Atrial fibrillation (AF) can be a potentially life-threatening arrhythmia when it conducts rapidly through the accessory pathway, which was not predicted by the noninvasive method. We evaluated the cardiac sympathetic activity for predicting the occurrence of AF in patients with Wolff-Parkinson-White (WPW) syndrome. Iodine-123 metaiodobenzylguanidine scintigraphy was performed under stable sinus rhythm conditions at rest <1 week before an electrophysiologic study (EPS) to assess the sympathetic activity using the heart/mediastinum (H/M) ratio in 45 consecutive patients with WPW who had a history of supraventricular tachycardia (mean ± SD, age: 47 ± 17 years, 42.2% women). The study also included 15 normal healthy volunteers (56 ± 17 years, 40% women). The H/M ratio was lower in patients with WPW syndrome than in the normal control group, and in the 15 patients with AF induced during EPS than in the 30 patients without AF (p <0.0001). The sensitivity of H/M ratio ≤2.8 for predicting the AF induced during EPS was 75% in 12 of 16 patients, and the specificity was 89.7% in 26 of 29 patients. The H/M ratio was positively correlated with anterograde effective refractory period (r = 0.514, p <0.0001). The sensitivity of H/M ratio ≤2.75 for predicting the AF with a short anterograde effective refractory period (≤250 ms) was 91.7% in 11 of 12 patients, and the specificity was 90.9% in 30 of 33 patients. In conclusion, the severe cardiac sympathetic dysfunction was associated with the occurrence of AF, particularly in those with rapid AF and in patients with WPW syndrome.
Sympathetic hyperinnervations are the most common triggers of supraventricular tachycardia (SVT) and atrial fibrillation (AF), and specific patterns of autonomic nerve discharge have been experimentally reported to differentiate between AF and SVT. On the condition of sympathetic hyperinnervation, the increased spillover of norepinephrine from the sympathetic nervous system in the skeletal muscle and heart leads to the increased plasma concentration and depleted stores in the heart. Therefore, using the radiotracer iodine-123 metaiodobenzylguanidine (I-123 MIBG), which is taken up into presynaptic cardiac sympathetic nerves, the cardiac sympathetic dysfunction as a low uptake of I-123 MIBG has been reported in patients with SVT or AF. SVT can be potentially life threatening because it is associated with a rapid AF through the accessory pathway (AP) in Wolff-Parkinson-White (WPW) syndrome. However, the noninvasive tests currently play only a small role in evaluating the life-threatening SVT before an invasive electrophysiologic study (EPS). We hypothesized that severe cardiac sympathetic dysfunction would be associated with the occurrence of AF in patients with WPW syndrome who had a history of SVT.
Methods
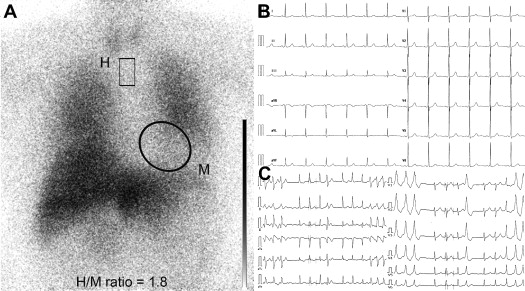
We studied patients with manifest WPW syndrome at Showa University Hospital. Tachyarrhythmia was found on the basis of SVT documented by ambulatory electrocardiography, 12-lead electrocardiography, and Holter monitoring. The left ventricular ejection fraction was measured by 2-dimensional echocardiography before the study, and the anteroposterior left atrial dimension (LAD) was measured from the parasternal long axis using M-mode echocardiography. In the present study, 15 normal healthy volunteers were also recruited for the control group (56 ± 17 years, 40% women). All the patients provided written informed consent before the study, and the protocol was approved by our Institutional Review Board. In the 45 consecutive patients with manifest WPW syndrome (51 ± 19 years, 46.6% women) who did not have the structural heart disease, I-123 MIBG scintigraphy was performed during stable sinus rhythm to assess cardiac sympathetic activity within the week before EPS. After intravenous injection of 111 MBq of I-123 MIBG (Dai-ichi Radioisotope Laboratory, Chiba, Japan), the myocardial planner images were acquired with 4-hour delayed images using a standard-field gamma camera equipped with a medium energy, parallel-hole collimator (PRIZM 2000XP, Picker/Philips Co., Cleveland, Northwest Ohio). A 20% window centered at 159 keV was used. To evaluate the myocardial accumulation of I-123 MIBG, the heart/mediastinal (H/M) activity ratio was calculated from the delayed image ( Figure 1 ). To measure C-reactive protein and plasma brain natriuretic peptide levels, blood samples were obtained before I-123 MIBG scintigraphy.
EPS was performed with at least 4 catheters positioned in the right atrium, right ventricular apex, His bundle region, and coronary sinus. Incremental atrial pacing was performed until the highest rate conducted 1/1 through the AP and/or atrioventricular node. Atrial stimulation was programmed (Cardiac Stimulator BC-1100, Fukuda Denshi Co., Tokyo, Japan) at a basic cycle length of 600 ms and 400 ms with the introduction of 1 and 2 extra stimuli. If the AP was observed, additional atrial and ventricular stimulations were performed with progressively shorter coupling intervals at drive-cycle lengths of 400 ms and 350 ms to induce SVT until the effective refractory periods (ERP) of the atrium and ventricle were achieved. Inducible arrhythmias were defined as sustained if they lasted >1 minute. The AF was considered to be induced during EPS by incremental atrial pacing or atrial extrastimulation, and the ERP of preexisted beats was measured. The inducibility was also assessed at baseline or after isoproterenol infusion with atrial pacing and was defined as a reproducible induction of sustained SVT or AF, according to a previous study. The anterograde ERP of an AP was defined as the longest coupling interval in which an anterograde block in the bypass tract was observed.
Continuous variables were presented as the mean ± SD. Differences between the groups were tested using an unpaired t test, a chi-square test, or Fisher’s exact test, as appropriate. The associations between the predictors and AF were formally tested by constructing a multivariate logistic regression analysis. The induction of rapid AF with a short anterograde ERP, which was defined as ≤250 ms (the ventricular rate ≥240 beats/min), through an anterograde AP conduction, was considered to be a life-threatening SVT, according to the American Heart Association/American College of Cardiology/European Society of Cardiology guideline. All the multivariate analyses used the forward stepwise method with the entry and removal p values set at 0.5. A receiver operating characteristic analysis was performed to define the cut-off values. This analysis provided the optimal sensitivity and specificity in predicting the AF. The statistical analysis was performed using IBM SPSS for Windows version 20 (SPSS Inc., an IBM Company, Chicago, Illinois).
Results
The H/M ratio was lower in the 45 patients with WPW than in the 15 patients within the control group (p <0.0001) ( Table 1 ) and in the 15 patients with AF induced during EPS than the 30 patients without AF (p <0.0001) ( Table 2 ). The LAD was also greater (p = 0.001) in patients with AF than those without AF ( Table 2 ). The anterograde ERP through AP was faster in patients with AF than those without AF, but the retrograde ERP was similar between them. In a univariate analysis, the AF was associated with a lower H/M ratio, larger LAD, and older age ( Table 3 ). In a multivariate analysis, after adjusting for potential confounding variables, the H/M ratio was a powerful independent predictor of AF, with an odds ratio of 1.37 (95% confidence interval 1.11 to 1.68, p = 0.003) for each 0.1 decrease. The sensitivity of severe sympathetic dysfunction, which was defined with an H/M ratio ≤2.8, for predicting the AF induced during EPS was 75% in 12 of 16 patients. The specificity was 89.7% in 26 of 29 patients ( Figure 2 ). The sensitivity of a large LAD, defined as >37 mm, was 73.3% in 11 of 15 patients, and the specificity was 80% in 24 of 30 patients.
| Variable | WPW Group (n = 45) | Control Group (n = 15) | p |
|---|---|---|---|
| Age (yrs) | 56 ± 17 | 47 ± 17 | 0.08 |
| Women | 19 (42.2) | 6 (40) | 0.88 |
| Heart/mediastinum ratio | 2.99 ± 0.67 | 3.8 ± 0.28 | <0.0001 |
| Left ventricular ejection fraction | 64.1 (8.5) | 66.8 (6.4) | 0.27 |
| LAD (mm) | 35.4 ± 6.1 | 33.8 ± 5.8 | 0.48 |
| Cardiothoracic ratio | 46 ± 4.8 | 46.6 ± 4.5 | 0.68 |
| Variable | Induced AF | p | |
|---|---|---|---|
| Yes (n = 15) | No (n = 30) | ||
| Age (yrs) | 55 ± 16 | 44 ± 16 | 0.03 |
| Women | 8 (53.3) | 11 (36.7) | 0.29 |
| Syncope | 1 (6.7) | 1 (3.3) | 0.61 |
| Diabetes mellitus | 3 (20) | 2 (6.7) | 0.18 |
| Hypertension | 3 (20) | 2 (18.7) | 0.75 |
| Hyperlipidemia | 6 (21.4) | 10 (6.7) | 0.18 |
| Body mass index ≥30 kg/m 2 | 0 | 1 (3.3) | 0.48 |
| Heart/mediastinum ratio | 2.36 ± 0.63 | 3.3 ± 0.43 | <0.0001 |
| Left ventricular ejection fraction (%) | 63.7 ± 9.1 | 64.3 ± 8.4 | 0.83 |
| LAD (mm) | 39.5 ± 4.6 | 33.3 ± 5.7 | 0.001 |
| Cardiothoracic ratio (%) | 47.8 ± 4.6 | 45.1 ± 4.7 | 0.07 |
| Heart rate at rest (beats/min) | 68 ± 9 | 70 ± 11 | 0.53 |
| Systolic blood pressure at rest (mm Hg) | 128 ± 13 | 125 ± 14 | 0.49 |
| Diastolic blood pressure at rest (mm Hg) | 75 ± 8 | 76 ± 11 | 0.72 |
| Heart rate during SVT | 212 ± 42 | 191 ± 37 | 0.09 |
| Serum concentration of C-reactive protein (mg/dl) | 0.1 ± 0 | 0.2 ± 0.2 | 0.1 |
| Plasma brain natriuretic peptide level (pg/ml) | 73.5 ± 153.9 | 26.8 ± 45.3 | 0.27 |
| Use of angiotensin-converting enzyme inhibitor | 3 (20) | 1 (3.3) | 0.06 |
| Use of β blocker | 3 (20) | 1 (3.3) | 0.06 |
| Use of calcium channel antagonist | 3 (20) | 2 (6.7) | 0.18 |
| Use of sodium channel blocker | 0 (0) | 1 (3.3) | 0.48 |
| Anterograde ERP (ms) | 225 ± 36 | 268 ± 50 | 0.005 |
| Retrograde ERP (ms) | 242 ± 42 | 266 ± 69 | 0.22 |
| Variable | Regression Analysis | Univariate Analysis | ||
|---|---|---|---|---|
| Coefficient (β) | Odds Ratio (95% Confidence Interval) | Wald Chi-Square | p | |
| Heart/mediastinum ratio (for 0.1 decrease) | −3.482 | 1.42 (1.15–1.74) | 10.6 | 0.001 |
| LAD, mm (for increase) | +0.213 | 1.24 (1.07–1.43) | 8.57 | 0.003 |
| Age, yrs (for increase) | +0.049 | 1.05 (1.002–1.101) | 4.24 | 0.04 |
| Cardiothoracic ratio, % (for increase) | +0.133 | 1.14 (0.99–1.32) | 3.22 | 0.07 |
| Use of angiotensin-converting enzyme inhibitor | +1.98 | 7.24 (0.68–76.9) | 2.7 | 0.1 |
| Use of β blocker | +1.98 | 3.13 (0.68–76.9) | 2.7 | 0.1 |
| Plasma brain natriuretic peptide level, pg/ml (for increase) | +0.005 | 1.005 (1–1.01) | 1.7 | 0.19 |
| Diabetes mellitus | +1.253 | 3.5 (0.52–23.8) | 1.65 | 0.2 |
| Hypertension | +1.253 | 3.5 (0.52–23.8) | 1.65 | 0.2 |
| Body mass index, kg/m 2 (for increase) | +0.076 | 1.08 (0.9–1.28) | 0.79 | 0.37 |
| Left ventricular ejection fraction, % (for decrease) | −0.009 | 0.99 (0.92–1.07) | 0.51 | 0.82 |




