart)
Plus two major or one major and two minor Jones criteria:
| Major criteria | Minor criteria |
| • Polyarthritis | • Fever |
| • Carditis | • Arthralgia |
| • Chorea | • Prolonged PR interval |
| • Erythema marginatum | • Elevated ESR and CRP |
| • Subcutaneous nodules |
Mitral stenosis: clinical features
Causes
Mitral stenosis (MS) is most commonly due to rheumatic fever. Other causes are rare. They include congenital (isolated lesion or in association with an atrial septal defect (ASD)—Lutembacher’s syndrome), mitral annular calcification, carcinoid heart disease, valvulitis (systemic lupus erythematosis), mucopolysaccharidoses (e.g. Hurler’s syndrome), and endocardial fibroelastosis. Stenosis occurs at three levels: the chordae (fuse, thicken, then shorten), cusps (initially rolled under edges, then thicken and eventually calcify), and commissures (progressive fusion).
Pathophysiology
Elevated left atrial (LA) pressure is required to propel the blood through the narrowed mitral valve orifice. This leads to pulmonary venous pressure and exertional dyspnoea due to pulmonary oedema and pulmonary compliance. Reactive pulmonary hypertension occurs leading to right ventricular (RV) hypertrophy and failure. LV function is initially unaffected. However, since filling is impaired, adequate cardiac output (CO) cannot always be maintained. The rise in CO during exertion is blunted. Onset of atrial fibrillation (AF) is associated with abrupt clinical deterioration, due to both the loss of atrial systole and the fast heart rate (decreased duration of diastole).
Clinical features
(see also Fig. 3.1)
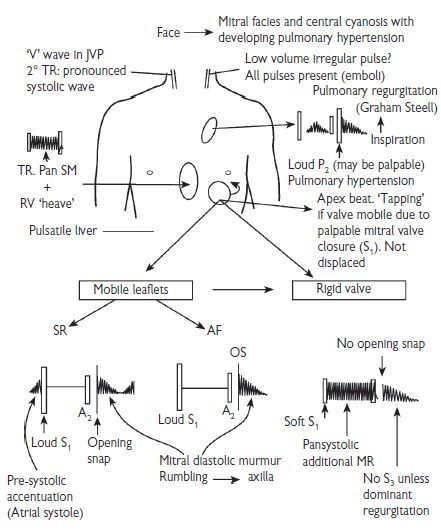
Fig. 3.1 Physical signs in mitral stenosis. Reproduced with permission from Swanton H (2003). Pocket Consultant: cardiology. 5th ed. Oxford: Blackwell Publishing. SM = systolic murmur; SR = sinus rhythm; TR = tricuspid regurgitation.
History
Physical examination
Mitral facies or malar flush seen in <50%. Prominent ‘a’ waves in jugular venous pulse (JVP). Low-amplitude arterial pulse. Irregularly irregular pulse in AF. ‘Tapping’ apex beat—palpable S1. Diastolic thrill at apex. Left parasternal heave (due to right ventricular hypertrophy (RVH)). Palpable pulmonary closure.
Auscultation: S1 loud if in sinus rhythm and valve is pliable. P2 accentuated. Opening snap (OS) of the MV is heard best at or medial to the apex in expiration. A2–OS interval varies inversely with severity of stenosis. Low-pitched, rumbling, mid-diastolic murmur with pre-systolic accentuation (if in sinus rhythm) is heard best at the apex with the patient in a left lateral position. Early diastolic murmur due to pulmonary regurgitation from pulmonary hypertension (Graham Steell murmur) may be heard rarely.
Mitral stenosis: investigations
Investigations
Radiographic features of mitral stenosis
| PA film | Lateral film |
| • Straight or convex L heart border | • LA or RV enlargement |
| • Double shadow of LA behind RA | • Valvular calcification frequent |
| • Splaying of carina (>90o)—rare | • LA calcification seen rarely (McCallum’s patch) |
| • Prominent pulmonary conus | • Oesophageal indentation on barium swallow |
| • Pulmonary haemosiderosis |
Classification
See Table 3.2.
Table 3.2 Classification of mitral stenosis
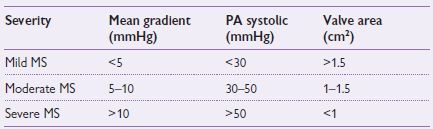
PA = pulmonary artery.
Management
Medical management
Balloon valvotomy
Indications for surgery
Surgical treatment
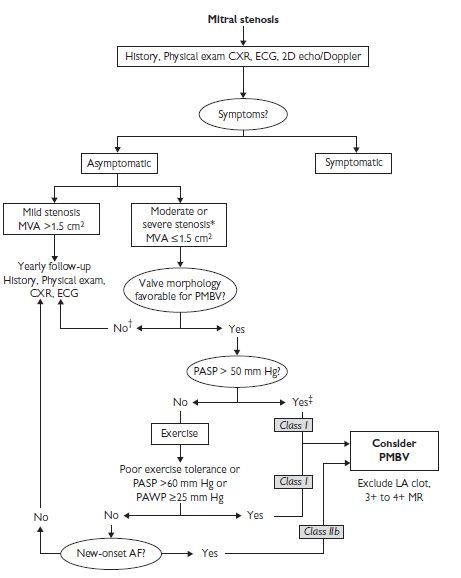
Fig. 3.2 Management strategy for patients with mitral stenosis. *The writing committee recognizes that there may be variability in the measurement of mitral valve area (MVA) and that the mean transmitral gradients, pulmonary artery wedge pressure (PAWP), and pulmonary artery systolic pressure (PASP) should also be taken into consideration. †There is controversy as to whether patients with severe mitral stenosis (MVA less than 1.0 cm2) and severe pulmonary hypertension (pulmonary artery pressure greater than 60 mm Hg) should undergo percutaneous mitral balloon valvotomy (PMBV) or mitral valve replacement to prevent right ventricular failure. ‡Assuming no other cause for pulmonary hypertension is present. AF indicates atrial fibrillation; CXR, chest X-ray; ECG, electrocardiogram; echo, echocardiography; LA, left atrial; MR, mitral regurgitation; and 2D, 2-dimensional. Reproduced with permission from Journal of the American College of Cardiology, Vol 48, No.3, 2006. August 1, 2006:e1–148. Bonow et al, AHA/ACC Best Practice Guidelines.
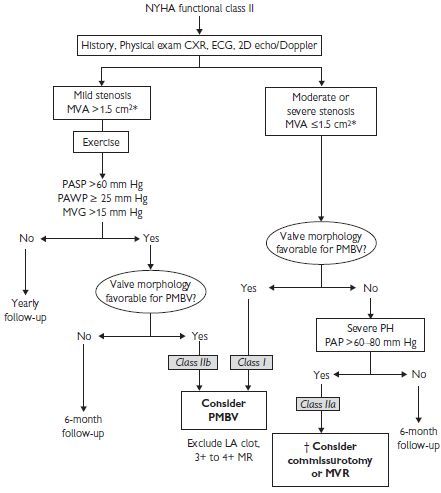
Fig. 3.3 Management strategy for patients with mitral stenosis and mild symptoms. *The committee recognizes that there may be variability in the measurement of mitral valve area (MVA) and that the mean transmitral gradient, pulmonary artery wedge pressure (PAWP), and pulmonary artery systolic pressure (PASP) should also be taken into consideration. †There is controversy as to whether patients with severe mitral stenosis (MVA less than 1.0 cm2) and severe pulmonary hypertension (PH; PASP greater than 60 to 80 mm Hg) should undergo percutaneous mitral balloon valvotomy (PMBV) or mitral valve replacement (MVR) to prevent right ventricular failure. CXR indicates chest X-ray; ECG, electrocardiogram; echo, echocardiography; LA, left atrial; MR, mitral regurgitation; MVG, mean mitral valve pressure gradient; NYHA, New York Heart Association; PAP, pulmonary artery pressure; and 2D, 2-dimensional. Reproduced with permission from Journal of the American College of Cardiology, Vol 48, No.3, 2006. August 1, 2006:e1–148. Bonow et al, AHA/ACC Best Practice Guidelines.
Mitral stenosis guidelines
Mitral regurgitation
Causes
Acute:
Infective endocarditis, acute myocardial infarction (MI), trauma.
Chronic:
Most common—myxomatous degeneration (mitral valve prolapse), chronic rheumatic heart disease, left ventricular or annular dilatation of any cause (e.g. chronic ischaemia, cardiomyopathy, annular calcification), degeneration of valve cusps, collagen vascular disease, hypertrophic cardiomyopathy.
Nomenclature
Pathophysiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


