Incomplete revascularization is common after percutaneous coronary intervention (PCI). Whether a “reasonable” degree of incomplete revascularization is associated with a similar favorable long-term prognosis compared with complete revascularization remains unknown. We sought to quantify the proportion of coronary artery disease burden treated by PCI and evaluate its impact on outcomes using a new prognostic instrument—the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) Revascularization Index (SRI). The baseline SYNTAX score (bSS), the residual SYNTAX score, and the delta SYNTAX score (ΔSS) were determined from 888 angiograms of patients enrolled in the prospective SYNTAX trial. The SRI was then calculated for each patient using the following formula: SRI = (ΔSS/bSS]) × 100. Outcomes were examined according to the proportion of revascularized myocardium (SRI = 100% [complete revascularization], 50% to <100%, and <50%). The Youden index for the SRI was computed to identify the best cutoff for 5-year all-cause mortality. The mean bSS was 28.4 ± 11.5, and after PCI, the mean ΔSS was 23.8 ± 10.9 and the mean residual SYNTAX score was 4.5 ± 6.9. The mean SRI was 85.3 ± 21.2% and was 100% in 385 patients (43.5%), <100% to 50% in 454 patients (51.1%), and <50% in 48 patients (5.4%). Five-year adverse outcomes, including death, were inversely proportional to the SRI. An SRI cutoff of <70% (present in 142 patients [16.0%] after PCI) had the best prognostic accuracy for prediction of death and, by multivariable analysis, was an independent predictor of 5-year mortality (hazard ratio [HR] 4.13, 95% confidence interval [CI] 2.79 to 6.11, p <0.0001). In conclusion, the SRI is a newly described method for quantifying the proportion of coronary artery disease burden treated by PCI. The SRI is a useful tool in assessing the degree of revascularization after PCI, with SRI ≥70% representing a “reasonable” goal for patients with complex coronary artery disease.
The Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) score (SS) has become a well-established instrument to quantify the extent and complexity of baseline coronary artery disease (CAD). It has been validated in many populations and patient subsets. The residual SYNTAX score (rSS) was designed and validated to quantify the absolute amount of untreated CAD after percutaneous coronary intervention (PCI) revascularization. An rSS ≥8 was identified as a level of incomplete revascularization strongly associated with increased mortality and adverse ischemic events. Recently, the SYNTAX Revascularization Index (SRI), representing the proportion of treated baseline CAD (baseline SYNTAX score [bSS]; delta SYNTAX score [ΔSS]), was developed as a tool to better quantify and describe the proportion of the disease treated (SRI = ΔSS/bSS × 100) by PCI revascularization. The SRI has been shown to be an independent predictor of 1-year mortality in patients with non–ST-elevation acute coronary syndrome and can be used as a “goal” to be achieved by PCI. However, external validation of this concept in a different population and who underwent longer follow-up is lacking. We, therefore, aimed to externally validate the SRI as a new prognostic tool in patients who underwent PCI from the randomized SYNTAX trial.
Methods
The SYNTAX trial was a randomized, prospective, multicenter trial investigating patients with de novo 3-vessel CAD and/or unprotected left main CAD (isolated or associated with 1-, 2-, or 3-vessel disease). In brief, a total of 1,800 patients were recruited and randomized to PCI (n = 903) or coronary artery bypass grafting (CABG; n = 897) from 85 centers in Europe and the United States. Exclusion criteria were limited to subjects with previous coronary revascularization, the requirement of concomitant cardiac surgery, or ongoing acute myocardial infarction (MI). During the local Heart Team meeting, the interventional cardiologist and cardiac surgeon specified the number of coronary lesions requiring treatment, their angiographic location, and characteristics using the bSS ( http://www.syntaxscore.com ). In case equivalent anatomical revascularization could be achieved with both treatment strategies, were randomized on a 1:1 basis (n = 1,800) to either PCI with TAXUS Express paclitaxel-eluting stents (Boston Scientific Corporation, Natick, Massachusetts) or CABG. Stratification was performed by 3 ways: by clinical site, the absence or presence of unprotected left main disease, and by the presence or absence of medically treated diabetes mellitus (requiring oral medications or insulin). Baseline and peri- and post-procedural data were prospectively collected by the individual participating centers. The calculation of the bSS was carried out by the Heart Team before randomization and corroborated by an independent core laboratory (Cardialysis BV, Rotterdam, The Netherlands) blinded to the treatment assignment. Baseline and procedural coronary angiograms were centrally stored. The baseline and procedural coronary angiograms were analyzed side by side by a panel of 3 interventional cardiologists blinded to the clinical outcomes.
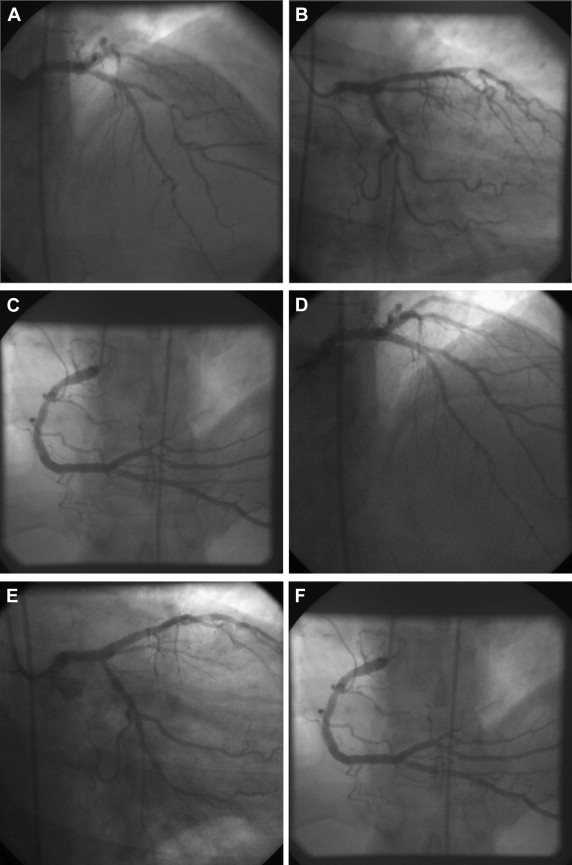
The bSS and its components, including anatomic location of all lesions, recorded by the core laboratory in calculation of the original SS, were used to identify all coronary lesions in the baseline and procedural coronary angiogram. The rSS was calculated based on the remaining obstructive CAD after treatment with PCI. The intraobserver variability for calculation of the rSS (quartile partitioning), based on reanalyzing 50 cases at a 3-month interval, indicated a high level of agreement (κ statistic 0.89, 95% confidence interval [CI] 0.79 to 0.99, p <0.001). The ΔSS, representative of the burden of disease treated by PCI, was calculated by subtracting the rSS from the bSS. The SRI was calculated with the following formula: (ΔSS/bSS × 100). Figure 1 illustrates the bSS and all its derived scores. Patients were stratified into 3 groups (as previously described) and compared: SRI = 100% (complete revascularization), SRI <100% to 50%, and SRI <50%. Adverse ischemic outcomes between groups were compared at 5 years.
Clinical outcomes included all-cause death major adverse cardiac and cerebrovascular events (MACCE; a composite of all-cause death, MI, cerebrovascular accident, and all-cause revascularization), and stent thrombosis using the Academic Research Consortium definition. An independent clinical events committee, including cardiologists, cardiac surgeons, and a neurologist, reviewed all the primary clinical end points. A separate independent clinical events committee adjudicated the Academic Research Consortium stent thrombosis events.
Categorical variables are presented as numbers and percentages and are compared with the chi-square test. Continuous variables are expressed as mean ± SD and are compared using the Student’s t test or Wilcoxon rank-sum test based on their distributions. Time-to-event variables are presented as Kaplan-Meier estimates and compared using the log-rank test. Multivariable analyses were performed to identify independent predictors of incomplete revascularization (SRI <100%). Multivariable analyses were conducted to identify independent predictors of 5-year mortality, with a Cox regression model using the forced enter method. Previously demonstrated anatomic and clinical variables, shown to be independent predictors of long-term mortality in the SYNTAX trial (p <0.1), were entered into the model, with no exit criteria. Area under the curve for the SRI was computed to identify the Youden index (best cutoff) for 5-year all-cause death. The Youden index is defined for all points of a receiver operating characteristic curve, and the maximum value of the index was used as a criterion for selecting the optimum cut-off point for the SRI. The index is represented graphically as the height above the chance line. It is equivalent to the area under the curve represented by a single operating point. All variables were stratified according to an SRI >70% (best cutoff). A 2-sided probability value <0.05 was considered significant for all tests. All analyses were conducted using SPSS, version 21.0 (IBM, Armonk, New York).
Results
In the randomized PCI cohort (n = 903), the bSS was available in 899 of 903 subjects (99.6%). The mean bSS was 28.4 ± 11.5. The SRI was available in 888 of 903 subjects (98.3%). The SRI ranged from 47.1% to 100%, with a mean of 85.3 ± 21.2. The SRI was 100% in 386 patients (43.5%), from 50% to <100% in 454 patients (51.1%), and <50% in 48 patients (5.4%). Table 1 presents the clinical characteristics and angiographic findings, stratified by SRI. Patients with lower SRI had a higher prevalence of diabetes, diabetes requiring insulin, and lower left ventricular ejection fraction. Angiographically, patients with a lower SRI were more likely to have more complex and extensive disease, with a more frequent presence of chronic total occlusion (CTO), heavily calcification, long (>20 mm) and tortuous lesions, involvement of the left main with 3-vessel disease, resulting in higher bSS and rSS, and longer procedural time. Independent predictors of incomplete revascularization (SRI <100%) included bSS (HR 1.08, 95% CI 1.07 to 1.10, p <0.0001) and diabetes mellitus (HR 1.82, 95% CI 1.31 to 2.54, p = 0.0003).
Variables | SRI = 100% (N=386) | SRI 50% to <100% (N=454) | SRI <50% (N=48) | p Value |
|---|---|---|---|---|
| Age (years) | 64.6±9.8 | 65.7±9.5 | 65.9±8.5 | 0.11 |
| Men | 280 (72.5%) | 362 (79.7%) | 35 (72.9%) | 0.04 |
| Diabetes mellitus | 85 (22.0%) | 148 (32.6%) | 19 (39.6%) | 0.001 |
| Insulin-requiring diabetes | 27 (7.0%) | 53 (11.7%) | 9 (18.8%) | 0.009 |
| Body mass index (kg/m 2 ) | 28.0±4.7 | 28.1±4.9 | 29.3±4.9 | 0.27 |
| Hypertension | 273 (71.5%) | 341 (75.6%) | 39 (81.3%) | 0.20 |
| Hyperlipidemia | 300 (77.9%) | 353 (78.6%) | 41 (87.2%) | 0.34 |
| Current smoker | 79 (20.5%) | 76 (16.7%) | 9 (18.8%) | 0.38 |
| Chronic obstructive pulmonary disease | 34 (8.8%) | 34 (7.5%) | 3 (6.3%) | 0.70 |
| Peripheral vascular disease | 32 (8.3%) | 45 (9.9%) | 5 (10.4%) | 0.69 |
| History of gastrointestinal bleeding/peptic Ulcer disease | 17 (4.4%) | 16 (3.5%) | 3 (6.5%) | 0.57 |
| History of stroke/Transient ischemic attack | 27 (7.0%) | 37 (8.2%) | 5 (10.4%) | 0.65 |
| Creatinine >200 μmol/L | 4 (1.0%) | 6 (1.3%) | 0 (0.0%) | 0.69 |
| Dialysis | 1 (0.3%) | 2 (0.4%) | 0 (0.0%) | 0.83 |
| Previous myocardial infarction | 114 (29.8%) | 144 (32.1%) | 19 (39.6%) | 0.36 |
| Unstable angina | 100 (25.9%) | 146 (32.2%) | 10 (20.8%) | 0.06 |
| Baseline anatomical and clinical scores | ||||
| Baseline SYNTAX score | 23.6±10.0 | 32.2±10.9 | 29.35±13.10 | <0.001 |
| Residual SYNTAX score | 0.0±0.0 | 6.2±3.9 | 23.9±12.9 | <0.001 |
| SYNTAX Revascularization Index (%) | 100.0±100.0 | 79.9±11.1 | 17.3±22.3 | <0.001 |
| Total Parsonnet Score | 8.2±7.1 | 8.7±6.8 | 10.2±7.3 | 0.07 |
| Logistic EuroSCORE | 3.8±5.5 | 3.8±3.6 | 3.5±3.1 | 0.78 |
| Left ventricular ejection fraction (%) | 60.3±12.2 | 59.8±12.9 | 57.4±13.9 | 0.002 |
| Procedural Characteristics | ||||
| Intra-aortic Balloon Pump | 11 (2.8%) | 8 (1.8%) | 3 (6.3%) | 0.14 |
| Bifurcation | 221 (57.3%) | 305 (67.2%) | 28 (58.3%) | 0.10 |
| Trifurcation | 28 (7.3%) | 33 (7.3%) | 4 (8.3%) | 0.96 |
| Ostial lesion | 66 (17.3%) | 61 (13.4%) | 9 (18.8%) | 0.25 |
| Total occlusion | 47 (12.3%) | 145 (31.9%) | 20 (41.7%) | <0.001 |
| Severe tortuosity | 213 (55.8%) | 338 (74.4%) | 32 (66.7%) | <0.001 |
| Lesion length >20 mm | 176 (46.1%) | 292 (64.3%) | 24 (50.0%) | <0.001 |
| Heavy calcification | 163 (42.7%) | 245 (54.0%) | 28 (58.3%) | 0.002 |
| Left main lesion | 164 (42.5%) | 173 (38.1%) | 18 (37.5%) | 0.41 |
| Left main + 3-vessel disease | 37 (9.6%) | 87 (19.2%) | 10 (20.8%) | <0.001 |
| 3-vessel disease only | 211 (54.7%) | 276 (60.8%) | 30 (62.5%) | 0.17 |
| Right coronary lesion | 289 (74.9%) | 384 (86.8%) | 44 (91.7%) | <0.001 |
| Left anterior descending lesion | 328 (85.0%) | 421 (92.7%) | 43 (89.6%) | 0.001 |
| Left circumflex lesion | 300 (77.7%) | 413 (91.0%) | 44 (91.7%) | <0.01 |
| Procedure time (hours) | 1.6±0.9 | 1.8±0.9 | 2.2±1.0 | <0.001 |
| Total number of stents | 4.5±2.4 | 4.8±2.1 | 4.1±2.2 | 0.47 |
| Total stent length (mm) | 85.8±51.6 | 87.1±45.0 | 73.1±37.5 | 0.75 |
The 5-year rates of all adverse ischemic events were strongly associated with SRI, with the lowest rates of adverse events in the group with complete revascularization and the highest rates in the group with SRI <50% ( Table 2 , Figure 2 ).
| Variables | SRI = 100% (N=386) | SRI 50% to <100% (N=454) | SRI <50% (N=48) | p Value ∗ |
|---|---|---|---|---|
| Death | 33 (8.6%) | 73 (16.1%) | 16 (33.3%) | <0.0001 |
| Cardiac death | 17 (4.3%) | 51 (11.2%) | 13 (26.2%) | <0.0001 |
| Myocardial infarction | 27 (7.1%) | 48 (10.6%) | 13 (26.5%) | <0.0001 |
| Unplanned revascularization | 73 (18.9%) | 131 (28.9%) | 30 (62.5%) | <0.0001 |
| Stent thrombosis (definite/probable) | 26 (6.7%) | 43 (9.4%) | 11 (22.2%) | <0.0001 |
| MACCE | 107 (27.7%) | 192 (42.3%) | 34 (69.9%) | <0.0001 |
Receiver operating characteristic curve analysis demonstrated a significant association between the SRI and 5-year all-cause mortality. An SRI cutoff of 70% had the best prognostic accuracy for risk prediction of death (area under the curve 0.68, 95% CI 0.65 to 0.71, p <0.0001). Baseline and procedural variables associated with an SRI <70% (occurring in 142 patients [16%]) versus an SRI ≥70% (occurring in 746 patients [84.0%]) are presented in Supplementary Table 1 . Figure 3 shows the occurrence of adverse events over time according to an SRI cutoff of 70%. Figure 4 shows and compares 5-year adverse event rates among SRI 100%, 70% to <100%, and <70%. By multivariable analysis, SRI <70% remains one of the strongest independent predictors of 5-year mortality ( Table 3 ).



