The Thrombolysis In Myocardial Infarction (TIMI) score and Global Registry of Acute Coronary Events (GRACE) score have been validated as predictors of major adverse cardiovascular events (MACE) in patients with acute myocardial infarction (AMI). This study was undertaken to determine whether the CHADS 2 score had good accuracy for predicting clinical outcome in patients with AMI and to compare the discriminatory performance of the 3 risk scores (RSs). We calculated the TIMI RS, GRACE RS, and CHADS 2 score for 747 consecutive patients with AMI. The study end point was the combined occurrence of MACE, including death, nonfatal myocardial infarction, and ischemic stroke. All patients were followed up for at least 3 years or until the occurrence of a major event. The area under the receiver operating characteristic curve was used to evaluate the predictive ability of each score at different time points. Higher CHADS 2 scores were associated with adverse outcome at discharge and 1-year and 3-year follow-ups (chi-square test for linear trend, p <0.001). Both CHADS 2 score and GRACE RS demonstrated better discrimination than TIMI RS in predicting 1-year and 3-year MACE (p <0.001). Multivariate Cox regression analysis revealed that the CHADS 2 score was an independent predictor of future MACE in patients with AMI (hazard ratio 1.349, 95% confidence interval 1.196 to 1.522). In conclusion, the CHADS 2 score provides potentially valuable prognostic information on clinical outcome when applied to patients with AMI.
Highlights
- •
The CHADS 2 score is easy to calculate at the bedside and includes clinical data that are routinely available in the coronary care unit.
- •
The CHADS 2 score provides significant discriminatory ability for predicting major adverse cardiovascular events in patients with acute myocardial infarction (AMI).
- •
Compared with the Thrombolysis In Myocardial Infarction risk score and the Global Registry of Acute Coronary Events risk score, the CHADS 2 score is simpler and more practical for predicting clinical outcome when applied to patients with AMI.
- •
Use of the CHADS 2 score is an acceptable method for risk stratification and prognosis of patients with AMI.
The CHADS 2 score (i.e., congestive heart failure, hypertension, age >75 years, diabetes, and previous stroke and/or transient ischemic attack [TIA]) is used for embolic risk stratification and guidance in the management of patients with atrial fibrillation (AF). In addition, the CHADS 2 score seems to have an impact on all-cause mortality after stroke. Henriksson et al showed that the CHADS 2 score can provide valuable insight for other outcome variables apart from having had an ischemic stroke and can be applied to patients with different risk factor profiles, for example, with a previous known cardiovascular disease but without known AF. A recent study demonstrates that the CHADS 2 score may help to identify patients with acute coronary syndrome (ACS) with high risk for a subsequent stroke or death and a need for enhanced risk-reducing treatment. However, the suitability of the CHADS 2 score for prognostic stratification in patients with acute myocardial infarction (AMI) remains uncertain. The Thrombolysis In Myocardial Infarction (TIMI) score and Global Registry of Acute Coronary Events (GRACE) score have been validated as predictors of cardiovascular events in patients with AMI. The main limitation of both risk scores (RSs) is their apparent “complexity” compared with CHADS 2 risk model. The aims of this study were to determine whether the CHADS 2 score, when applied to a cohort of patients with AMI, would show good accuracy for predicting clinical outcome and to compare the in-hospital and long-term prognostic accuracy of the 3 RSs.
Methods
This was a retrospective study of consecutive patients with AMI admitted to a coronary care unit from May 2002 to December 2005. AMI was defined as detection of elevated troponin I level ≥0.1 ng/ml, accompanied by either typical chest pain for >30 minutes and/or electrocardiographic changes (including ischemic ST-segment depression, ST-segment elevation, or pathologic Q waves). Before enrollment, each patient’s chart was reviewed in detail to gather data on symptoms, medications, coronary risk factors, previous cardiac events, smoking status, and other systemic diseases. Serum creatinine levels >2 mg/dl were classified as renal insufficiency. Smokers were classified as former smokers only if they had not smoked for >6 months. To reduce patient selection bias, there was no age limit or other specific exclusion criteria. The study was approved by the Research Ethics Committee of Taipei Veterans General Hospital.
The TIMI and GRACE RSs were calculated on the basis of the initial clinical history, electrocardiogram, and laboratory values collected on admission. The CHADS 2 score was calculated for each patient by assigning 1 point each for ages >75 years, hypertension, diabetes mellitus, and heart failure and 2 points for a previous stroke or TIA. The study patients were divided into 3 groups according to their CHADS 2 scores: group 1, score 0; group 2, score 1 to 2; and group 3, score 3 to 6. These cut-off values were determined according to a previous study on the risk of stroke.
All patients included in the study were followed up for at least 3 years or until the occurrence of a major event. The study end point was the combined occurrence of major adverse cardiovascular events (MACE), including death, nonfatal myocardial infarction, and ischemic stroke. All study subjects were contacted by telephone periodically and their medical records were followed up regularly. Nonfatal myocardial infarction was defined by an increase of cardiac troponin I (≥0.1 ng/ml) with ischemic symptoms or characteristic electrocardiographic changes. Ischemic stroke was defined as the presence of a new neurological deficit lasting for at least 24 hours with definite evidence of a cerebrovascular accident verified by either magnetic resonance imaging or computed tomography. The end point was analyzed at the time of discharge, 1 year, and 3 years.
Data are expressed in terms of mean and SD for numeric variables and as number (percent) for categorical variables. Comparisons of continuous variables among groups were performed by the Student t test. Subgroup comparisons of categorical variables were assessed by the chi-square or Fisher’s exact test. For each of the 3 RSs, receiver operating characteristic curves were used to relate the calculated scores to the rate of adverse clinical events at discharge, 1 year, and 3 years. The area under the receiver operating characteristic curve (AUC) or C-statistic was used as a measure of the predictive accuracy of the RS. The relative performance of each test was evaluated with a 95% confidence interval for the difference between 2 AUCs. The statistical significance of the difference between 2 AUCs was tested with the method of DeLong et al. The method of Bonferroni correction was used to counteract the problem of multiple comparisons. Survival curves were generated by the Kaplan-Meier method, and survival among groups was compared by the use of log-rank test. Multivariate Cox regression analysis was performed to determine the independent predictors of future MACE. Variables significantly associated with MACE were entered into the multivariate model. Data were analyzed using SPSS version 17.0 (SPSS Inc., Chicago, Illinois) and MedCalc version 12.3.0 (MedCalc Software, Mariakerke, Belgium). A p value <0.05 was considered to indicate statistical significance.
Results
A total of 747 consecutive patients (598 men, 82%) were enrolled in this study. All study subjects were followed up until May 2010. Overall, the mean delay between symptom onset and hospital admission was 4.5 hours, with a significant difference (p = 0.027) between ST-segment elevation myocardial infarction (4.2 hours) and non–ST-segment elevation myocardial infarction (4.9 hours). The baseline characteristics of all patients are listed in Table 1 . The mean age of our cohort was 67 ± 12 years. Among the subjects, 64.4% had hypertension, 36.8% had diabetes mellitus, 18.6% had renal insufficiency, 12.0% had a previous stroke and/or TIA, 6.7% had congestive heart failure, and 3.1% had AF. Oral anticoagulation therapy was used in 39% of patients with AF. Patients with high CHADS 2 scores tended to be older, with more co-morbidities, and were less likely to undergo revascularization during index hospitalization than those with low CHADS 2 scores.
| Variable | CHADS 2 0 (n = 157) | CHADS 2 1–2 (n = 427) | CHADS 2 ≥3 (n = 163) | p |
|---|---|---|---|---|
| Age (years) | 59.4 ± 11.1 | 67.1 ± 11.8 | 75.9 ± 7.7 | <0.001 |
| Men | 143 (91.1%) | 342 (80.1%) | 113 (69.3%) | <0.001 |
| Current smoker | 98 (62.4%) | 183 (42.9%) | 37 (22.7%) | <0.001 |
| Hypertension | 0 | 324 (75.9%) | 157 (96.3%) | <0.001 |
| Diabetes mellitus | 0 | 162 (37.9%) | 113 (69.3%) | <0.001 |
| Hypercholesterolemia | 18 (11.5%) | 86 (20.1%) | 29 (17.8%) | 0.052 |
| Renal insufficiency | 10 (6.4%) | 80 (18.8%) | 49 (30.1%) | <0.001 |
| Previous coronary intervention | 8 (5.1%) | 47 (11.0%) | 26 (16.0%) | 0.008 |
| Previous coronary bypass | 3 (1.9%) | 18 (4.2%) | 11 (6.7%) | 0.101 |
| Previous myocardial infarction | 10 (6.4%) | 52 (12.2%) | 20 (12.3%) | 0.115 |
| Previous stroke/TIA | 0 | 4 (0.9%) | 86 (53.1%) | <0.001 |
| Heart failure | 0 | 17 (4.0%) | 33 (20.2%) | <0.001 |
| Atrial fibrillation | 3 (1.9%) | 11 (2.6%) | 9 (5.5%) | 0.147 |
| Ejection fraction (%) | 47.4 ± 14.1 | 43.5 ± 13.5 | 42.1 ± 13.5 | 0.010 |
| Killip classification | <0.001 | |||
| Killip = 1 | 116 (73.9%) | 243 (56.9%) | 58 (35.6%) | |
| Killip >1 | 41 (26.1%) | 184 (43.1%) | 105 (64.4%) | |
| In-hospital revascularization | <0.001 | |||
| Coronary intervention | 120 (76.4%) | 234 (54.8%) | 46 (28.2%) | |
| Coronary bypass | 8 (5.1%) | 47 (11.0%) | 20 (12.3%) | |
| Medication use at discharge | ||||
| Antiplatelet | 156 (99.4%) | 423 (99.1%) | 159 (97.5%) | 0.376 |
| β-Blocker | 7 (4.5%) | 132 (30.9%) | 71 (43.6%) | <0.001 |
| ACE inhibitor | 6 (3.8%) | 115 (26.9%) | 56 (34.4%) | <0.001 |
| A II receptor blocker | 1 (0.6%) | 61 (14.3%) | 32 (19.6%) | <0.001 |
| Statin | 68 (43.3%) | 187 (43.8%) | 59 (36.2%) | 0.231 |
| CHADS 2 score | 0 | 1.46 ± 0.50 | 3.56 ± 0.70 | <0.001 |
A total of 313 cases of MACE occurred, including 220 cases of death, 65 cases of nonfatal myocardial infarction, and 28 cases of ischemic stroke. Figure 1 illustrates the in-hospital, 1-year, and 3-year MACE by patient risk groups. Higher risk categories were associated with adverse outcome at discharge, 1 year, and 3 years (chi-square test for linear trend, p <0.001). The increase in 1 point of CHADS 2 score was associated with a 51%, 70%, and 91% significant increase in in-hospital, 1-year, and 3-year MACE, which resulted in odds ratios (95% confidence interval) of 1.51 (1.25 to 1.82), 1.70 (1.47 to 1.95), and 1.91 (1.67 to 2.20), respectively.
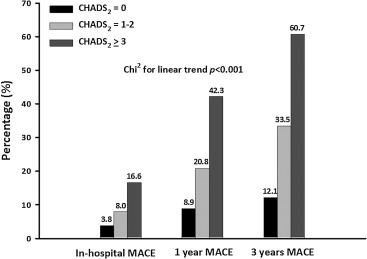
As listed in Table 2 , the incidence of MACE was significantly higher in patients with high CHADS 2 scores compared with that in patients with low CHADS 2 scores (68.1% vs 16.6%, p <0.001). To determine the relation between survival free of adverse events and CHADS 2 scores, Kaplan-Meier survival analysis was performed. Patients with high CHADS 2 scores had significantly reduced MACE-free survival rate than those with low CHADS 2 scores (p <0.001), as illustrated in Figure 2 .
| Variable | CHADS 2 Score | p | ||
|---|---|---|---|---|
| 0 (n = 157) | 1–2 (n = 427) | ≥3 (n = 163) | ||
| Nonfatal MI | 6 (3.8%) | 38 (8.9%) | 21 (12.9%) | 0.016 |
| Ischemic stroke | 1 (0.6%) | 16 (3.7%) | 11 (6.7%) | 0.016 |
| Cardiovascular death | 6 (3.8%) | 79 (18.5%) | 48 (29.4%) | <0.001 |
| All-cause death | 19 (12.1%) | 122 (28.6%) | 79 (48.5%) | <0.001 |
| MACE (death/MI/stroke) | 26 (16.6%) | 176 (41.2%) | 111 (68.1%) | <0.001 |

Table 3 lists the AUC for the 3 RSs in predicting in-hospital, 1-year, and 3-year MACE, respectively. The TIMI RS, GRACE RS, and CHADS 2 score were able to discriminate patients with AMI with and without MACE at different time points up to 3 years. The discriminatory performance of the 3 RSs in predicting the risk of in-hospital MACE was not significantly different. Both CHADS 2 score and GRACE RS demonstrated better discrimination than TIMI RS in predicting MACE at 1 year and 3 years (p <0.001, respectively), but there was no difference between the CHADS 2 score and GRACE RS, as listed in Table 4 .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


