Functional lesion assessment for coronary tandem lesions and its clinical applications have not been thoroughly studied. The aim of this study was to test the hypothesis that the fractional flow reserve (FFR) gradient across an individual stenosis (ΔFFR) during pressure-wire pullback is a surrogate of the relative functional severity of each stenosis in coronary tandem lesions. For in vitro validation, computational flow dynamic modeling of coronary tandem lesion with various degree of stenosis was constructed. For clinical validation, a total of 52 patients (104 lesions) with coronary tandem lesions (2 stenoses along 1 coronary artery) were consecutively enrolled, and tailored stent procedures based on ΔFFR was performed, at first treating the lesion with large ΔFFR and then subsequently reassessing the FFR for the remaining lesion. The coronary stenosis was considered functionally significant and stenting was performed when the FFR of a lesion was ≤0.80. Using in vitro computational flow dynamic modeling, the lesion with the large ΔFFR of the coronary tandem lesion was indicated as the lesion with the greater degree of simulated diameter stenosis. In the clinical cohort, 28 patients (53.8%) had only single-lesion treatment, and stent implantation for 28 lesions (26.9%) was deferred according to the proposed strategy. During the 9-month follow-up period, only 1 repeat revascularization occurred among the deferred lesions. In conclusion, for the treatment of coronary tandem lesions, ΔFFR may be a useful index for prioritizing the treatment sequence and optimizing the stenting procedure. In this way, unnecessary stent implantation can be avoided, with the achievement of favorable functional and clinical outcomes.
Fractional flow reserve (FFR) is a reliable functional index for epicardial coronary stenosis. However, a simple FFR measurement does not predict the functional severity of an individual stenosis in a coronary tandem lesion, because of the complex hydromechanic interaction between stenoses. We therefore hypothesized that the FFR gradient across an individual stenosis (designated ΔFFR) during pressure-wire pullback is a surrogate of the relative functional severity of each stenosis in a coronary tandem lesion. Accordingly, we proposed the strategy of first treating the lesion with a large ΔFFR and then subsequently reassessing the FFR for the remaining lesion. This concept of the “rule of big delta” FFR has been validated by means of computational flow dynamic (CFD) modeling of coronary tandem lesions as well as in a prospective clinical cohort.
Methods
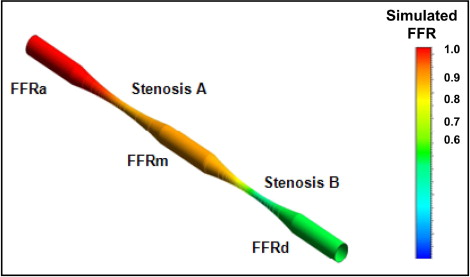
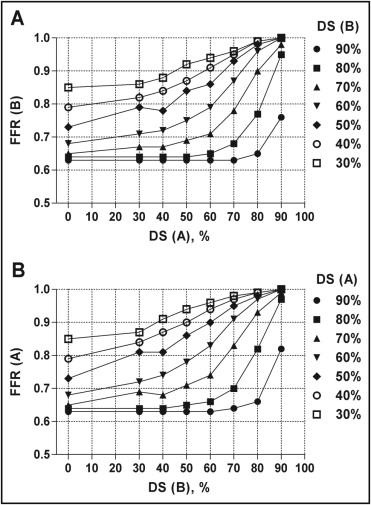
To validate the study hypothesis, we developed CFD modeling for coronary tandem lesions. Figure 1 shows a schematic figure of a simulated coronary tandem lesion. We made a total of 147 combinations of the proximal (stenosis A, 30% to 90% diameter stenosis, increasing in increments of 10%) and distal (stenosis B, 30% to 90% diameter stenosis, increasing in increments of 10%) stenoses with distances of 10, 20, and 30 mm. Herein, percentage diameter stenosis created in the simulation is equivalent to the true functional severity of an individual stenosis. In the simulation, we assumed that the downstream coronary vascular beds were maximally dilated and used the commercial CFD code (ANSYS Inc., Pennsylvania) Fluent to simulate the flow around the tandem lesion in several stenotic conditions. A detailed explanation of the approach is represented in the Supplemental Methods . We also externally validated the results of CFD modeling using historical data from a previous study by Pijls et al to obtain the formula needed to assess the individual FFR of coronary tandem stenoses in human ( Supplemental Table 1 and Supplemental Figure 1 ).
Between July 2009 and April 2011, a total of 52 patients with coronary tandem lesion for which the FFR value was ≤0.80 at a position distal to the distal stenosis were prospectively enrolled in the present analysis of clinical cohort. A coronary tandem lesion was defined as 2 separate stenoses with ≥50% diameter stenosis determined by visual estimation, within 1 epicardial coronary artery, separated by an angiographically normal appearing segment. Lesions with large side branches between the stenoses and the left main coronary artery stenosis were excluded. Patients with left ventricular ejection fractions <40%, bypass graft lesions, thrombus-containing lesions, and any contraindications to adenosine were also excluded. This study was approved by the institutional review board of our hospital, and informed consent was obtained from all patients before the study.
Catheterization is performed through the femoral route and using standard catheters. Coronary angiograms were digitally recorded and assessed off-line in a quantitative angiographic core laboratory (Asan Medical Center, Seoul, Korea), using an automated edge detection system (CAAS II; Pie Medical, Maastricht, The Netherlands) operated by experienced personnel who were unaware of the study aims. Standard qualitative and quantitative analyses and definitions were used for angiographic analysis.
FFR measurements were performed using 0.014-inch pressure wires (St. Jude Medical, St. Paul, Minnesota), as described previously. Briefly, under fluoroscopic guidance, the pressure wire was advanced into the coronary artery to a position distal to the most distal lesion, and steady-state maximum hyperemia was induced by the continuous administration of 140 to 200 μg/kg/min adenosine into the large antecubital vein or central vein. During maximum hyperemia, the pressure wire was slowly pulled back from the distal coronary artery to the ostium of the coronary artery, thereby recording the mean aortic pressure (Pa), mean coronary pressure between the 2 lesions (Pm), and mean coronary pressure distal to the most distal lesion (Pd). Corresponding FFR values (FFRa = Pa/Pa = 1, FFRm = Pm/Pa, and FFRd = Pd/Pa) and FFR gradients (ΔFFR [A] = FFRa − FFRm, and ΔFFR [B] = FFRm − FFRd) at each point were also calculated ( Figure 1 ). Finally, the pressure wire was completely pulled back into the guiding catheter, and we verified that no drift had occurred during the procedure.
After completion of the FFR measurement along the entire coronary tandem lesion, the treatment strategy was determined on the basis of the measured FFR value. A coronary stenosis was considered functionally significant when the FFR of the lesion was ≤0.80. Therefore, all the coronary tandem lesions included in the present study were justified to be revascularized. Percutaneous coronary intervention (PCI) was first performed for any lesion that showed a large ΔFFR between 2 stenoses, as seen during the pullback of the pressure wire. Thereafter, FFR was reassessed for the remaining stenosis. If the FFR was ≤0.80, PCI was performed, and if the FFR was >0.80, PCI was deferred. PCI was performed using standard methods. Drug-eluting stent implantation was adopted as a default strategy under intravascular ultrasound guidance.
Clinical follow-up was performed at 1 month after the procedure and every 3 months thereafter. Adverse cardiac events were defined as death, myocardial infarction, and target vessel revascularization during the follow-up period.
Continuous variables are expressed as mean ± SD and categorical variables as numbers and percentages. Continuous variables were compared using Student’s t tests or Mann-Whitney U tests, and categorical variables were compared using chi-square or Fisher’s exact tests, as appropriate. Binary logistic regression analysis was performed to find the predictors of dual-lesion treatment. Among the hemodynamic and angiographic parameters, only the variables with p values <1.00 in univariate analysis were entered into the multivariate model, and backward stepping was used to determine the independent predictors. All p values were 2 sided, and p values <0.05 were considered statistically significant. All statistical analyses were performed using SPSS version 12.0 for Windows (SPSS, Inc., Chicago, Illinois).
Results
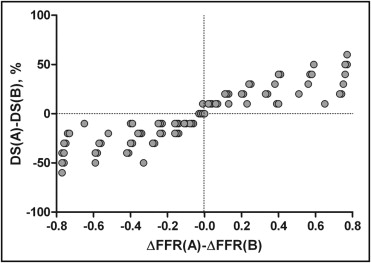
A total of 147 combinations of stenosis A and stenosis B were created. The change in FFR according to the differing stenosis severity of the other stenosis is shown in Figure 2 . Figure 3 plots the relation between the differences in diameter stenosis of stenoses A and B and the differences in ΔFFR (A) and ΔFFR (B). Furthermore, the experimental results of Pijls et al were plotted for the external validation of our simulated results in Supplemental Figure 1 . Figure 2 and Supplemental Figure 1 show that the lesion with a large ΔFFR is considered the lesion with the more functionally severe stenotic lesion.
From July 2009 to April 2011, a total of 52 consecutive patients with angiographically confirmed coronary tandem lesions were consecutively enrolled. The baseline demographic, angiographic, and procedural characteristics of all patients are listed in Table 1 . The mean patient age was 63 years, and 64% of our study patients were men. Most coronary tandem lesions (79%) included in our analysis were located in the left anterior descending coronary artery. The angiographically determined entire lesion length of the coronary lesions was approximately 49 mm.
| Variable | Value |
|---|---|
| Age (years) | 62.6 ± 9.0 |
| Men | 33 (64%) |
| Diabetes mellitus | 20 (39%) |
| Hypertension ⁎ | 24 (46%) |
| Hyperlipidemia † | 19 (37%) |
| Current smokers | 10 (19%) |
| Chronic renal failure ‡ | 2 (4%) |
| Left ventricular ejection fraction (%) | 60.9 ± 5.7 |
| Presentation | |
| Stable angina pectoris | 26 (50%) |
| Unstable angina pectoris | 23 (44%) |
| Acute myocardial infarction | 3 (6%) |
| Number of coronary arteries narrowed | |
| 1 | 11 (21%) |
| 2 | 15 (29%) |
| 3 | 26 (50%) |
| Location of narrowing of interest | |
| Left anterior descending coronary artery | 41 (79%) |
| Right coronary artery | 9 (17%) |
| Left circumflex coronary artery | 2 (4%) |
| Total lesion length (mm) | 49.0 ± 16.7 |
| Single-lesion treatment | 28 (54%) |
| Total stent length (mm) | 37.9 ± 16.4 |
| Total stent number per patient | 1.6 ± 0.7 |
| Minimal luminal diameter (mm) | 1.3 ± 0.3 |
| Mean reference vessel diameter (mm) | 3.0 ± 0.4 |
| Mean diameter stenosis (%) | 57.2 ± 9.6 |
| Maximal stent size (mm) | 3.4 ± 0.4 |
⁎ Systolic blood pressure >140 mm Hg, diastolic blood pressure >90 mm Hg, or receiving antihypertensive medication.
† Total cholesterol >200 mg/dl or receiving lipid-lowering treatment.
The correlation between the differences in diameter stenosis assessed by quantitative coronary angiography and the ΔFFR of the proximal and distal stenosis showed poor agreement (κ = 0.41). Disagreement between the 2 parameters was observed in 31% of patients with coronary tandem lesions ( Figure 4 ).
All FFR measurements were successfully performed. Coronary stents were sequentially implanted according to the results of the FFR measurements as described earlier. Figures 5 and 6 demonstrate representative cases for single-lesion and dual-lesion treatment, respectively. The treatment strategy and results are summarized in Figure 7 . The proximal lesion was treated first in 32 patients. Among a total of 104 stenoses, only 76 lesions (73.1%) were treated by 84 stent implantations. Revascularization for the remaining 28 lesions (26.9%) was deferred on the basis of FFR >0.80. Therefore, 28 patients (53.2%) were treated only by single-lesion treatment, after which the FFR of coronary tandem lesion recovered from 0.70 ± 0.05 to 0.86 ± 0.04 (p <0.001).




