Varicose veins
Varicose veins are dilated, tortuous veins that are engorged with blood. They result from improper venous valve function, and they may be primary, originating in the superficial veins, or secondary, occurring in the deep veins. Without treatment, varicose veins continue to enlarge.
Although there’s no cure, certain measures, such as walking and using compression stockings, can reduce the symptoms. Surgery may remove varicose veins, but the condition can occur in other veins.
CAUSES AND INCIDENCE
Primary varicose veins can arise from conditions that produce prolonged venous stasis or increased intra-abdominal pressure, such as pregnancy, obesity, constipation, or wearing tight clothes. They also may occur because of a congenital weakness of the valves or venous wall. Occupations that require standing for an extended period are another influential factor.
Secondary varicose veins may be caused by arteriovenous fistulas, deep vein thrombosis, occlusion, trauma to the venous system, or venous malformation.
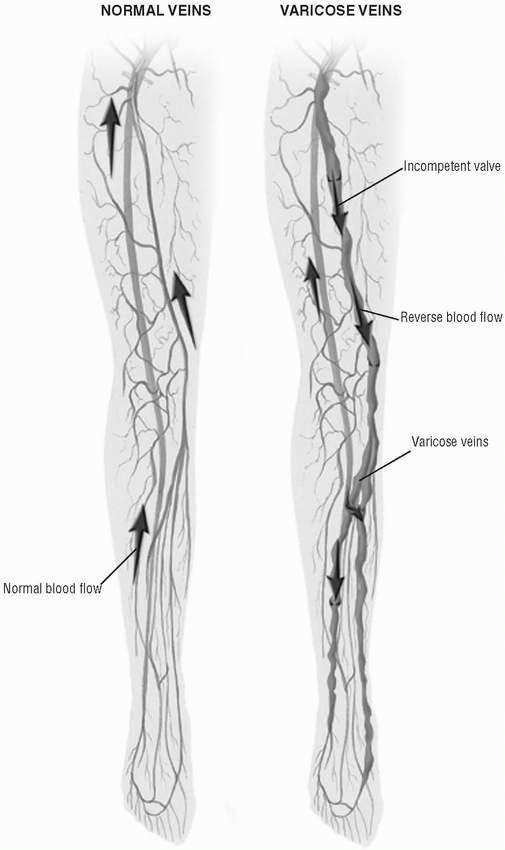
To understand the pathophysiology of varicose veins, remember that veins are thin-walled, distensible vessels with valves that keep blood flowing in one direction. Any condition that weakens, destroys, or distends these valves allows blood to flow backward to the previous valve. If a valve can’t hold the pooling blood, it can become incompetent, allowing even more blood to flow backward. As the volume of venous blood builds, pressure in the vein increases and the vein becomes distended. As the veins stretch, their walls weaken and lose elasticity, becoming enlarged, lumpy, and tortuous. As hydrostatic pressure increases, plasma is forced out of the veins and into the surrounding tissues, resulting in edema. (See
Vascular changes in varicose veins.)
People who stand for long periods may develop venous pooling because muscle contractions in the legs are inadequate to force blood back up to the heart. If valves in the veins are too weak to hold the pooling blood, they begin to leak, allowing blood to flow backward.
Primary varicose veins tend to be familial and to affect both legs; they’re twice as common in women as in men. They account for about 90% of varicose veins; 10% to 20% of Americans have primary varicose veins. Usually, secondary varicose veins occur in one leg. Both types are more common in middle adulthood.
SIGNS AND SYMPTOMS
Varicose veins typically appear as dilated, tortuous, purplish, ropelike veins, particularly in the calves. Edema of the calves and ankles may be present. The patient may complain of leg heaviness that worsens in the evening and in warm weather, dull aching in the legs after prolonged standing or walking, and aching during menses (as a result of increased fluid retention).
COMPLICATIONS
• Blood clots secondary to venous stasis
• Venous stasis ulcers
• Chronic venous insufficiency
DIAGNOSIS
• A manual compression test detects a palpable impulse when the vein is firmly occluded at least 8″ (20 cm) above the point of palpation, indicating incompetent valves in the vein.
• Trendelenburg’s test (retrograde filling test) shows incompetent deep and superficial vein valves.
• Photoplethysmography characterizes venous blood flow by showing changes in the skin’s circulation.
• Doppler ultrasonography reveals the presence or absence of venous backflow in deep or superficial veins.
• Venous outflow and reflux plethysmography shows deep venous occlusion, but this test is invasive and not routinely used.
• Ascending and descending venography demonstrates venous occlusion and patterns of collateral flow.
TREATMENT
Treatment should include management of the underlying cause of varicose veins, such as an abdominal tumor or obesity. Other supportive measures include use of antiembolism stockings or elastic bandages to counteract swelling by supporting veins and improving circulation and regular exercise to promote muscle contraction that forces blood through the veins and reduces venous pooling.
Surgical intervention may be needed for severe varicose veins. Methods include surgical stripping and ligation and phlebectomy. Phlebectomy involves removing the varicose vein through small incisions in the skin; it may be performed in an outpatient setting.
Drugs
• Injection of a sclerosing agent to treat small to medium varicosities
• Analgesics to manage pain post-operatively or after injection of a sclerosing agent
SPECIAL CONSIDERATIONS
• Discourage the patient from wearing constrictive clothing that interferes with venous return.
• Encourage an obese patient to lose weight to reduce intra-abdominal pressure.
• Tell the patient to elevate her legs above her heart whenever possible to promote venous return.
• Instruct the patient to avoid prolonged standing or sitting because
these actions enhance venous pooling.
• After surgery, check circulation often in the toes (color and temperature) and observe elastic bandages for bleeding. As ordered, rewrap bandages at least once per shift, wrapping from toe to thigh with the leg elevated.
Vasculitis
Vasculitis includes a broad spectrum of disorders characterized by inflammation and necrosis of blood vessels. Its clinical effects, which reflect tissue ischemia caused by obstructed blood flow, and confirming laboratory procedures depend on the vessels involved. The prognosis is variable. For example, hypersensitivity vasculitis usually is a benign disorder limited to the skin; more extensive polyarteritis nodosa can be rapidly fatal.
Vasculitis may occur at any age, except for mucocutaneous lymph node syndrome, which occurs only during childhood. Vasculitis may be a primary disorder or occur secondary to other disorders, such as rheumatoid arthritis or systemic lupus erythematosus.
CAUSES AND INCIDENCE
How vascular damage develops in vasculitis isn’t well understood. It has been linked to a history of serious infectious disease, such as hepatitis B or bacterial endocarditis, and high-dose antibiotic therapy. It may result from excessive circulating antigen that triggers formation of soluble antigen-antibody complexes. These complexes can’t be cleared effectively by the reticuloendothelial system, so they’re deposited in blood vessel walls (type III hypersensitivity). Increased vascular permeability from release of vasoactive amines by platelets and basophils enhances such deposition. The deposited complexes activate the complement cascade, resulting in chemotaxis of neutrophils, which release lysosomal enzymes. In turn, these enzymes cause vessel damage and necrosis, which may trigger thrombosis, occlusion, hemorrhage, and ischemia.
Another mechanism that may contribute to vascular damage is the cell-mediated (T-cell) immune response, in which circulating antigen triggers release of soluble mediators by sensitized lymphocytes, which attracts macrophages. The macrophages release intracellular enzymes, which cause vascular damage. They can also transform into the epithelioid and multinucleated giant cells that typify the granulomatous vasculitides. Phagocytosis of immune complexes by macrophages enhances granuloma formation.