After repair of tetralogy of Fallot, the left ventricular ejection fraction and the right ventricular ejection fraction are associated with clinical status and outcomes, but the relation of strain, a potentially earlier marker of dysfunction, to quality of life has not been evaluated. In 58 patients with tetralogy of Fallot (median age 29 years, interquartile range 20 to 41) who underwent cardiovascular magnetic resonance imaging and completed the Short Form 36, Version 2 (a validated quality-of-life assessment), left ventricular global circumferential strain, left ventricular global longitudinal strain, and right ventricular free wall longitudinal strain (RVLS FW ) were measured from cine images using feature-tracking software. Age-adjusted z score ≤−1 for the physical component summary or subscales of physical functioning, role-physical, and general health was considered a clinically significant decrease in quality of life. Patients with RVLS FW less than the median had increased odds of decreased physical functioning (odds ratio [OR] 5.4, p = 0.01) and general health (OR 3.5, p = 0.04) subscale scores, which remained significant in patients with right ventricular ejection fractions ≥45% (physical functioning: OR 9.5, p = 0.03; general health: OR 5.9, p = 0.04). Left ventricular global circumferential strain and left ventricular global longitudinal strain did not predict decreased quality of life in this population. Intraobserver and interobserver variability was acceptable for left ventricular global circumferential strain (coefficients of variation 9.5% and 10.0%, respectively) but lower for left ventricular global longitudinal strain (coefficients of variation 17.2% and 16.8%, respectively) and poor for RVLS FW (coefficients of variation 19.9% and 28.8%, respectively). In conclusion, RVLS FW appears to have discriminative ability in this population for decreased quality of life and may yield incremental prognostic value beyond global right ventricular ejection fraction assessment, but further study is needed to evaluate methods to limit variability.
After repair of tetralogy of Fallot (TOF), the left ventricular ejection fraction (LVEF) and the right ventricular ejection fraction (RVEF) are important indicators of clinical outcomes, such as death, sustained ventricular tachycardia, or progression to New York Heart Association class III or IV, and are associated with patient-reported quality of life. However, earlier indicators of ventricular dysfunction could have an important role in clinical decision making, because the LVEF and the RVEF may not improve after pulmonary valve replacement. In several disease states, decreased left ventricular strain has been reported in patients with normal ejection fractions. Left and right ventricular strain measurements have been related to exercise function and outcomes such as ventricular tachycardia and death, but the potential relation to quality of life has not been explored. Feature tracking is a promising technique that can measure strain from standard cardiovascular magnetic resonance (CMR) steady-state free precession cine images and has been validated in comparison with harmonic-phase imaging and speckle-tracking echocardiography. The aim of this study was to evaluate the relations of left and right ventricular strain by feature tracking with patient-reported quality of life in adolescents and adults with repaired TOF.
Methods
This study included patients with repaired TOF, aged ≥14 years, who were referred for clinically indicated CMR imaging from June 2008 to December 2009 and were prospectively enrolled as part of a previous cross-sectional study. Patients were excluded if they had additional significant cardiac malformations (e.g., atrioventricular septal defects) or contraindications to CMR imaging or gadolinium contrast, required anesthesia or if they could not complete the quality-of-life assessment because of cognitive impairment. For this analysis, patients were excluded if the quality-of-life assessment was completed >3 months from the time of CMR imaging or if short-axis or 4-chamber images were not available for analysis. This study was approved by the institutional review board, and all subjects and parents of minors provided informed consent.
CMR imaging was performed using a commercially available 1.5-T scanner (Philips Intera Achieva; Philips Medical Systems, Best, The Netherlands). Cine images were obtained with a breath-hold, electrocardiographically gated, segmented k-space, steady-state free precession sequence, with 30 phases/cardiac cycle.
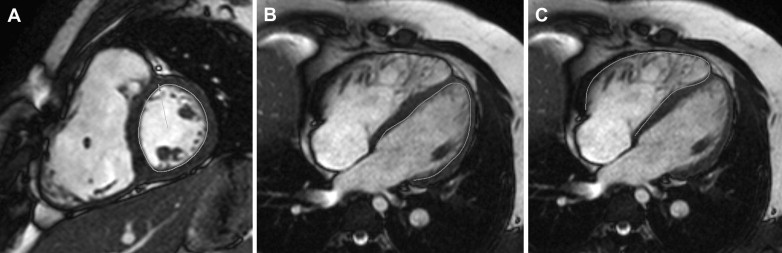
CMR images were analyzed using feature-tracking software (TomTec GmbH, Unterschleissheim, Germany). Points were manually selected along the endocardial contour, with subsequent automated tracking. Contours were visually evaluated for adequate tracking of the endocardium and redrawn as necessary. Left ventricular global circumferential strain (LVGCS) was measured from a midventricular short-axis slice ( Figure 1 ). Left ventricular global longitudinal strain (LVGLS) was measured from a 4-chamber slice ( Figure 1 ). Right ventricular free wall longitudinal strain (RVLS FW ) was measured from a 4-chamber slice, using the 3 segments of the free wall ( Figure 1 ). RVLS FW was chosen a priori over global longitudinal strain because septal motion is incorporated in LVGLS measurement and may vary in this population with factors such as right ventricular conduction delay and relative ventricular pressures. We hypothesized that RVLS FW would better reflect the status of the right ventricle than a 6-segment model. Left ventricular synchrony was evaluated using maximum delay to peak circumferential strain, maximum opposing wall delay to peak longitudinal strain, and the standard deviation of time to peak strain.
A single reader (J.C.L.) analyzed all images and reanalyzed a subset of the first 30 enrolled patients ≥1 month later for intraobserver variability. A second reader (A.L.D.), blinded to the results of the previous analysis, analyzed the subset of 30 patients for interobserver variability.
On enrollment, typically on the day of CMR imaging (maximum 64 days from CMR), subjects completed the Short Form 36, Version 2, which provides a measure of multiple domains of health and functioning. The physical component summary score and the subscales of physical functioning (ability to perform physical activities), role-physical (participation in work or usual activities without physical limitations), and general health (perception of general health and its likelihood to change) were chosen to represent the physical impact of disease. Scores were normalized for age on the basis of population-based normative data. Because previous reports demonstrated only small differences between patients with TOF and controls, an age-adjusted z score ≤−1 was considered a clinically significant decrease in quality of life.
Data are presented as mean ± SD if normally distributed or as median (interquartile range). Categorical variables were compared using chi-square or Fisher’s exact tests, when the expected value of any category was <5. Correlation analysis of continuous variables was performed using Pearson’s correlation coefficient. Odds ratios were calculated for a clinically significant decrease in quality of life, with 95% confidence intervals calculated using Fisher’s exact test. A p value <0.05 was considered statistically significant. Coefficients of variation and Bland-Altman analysis are presented to evaluate interobserver and intraobserver variability.
Results
In the initial cohort, 62 of 65 consecutive patients met the inclusion criteria and were enrolled (1 declined participation, and an investigator was not available for consent for 2 others). Of these patients, 3 did not complete the Short Form 36 within 3 months of CMR imaging. In 1 patient, CMR imaging was performed with pulse gating rather than vector cardiographic gating; despite the selection of a time interval beginning with end-diastole, reliable strain measurements could not be obtained, and the patient was excluded. Feature tracking for the remaining 58 patients was acceptable, and characteristics of this cohort are listed in Table 1 . In this cohort, 13 patients had undergone previous pulmonary valve replacement or conduit replacement a median of 8 years (interquartile range 4 to 11) before CMR imaging. Quality-of-life scores in this population were previously reported, similar to the population norm, except for a small but statistically significant decrease in general health.
| Variable | Value |
|---|---|
| Men | 33 (57%) |
| Age (yrs) | 29 (20 to 41) |
| Age at repair (yrs) | 3.4 (0.8 to 5.7) |
| Time from CMR imaging to Short Form 36 (days) | 0 (0 to 0) |
| Heart rate (beats/min) | 72 ± 12 |
| Type of repair | |
| Transannular patch | 31 (53%) |
| Right ventricle–to–pulmonary artery conduit | 6 (10%) |
| Valve sparing | 7 (12%) |
| Unspecified | 14 (24%) |
| Right ventricular end-diastolic volume (ml/m 2 ) | 145 ± 49 |
| Pulmonary regurgitant fraction (%) | 31 ± 21 |
| LVEF (%) | 54 ± 8 |
| RVEF (%) | 47 ± 8 |
| LVGCS (%) | −21.0 (−17.7 to −22.3) |
| Maximum time delay to peak circumferential strain (ms) | 127 (102 to 164) |
| LVGLS (%) | −14.7 (−11.2 to −17.2) |
| Maximum opposing wall delay (ms) | 163 (94 to 288) |
| RVLS FW (%) | −18.3 (−12.6 to −21.8) |
Left ventricular strain measurements were related to the global LVEF, as well as right ventricular size and function. LVGCS was correlated with the LVEF (r = −0.63, p <0.0001) and the RVEF (r = −0.41, p = 0.002) and decreased in magnitude with increasing right ventricular end-diastolic volume (r = 0.32, p = 0.02). LVGLS was correlated with the LVEF (r = −0.49, p = 0.0001) and weakly with the RVEF (r = −0.33, p = 0.01) but did not reach significance with right ventricular end-diastolic volume (r = 0.22, p = 0.11). RVLS FW was correlated weakly with the LVEF (r = −0.29, p = 0.03) but did not reach significance with the RVEF or right ventricular end-diastolic volume. Right ventricular global longitudinal strain (using 6 segments) was correlated weakly with the RVEF (r = −0.34, p = 0.01).
LVGCS weakly correlated with the physical functioning (r = −0.26, p = 0.05) and role-physical (r = −0.32, p = 0.01) Short Form 36 subscale scores. However, LVGCS less than the median did not reach significance with age-adjusted z scores ≤−1 ( Figure 2 ). LVGLS was not correlated with quality-of-life scores, and LVGLS less than the median was not associated with clinically significant decreases in quality of life ( Figure 2 ). None of the left ventricular synchrony measures was related to quality of life.
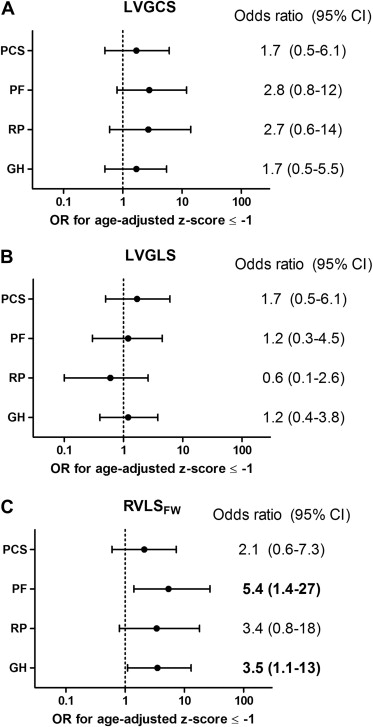
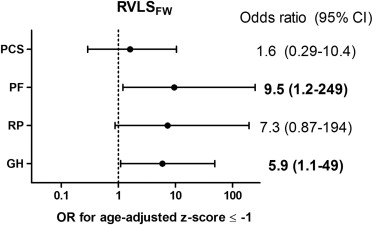
RVLS FW was not correlated with quality-of-life scores, but RVLS FW less than the median was associated with clinically significant decreases in quality of life ( Figure 2 ), which remained significant in 34 patients with normal global right ventricular function ( Figure 3 ). Global right ventricular longitudinal strain (using a 6-segment model) did not reach significance with quality of life, with a strong trend toward decreased physical functioning (odds ratio 3.4, 95% confidence interval 0.93 to 14.3, p = 0.06).
Intraobserver and interobserver variability are listed in Table 2 , with Bland-Altman plots presented in Figure 4 .



