CHAPTER 2 Valves
2.1 MITRAL VALVE (MV)
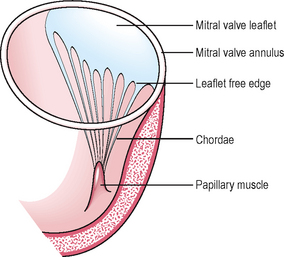
The 2 leaflets are attached at one end to the annulus and at the other (free) edge to the chordae which are fixed to the LV by the papillary muscles. The chordae hold each of the MV leaflets like cords hold a parachute canopy. The leaflets’ free edges meet at 2 points called the commissures (Figs 2.1, 2.2).
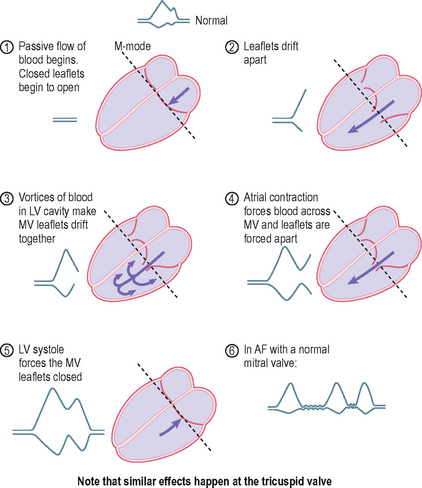
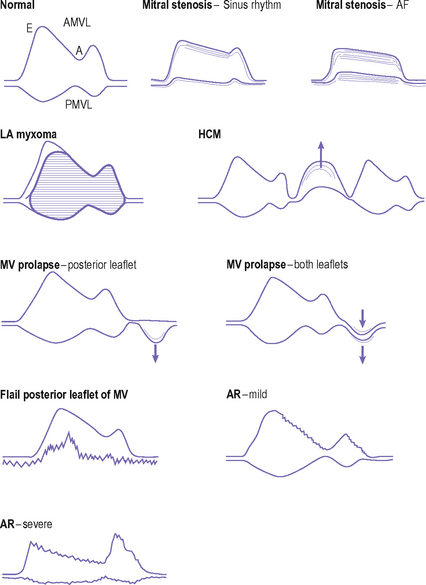
Movement of the MV leaflets can be seen by M-mode and 2-D echo. The normal MV leaflets have a characteristic movement pattern on M-mode examination. The anterior MV leaflet (AMVL) sweeps an M-shape pattern, while the posterior leaflet (PMVL) sweeps a W-shaped pattern (Fig. 1.11a). Understanding the origin of the normal MV opening and closing pattern is easy and helps in understanding abnormal patterns in disease (Fig. 2.3).
The first peak of MV movement (early, E-wave) coincides with passive LA to LV flow. The second peak coincides with atrial contraction and active flow of blood into the LV (atrial, A-wave). This pattern of movement is brought about by the characteristics of blood flow into the LV. This second peak is lost in AF, where atrial mechanical activity is absent. On 2-D examination, the normal MV leaflets should be seen to be thin, mobile and separate and close well. Their motion should be of a double waveform as expected from the M-mode findings. The Doppler pattern of mitral flow shows a similar pattern to M-mode movement of the MV leaflets.
Mitral stenosis (MS)
In practical terms, the only common cause of MS is rheumatic heart disease.
Much rarer causes include mitral annulus calcification (usually asymptomatic and more likely to be associated with MR, rarely stenosis), congenital (may be associated with congenital aortic stenosis or aortic coarctation), connective tissue disorders and infiltrations, systemic lupus erythematosus (SLE), rheumatoid arthritis, mucopolysaccharidoses (Hurler’s syndrome) and carcinoid.
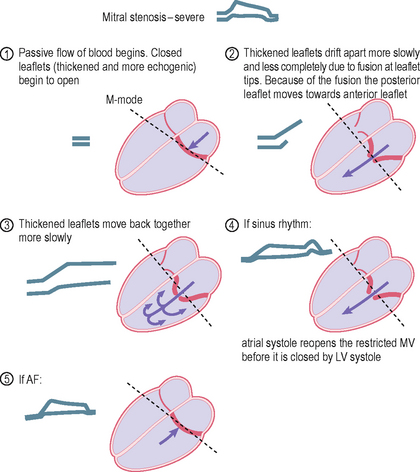
Rheumatic fever is an autoimmune phenomenon caused by cross-reaction of antibodies to streptococcal bacterial antigens with antigens found on the heart. In its acute stages, rheumatic fever is associated with inflammation of all layers of the heart – endocardium (including that of the valves), myocardium and pericardium. MS does not occur at this stage, but many years later as a consequence of this initial inflammatory process. The MV leaflets progressively fuse, initially at the commissures and free edges, which become thickened and later calcified. The inflamed valve becomes progressively thickened, fibrosed and calcified. This restricts the opening and closing of the valve. The chordae may also become thickened, shortened and calcified, further restricting normal valve function. The leaflets shrink and become rigid. The size of the MV orifice reduces leading to MS, which restricts blood flow from LA to LV.
The M-mode pattern changes in a predictable way (Fig. 2.4). The movement of the leaflets is more restricted, and the leaflet tips are fused, so the posterior leaflet is pulled towards the anterior leaflet rather than drifting away from it. In severe MS, there is often AF rather than sinus rhythm, and the 2nd peak of MV movement is lost. The calcified leaflets reflect ultrasound in a different pattern from normal leaflets due to their increased thickness, fibrosis and often calcification. Instead of a single echo reflection giving a sharp image of the leaflets, there is a reverberation with several echo reflections giving a fuzzy image. Calcified leaflets produce a stronger echo reflection.
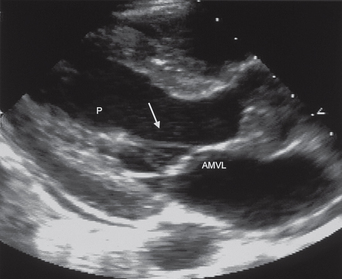
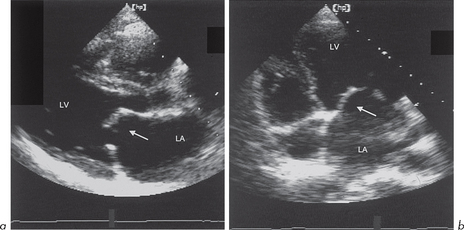
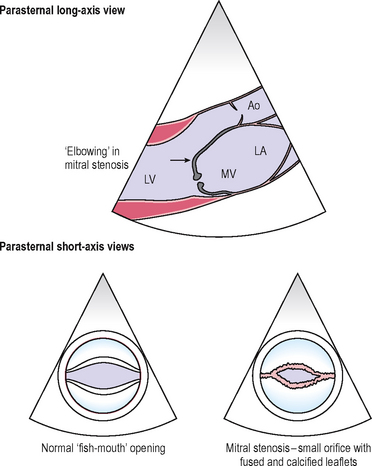
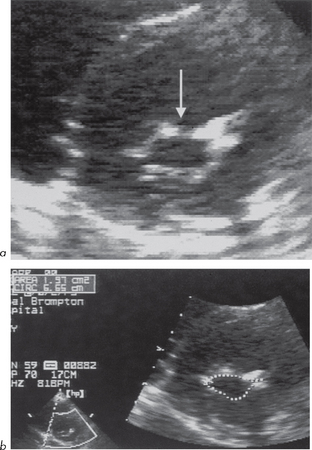
On 2-D echo, the MV leaflets can be seen to be thickened and their movement restricted. Because of the fusion of the anterior and posterior leaflet tips, while the leaflet cusps may remain relatively mobile, there may be a characteristic ‘elbowing’ or ‘bent-knee’ appearance, particularly of the anterior MV leaflet (Figs 2.5, 2.6). This has also been likened to the bulging of a boat’s sail as it fills with wind. The LA also enlarges.
MV orifice area (Fig. 2.7) can also be measured using Doppler (Ch. 3).
Criteria for diagnosis of severe MS (many derived from Doppler)
A number of diseases produce other typical mitral M-mode patterns (Fig. 2.8):
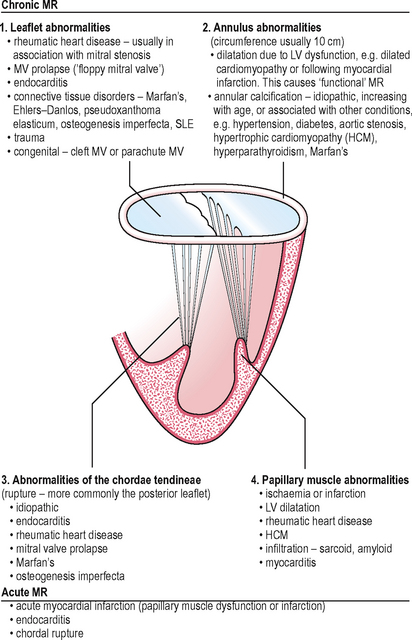
Mitral regurgitation (MR)
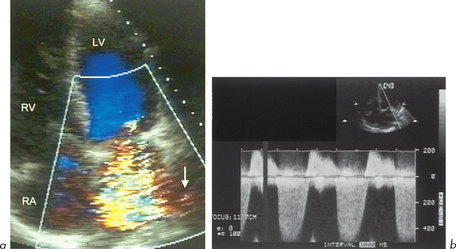
Echo assessment of severity of MR
While the diagnosis of MR may be easy (Fig. 2.9), the echo assessment of severity can be difficult. A balance must be made of all the echo information. The severity relates to the regurgitant fraction, which depends on:
The features of severe chronic MR are those of:
Doppler echo features of severe MR (Fig. 2.10):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree