Although we strive to achieve complete revascularization (CR) in those receiving percutaneous coronary intervention, it is uncertain which of these patients are at increased risk of clinical events. In this study, we aimed to investigate whether the baseline SYNTAX score (bSS) can predict adverse clinical events in patients receiving CR. From the Efficacy of Xience/Promus Versus Cypher in Reducing Late Loss After Stenting registry, the 3-year patient-oriented composite end point (POCE; all cause death, any myocardial infarction, and any revascularization) was compared according to bSS tertiles (1 ≤ low bSS < 6, 6 ≤ mid-bSS < 10, high bSS ≥ 10). Of the 5,088 patients, CR was achieved in 2,173 by percutaneous coronary intervention. The 3-year POCE increased significantly along with bSS tertile (7.3% vs 8.4% vs 14.8%, p <0.001). Multivariate analysis showed that, despite having the same residual SS of 0, the bSS was an independent predictor of 3-year POCE (hazard ratio 1.038, 95% confidence interval 1.018 to 1.058, p <0.001 per bSS point). In subgroup analysis, bSS was a predictor for 3-year POCE in multivessel diseases (hazard ratio 1.029, 95% confidence interval 1.004 to 1.054, p = 0.025 per bSS point), whereas in single-vessel diseases, the discriminative value of bSS was less significant. Also the clinical SYNTAX score, which added age, creatinine level, and ejection fraction to the bSS, was superior to the bSS in predicting 3-year POCE (area under the curve 0.595 vs 0.649, p = 0.008). In conclusion, the bSS was an independent predictor of long-term clinical outcomes in patients receiving CR, especially in those with multivessel coronary artery disease. Adding clinical factors to the bSS could increase the predictive power of clinical outcomes.
Complete revascularization (CR), defined as revascularization of all diseased coronary artery segments, can often be achieved leading to improved clinical outcome in patients with coronary artery disease. In addition, the degree of incompleteness of revascularization was correlated with an incremental increase in adverse events. The beneficial effect of CR is thought to be from reduction or elimination of ischemia. Despite the benefits of CR, it is unknown which subgroup of patients will fare well and which are at increased risk of adverse events in the long term. In the present study, using the SYNTAX score (SS), we examined whether the baseline SYNTAX score (bSS) could predict clinical outcomes in those who received CR.
Methods
Extended description of study methods is presented in the online Supplementary Appendix .
The Efficacy of Xience/Promus Versus Cypher in Reducing Late Loss After Stenting (EXCELLENT) registry was a multicenter registry enrolling patients from 29 centers in Korea to compare the efficacy of everolimus-eluting stents (Xience/Promus) versus sirolimus-eluting stents (SES; Cypher) in all comers who underwent percutaneous coronary intervention (PCI) with unrestricted drug-eluting stent use. The study protocol was approved by the ethics committee at each participating center and was conducted according to the principles of the Declaration of Helsinki. All patients provided written informed consent for participation in the registry.
Independent quantitative analysis of baseline coronary angiographic images and calculation of the SS were performed by 3 specialized quantitative coronary angiography technicians at the Seoul National University Hospital Cardiovascular Clinical Research Center Angiographic Core Laboratory. CR was defined as a residual SS of 0. For calculation of the clinical SYNTAX score (cSS), the SS was multiplied with the value of the modified “Age, Creatinine, and Left Ventricular Ejection Fraction (ACEF)” score, which was retrospectively calculated, based on the patients’ left ventricular ejection fraction, age, and creatinine clearance derived using the Cockcroft-Gault equation.
The primary analysis end point was the 3-year patient-oriented composite end point (POCE). POCE was defined as a composite of all-cause death, any myocardial infarction (MI, including nontarget vessel territory), and any repeat revascularization (including all target and nontarget vessels, regardless of percutaneous or surgical methods). Secondary analysis end points were target lesion failure (TLF, a composite of cardiac death, target-vessel MI, and target lesion revascularization) and the individual components of the 3-year POCE.
Data are presented as numbers and frequencies for categorical variables and as mean ± SD for continuous variables. For comparison among groups, chi-square test for categorical variables and unpaired Student’s t test or 1-way ANOVA for continuous variables was applied. To estimate the independent effect of bSS on clinical outcome, a multivariable Cox proportional hazards regression model was used. The Kaplan-Meier event curves were drawn up to 36 months, and the log-rank test was used to analyze the significance in difference of clinical outcomes. Area under the curve of receiver-operating characteristic curves for bSS and cSS were performed. A 2-sided probability value <0.05 was considered statistically significant. Statistical tests were performed using SPSS, V.18 (SPSS, Inc., Chicago, Illinois).
Results
The all-comer EXCELLENT registry enrolled 5,159 patients, from which 71 patients (1.4%) had uninterpretable post-PCI angiographic images, leaving 5,088 patients (98.3%) with bSS and residual SS values. The SS was significantly reduced after PCI (13.6 ± 9.1 to 4.7 ± 6.5, p <0.05). CR was achieved in 2,173 patients (42.7%) and the bSS of these patients was 8.5 ± 6.3. Patients receiving CR were divided into approximate tertiles, according to bSS: 832 patients (38.3%) in low bSS (1 ≤ bSS < 6, mean: 3.5 ± 1.4), 692 patients (31.8%) in mid-bSS (6 ≤ bSS < 10, mean: 7.5 ± 1.0), and 649 patients (29.9%) in high bSS (bSS ≥ 10, mean: 16.2 ± 5.5). The baseline clinical and angiographic characteristics of patients in each tertile are summarized in Table 1 , and lesion characteristics are summarized in Supplementary Table 1 .
| Variable | Baseline SYNTAX score | P value | ||
|---|---|---|---|---|
| 1≤ – <6 (n=832) | 6≤ – <10 (n=692) | ≥10 (n=649) | ||
| Age (years) | 61.7±10.6 | 60.4±11.1 | 61.9±11.6 | 0.657 |
| Body Mass index (kg/m 2 ) | 25.01±3.93 | 24.81±3.04 | 24.61±3.07 | 0.029 |
| Male | 520 (67.4%) | 481 (69.5%) | 469 (72.3%) | 0.050 |
| Previous Percutaneous coronary intervention | 122 (15.8%) | 79 (11.4%) | 88 (13.6%) | 0.925 |
| Previous Coronary artery bypass graft surgery | 6 (0.8%) | 3 (0.4%) | 13 (2.0%) | 0.031 |
| Previous Myocardial infarction | 55 (7.1%) | 38 (5.5%) | 53 (8.2%) | 0.778 |
| Previous Cerebrovascular accident | 41 (5.3%) | 23 (3.3%) | 42 (6.5%) | 0.719 |
| Previous chronic heart failure | 12 (1.6%) | 7 (1.0%) | 10 (1.5%) | 0.903 |
| Peripheral Vascular Disease | 6 (0.8%) | 5 (0.7%) | 5 (0.8%) | 0.839 |
| Diabetes Mellitus | 246 (31.9%) | 171 (24.7%) | 230 (35.4%) | 0.223 |
| Hypertension | 474 (61.5%) | 386 (55.8%) | 348 (53.6%) | 0.002 |
| Chronic renal failure | 14 (1.8%) | 15 (2.2%) | 17 (2.6%) | 0.304 |
| Dyslipidemia | 296 (38.4%) | 246 (35.5%) | 222 (34.2%) | 0.921 |
| Smoking ∗ | 31.3% / 17.4% / 49.2% | 29.2% / 19.8% / 48.6% | 35.7% / 16.5% / 45.9% | 0.599 |
| Chronic obstructive pulmonary disease | 26 (3.4%) | 21 (3.0%) | 19 (2.9%) | 0.626 |
| Family history of Coronary artery disease | 30 (3.9%) | 43 (6.2%) | 35 (5.4%) | 0.163 |
| Ejection fraction | 62.2±9.7 % | 61.6±10.0 % | 57.5±12.0 % | <0.001 |
| Clinical diagnosis † | 39.7% / 42.5% / 8.6% / 9.3% | 37.6% / 40.5% / 9.8% / 12.1% | 29.0% / 34.4% / 11.0% / 25.7% | <0.001 |
| Acute coronary syndrome | 489 (60.4%) | 427 (62.4%) | 459 (71.1%) | <0.001 |
| Number of Vessel disease ‡ | 75.8% / 18.9% / 5.3% | 70.1% / 23.1% / 6.8% | 40.7% / 39.2% / 20.1% | <0.001 |
| Total stent length (mm) | 23.8±8.9 | 24.9±10.8 | 30.5±16.2 | <0.001 |
| Number of stents per lesion | 1.1±0.3 | 1.1±0.4 | 1.3±0.6 | <0.001 |
| Number of stents per patient | 1.1±0.3 | 1.2±0.5 | 1.7±0.8 | <0.001 |
| Laboratory tests | ||||
| WBC ( /μL) | 7640±2740 | 7230±2950 | 8450±3380 | <0.001 |
| Hemoglobin (g/dL) | 13.7±1.8 | 13.8±1.8 | 13.8±2.8 | 0.193 |
| Total cholesterol (mg/dL) | 174±44 | 181±64 | 179±44 | 0.087 |
| Triglyceride (mg/dL) | 145±94 | 142±94 | 148±106 | 0.542 |
| Low density lipoprotein (mg/dL) | 105±37 | 110±60 | 110±41 | 0.064 |
| High density lipoprotein (mg/dL) | 44±12 | 44±12 | 43±17 | 0.099 |
| Creatinine (mg/dL) | 1.04±0.78 | 1.10±1.11 | 1.08±0.75 | 0.334 |
| C reactive protein (mg/dL) | 3.20±18.61 | 4.82±34.16 | 6.23±35.62 | 0.114 |
∗ Smoking: Current/ex-/never smoker.
† Clinical diagnosis: Stable angina, Unstable angina, Non-ST elevation myocardial infarction, ST elevation myocardial infarction.
‡ Number of vessel disease: 1 vessel disease/2 vessel disease/3 vessel disease.
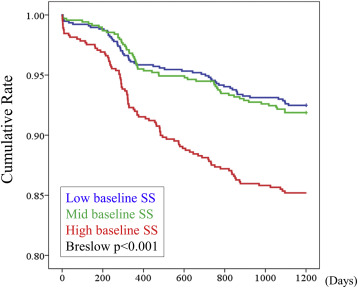
A total of 217 clinical events (10.0%) occurred in patients receiving CR over the 3 years. Three-year POCE significantly increased according to bSS tertile ( Table 2 ). For the secondary analysis end points, all end points occurred more frequently as bSS increased except MI, for which the incremental increase was insignificant. Also the cumulative Kaplan-Meier event curves for 3-year POCE showed statistically significant difference between the low, mid, and high bSS groups ( Figure 1 ). Among the POCE events, 121 (55.8%) were target lesion-related and 96 (44.2%) were nontarget lesion-related POCE events. Also repeat revascularization occurred in 135 cases (62.2%), of which 82 (60.7%) were target lesion revascularization. Nontarget lesion-related events comprised around 40% of all 3-year events, and both non-TLF and non-target lesion revascularization events increased with bSS tertile. After adjustment for possible confounding covariates, such as age, gender, clinical diagnosis, body mass index, diabetes mellitus, hypertension, dyslipidemia, ejection fraction, and WBC count using a Cox proportional hazard model, bSS tertile was an independent predictor for 3-year POCE (p for trend <0.001, Table 3 ). This trend was mainly driven by the event discrimination between the mid and high bSS group.
| Variable | 1≤ baseline SYNTAX score <6 (n=832) | 6≤ baseline SYNTAX score <10 (n=692) | baseline SYNTAX score ≥10 (n=649) | P value |
|---|---|---|---|---|
| 3-year POCE ∗ | 61 (7.3%) | 58 (8.4%) | 98 (15.1%) | <0.001 |
| All cause death | 25 (3.0%) | 20 (2.9%) | 36 (5.5%) | 0.014 |
| Cardiac death | 12 (1.4%) | 12 (1.7%) | 18 (2.8%) | 0.070 |
| Revascularization | 35 (4.2%) | 38 (5.5%) | 62 (9.6%) | <0.001 |
| Target lesion revascularization | 23 (2.8%) | 23 (3.3%) | 36 (5.5%) | 0.015 |
| Non-target lesion revascularization | 12 (1.4%) | 15 (2.2%) | 26 (4.0%) | 0.006 |
| Myocardial infarction | 2 (0.3%) | 3 (0.4%) | 4 (0.6%) | 0.533 |
| Target lesion failure † | 34 (4.1%) | 33 (4.8%) | 54 (8.3%) | 0.001 |
| Non-Target lesion failure | 27 (3.2%) | 25 (3.6%) | 44 (6.8%) | 0.002 |
∗ POCE: patient oriented composite endpoint, including all cause death, all cause myocardial infarction and revascularization.
† Target lesion failure: cardiac death, target vessel myocardial infarction, target lesion revascularization.
| Variable | Hazard ratio (95% Confidential Interval) | P value |
|---|---|---|
| Age (> 65 years) | 1.537 (1.161-2.035) | 0.003 |
| Diabetes Mellitus | 1.467 (1.099-1.956) | 0.009 |
| Ejection fraction (<55%) | 1.388 (1.004-1.920) | 0.047 |
| Body mass Index <25 kg/m 2 | 1.397 (1.045-1.867) | 0.024 |
| Baseline SS by tertile ∗ | <0.001 | |
| Low bSS vs. mid bSS | 1.236 (0.849-1.799) | 0.269 |
| Mid bSS vs. High bSS | 1.595 (1.130-2.252) | 0.008 |
| Low bSS vs. High bSS | 1.970 (1.401-2.770) | <0.001 |
| Baseline SS (per point) ∗ | 1.038 (1.018-1.058) | <0.001 |
∗ A multivariable Cox proportional hazards regression model was analyzed twice; once, using the baseline SS by tertile and second, using the baseline SS by point.
Within the entire EXCELLENT registry, 2,260 patients had single-vessel disease, of which 1,334 patients (59.0%) achieved CR. The other 2,828 patients had left main or multivessel disease and among them, 839 patients (29.7%) achieved CR. Therefore, among the patients receiving CR, 61.4% had single-vessel disease and 38.6% had left main or multivessel disease. Three-year POCE occurred about twice as much often in the left main or multivessel disease group (111 [13.2%] vs 106 cases [7.9%], p <0.001). When divided into tertiles according to bSS, bSS had marginal significance in predicting 3-year POCE in the single-vessel disease group. Incidence of other secondary end points increased nominally according to bSS tertile, but the difference was not statistically significant. However, in the left main or multivessel disease group, 3-year POCE events significantly increased with increasing bSS tertile, which was mainly driven by revascularization ( Table 4 ). Kaplan-Meier event curves also showed higher 3-year POCE rates in the high bSS tertile in both single-vessel disease and left main or multivessel disease group, where the discriminative value of bSS tertile was superior in the left main or multivessel disease group ( Figure 2 ). By the Cox proportional hazard model, bSS was an independent predictor of 3-year POCE only in the left main or multivessel disease group (hazard ratio 1.029, 95% confidence interval 1.004 to 1.054, p = 0.025 per bSS point).
| Baseline SYNTAX score | P value | |||
|---|---|---|---|---|
| 1≤ – <6 | 6≤ – <10 | ≥10 | ||
| Single Vessel Disease Group | (n=628) | (n=476) | (n=230) | |
| 3-year POCE ∗ | 43 (6.8%) | 36 (7.6%) | 27 (11.7%) | 0.059 |
| All cause death | 17 (2.7%) | 16 (3.4%) | 10 (4.3%) | 0.473 |
| Revascularization | 25 (4.0%) | 21 (4.4%) | 17 (7.4%) | 0.105 |
| Target lesion revascularization | 19 (3.0%) | 16 (3.4%) | 11 (4.8%) | 0.454 |
| Myocardial infarction | 2 (0.3%) | 1 (0.2%) | 2 (0.9%) | 0.385 |
| Target lesion failure † | 27 (4.3%) | 23 (4.8%) | 16 (7.0%) | 0.280 |
| Left main or multivessel disease group | (n=204) | (n=216) | (n=419) | |
| 3-year POCE ∗ | 18 (8.8%) | 22 (10.2%) | 71 (16.9%) | 0.006 |
| All cause death | 8 (3.9%) | 4 (1.9%) | 26 (6.2%) | 0.039 |
| Revascularization | 10 (4.9%) | 17 (7.9%) | 45 (10.7%) | 0.046 |
| Target lesion revascularization | 4 (2.0%) | 7 (3.2%) | 25 (6.0%) | 0.046 |
| Myocardial infarction | 0 (0.0%) | 2 (0.9%) | 2 (0.5%) | 0.388 |
| Target lesion failure † | 7 (3.4%) | 10 (4.6%) | 38 (9.1%) | 0.012 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


