The aim of this study was to investigate whether preoperative determination of plasma copeptin levels in addition to plasma N-terminal pro–B-type natriuretic peptide (NT–pro-BNP) could help improve risk stratification in patients who undergo major vascular surgery. One hundred ninety-eight consecutive patients who underwent major vascular surgery (58.6% infrainguinal aortic reconstruction, 23.7% abdominal aortic aneurysm surgery, 17.7% carotid endarterectomy) were included in this study. Patients were monitored for in-hospital and long-term (2-years) major adverse cardiac events, consisting of cardiac death, nonfatal myocardial infarction, and emergent coronary revascularization. Overall, 40 patients (20.2%) reached the primary end point, and most of these events occurred during the index hospital stay (n = 18 [45%]). In univariate Cox regression analysis, increasing concentrations of copeptin were significant determinants of outcome as a continuous variable (hazard ratio [HR] 1.012, p = 0.005) and as a dichotomized variable according to the recommended cutoff of 14.0 pmol/L (HR 4.116, p <0.001). Subgroup analyses revealed that especially patients at low estimated risk according to plasma NT–pro-BNP levels were at significantly higher risk for worse outcomes with higher copeptin levels (HR 5.983, p = 0.002). In multivariate Cox regression analysis, copeptin concentrations >14 pmol/L were significant independent predictors of outcome (HR 2.842, p = 0.002) in addition to type of surgery, history of myocardial infarction, elevated levels of cardiac troponin T, and NT–pro-BNP levels. In conclusion, the results of this study suggest that preoperative determination of this new biomarker could substantially improve prediction of perioperative and postoperative outcomes in vascular surgery patients.
Patients who undergo elective noncardiac surgery have a high prevalence of asymptomatic coronary artery disease, and because of the aging population, the incidence of significant coronary artery disease will further increase during the next decades. Cardiac complications are frequent after noncardiac surgery, and vascular surgery patients in particular have a high rate of perioperative myocardial damage and associated cardiac mortality. Several risk indexes have been developed to estimate a patient’s risk for postoperative complications. The revised cardiac risk index (Lee index) is the preferred tool of clinicians for the preoperative evaluation of surgery patients because it uses easily obtainable variables of medical history data and has been validated on a large database of noncardiac surgery patients. Arginine vasopressin (AVP) or antidiuretic hormone plays a central role in the regulation of osmotic and cardiovascular homeostasis. In addition to increasing blood pressure by enhancement of free water reabsorption by the kidney and inducing peripheral vasoconstriction, AVP also stimulates platelet aggregation and release of von Willebrand factor and factor VIII. Because perioperative myocardial infarction is at least partially induced by tachycardia, hypertension, platelet aggregation, reduced fibrinolytic activity, and consecutive hypercoagulability, it is plausible that activation of the hypothalamus-pituitary axis and enhanced AVP secretion before surgery makes patients susceptible for perioperative myocardial injury. Therefore, quantification of AVP secretion would be of major clinical importance for preoperative risk evaluation and extension of perioperative surveillance and therapy. However, AVP is unstable in human plasma, is largely attached to platelets, and has a short half-life, which makes this nonapeptide unsuitable as a biomarker for the daily clinical routine. In contrast, copeptin, the C-terminal fragment of the provasopressin peptide, is secreted in equimolar doses with AVP and can reliably determined using a novel chemiluminescence assay. Thereby, determination of copeptin concentrations provides a unique opportunity to investigate the activity of the hypothalamic-pituitary-adrenal axis and quantify the individual stress level. Previously, we showed in a prospective study of patients who underwent major vascular surgery that preoperative and postoperative measurement of N-terminal pro–B-type natriuretic peptide (NT–pro-BNP) could be used for the prediction of short- and long-term cardiac events, including fatal or nonfatal myocardial infarction. Using this clinically well defined cohort, we investigated whether measurement of copeptin on the day before elective vascular surgery could be used for the identification of high-risk patients in addition to NT–pro-BNP and cardiac troponin T (cTnT) levels.
Methods
The study protocol with the inclusion and exclusion criteria of this prospective observational study has already been published. In brief, 287 consecutive patients scheduled for vascular surgery (abdominal aortic aneurysm surgery, infrainguinal arterial reconstruction, or carotid endarterectomy) were screened for eligibility from October 2002 to June 2003. Excluded were patients with acute coronary syndromes or evidence of myocardial ischemia on stress tests (n = 4), decompensated heart failure (n = 2), aortic stenosis (n = 2), atrial fibrillation (n = 17), kidney dysfunction (serum creatinine ≥1.4 mg/dl; n = 26), reduced left ventricular function (left ventricular ejection fraction <40%; n = 10), and canceled surgery (n = 6) and those who were unable or refused to provide written informed consent (n = 2). Of the remaining 218 patients with complete follow-up, 198 patients had available plasma samples for determination of copeptin levels. The institutional review board of the Medical University of Graz (Graz, Austria) approved the study.
Blood samples were centrifuged and stored in aliquots at −80°C until determination of the respective biomarkers. Copeptin concentrations were measured using a novel commercially available chemiluminescence assay (Brahms AG, Hennigsdorf, Germany), as described previously. The assay has an analytic detection limit of 0.4 pmol/L and a functional assay sensitivity (lowest value with an interassay coefficient of variation <20%) <1.0 pmol/L and allows the precise measurement of copeptin in a range of 0.4 to 1,250 pmol/L. Plasma concentrations of NT–pro-BNP were determined using an Elecsys 2010 instrument (Roche Diagnostics GmbH, Mannheim, Germany; sensitivity 5 pg/ml, intra- and interassay coefficients of variance <3%). High-sensitivity C-reactive protein (hs-CRP) was measured by a particle-enhanced immunonephelometric assay (CardioPhase hs-CRP; Dade Behring GmbH, Marburg, Germany; sensitivity 0.175 mg/L, intra- and interassay coefficients of variance <5%). Cardiac troponin T was measured using an electrochemiluminescence immunoassay (Elecsys troponin T STAT; Roche Diagnostics GmbH; 99th percentile of the distribution in healthy population <0.01 ng/ml, sensitivity 0.01 ng/ml, intra- and interassay coefficients of variance <5%, cutoff 0.03 ng/ml).
The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) study equation. The revised cardiac risk index or Lee index was calculated for each patient as described previously. Because patients with creatinine concentrations >1.4 mg/dl were excluded, this variable could not be used in our data set. Abdominal aortic aneurysm and infrainguinal arterial reconstruction were considered high-risk surgery. The Eagle score was calculated according to the original publication in 1996. Anesthetic management, perioperative care, and intensive care unit referral were at the discretion of the attending physician. Perioperative anticoagulation was standardized. Intraoperatively, all patients received unfractionated heparin (30 U/kg intravenously) before vascular clamping but no protamine after vascular declamping.
In patients who underwent carotid endarterectomy or infrainguinal bypass surgery, long-term therapy with aspirin or clopidogrel was maintained perioperatively. In patients who underwent elective abdominal aortic aneurysm surgery, long-term antiplatelet (aspirin and clopidogrel) therapy was discontinued 5 to 7 days preoperatively, replaced with low–molecular weight heparin until surgery, and resumed on postoperative day 3 in case of uneventful clinical course.
In-hospital and long-term follow-up (24 to 30 months after index surgery) were performed for all patients. The primary end point of the study was a composite of cardiac death, nonfatal myocardial infarction, and emergent coronary artery revascularization, whichever occurred first. All end points were adjudicated by an independent cardiologist who had access to all available documents and clinical charts of each patient. Cardiac death was defined by death secondary to myocardial infarction, cardiac arrhythmia, or heart failure. Nonfatal myocardial infarction was defined by clinical, electrocardiographic, and/or echocardiographic signs and symptoms suggestive of myocardial ischemia, with typical increase of cTnT to >0.03 ng/ml. Emergent coronary revascularization was defined as percutaneous coronary angioplasty or coronary artery bypass grafting due to sustained myocardial ischemia and hemodynamic compromise despite optimal medical therapy.
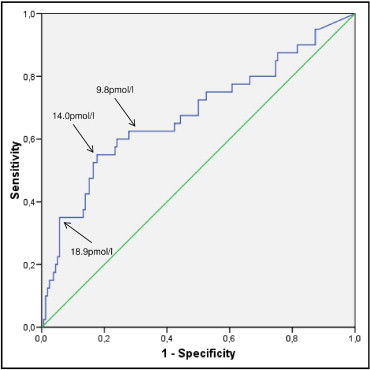
Continuous variables are expressed as mean ± SD unless stated otherwise. Relations between continuous variables were determined using Spearman’s rank correlation test and linear regression analyses. Categorical variables and event rates were compared using Pearson’s chi-square test, and Student’s t test or the Mann-Whitney U test, as appropriate, was used to compare continuous variables. We defined elevated copeptin levels above the cutoff of 14 pmol/L, as previously suggested. In the present data set, this cutoff had sensitivity of 55.0% and specificity of 82.3% to predict cardiac events. The NT–pro-BNP cutoff of 280 pg/ml had similar accuracy to predict postoperative outcome (sensitivity 70.00%, specificity 70.90%) as previously reported. Similarly, the creatinine cutoff of 1.2 mg/dl and the hs-CRP protein cutoff of >3 mg/dl also had similar predictive power, as previously published. Therefore, we used these cutoffs in subgroup analysis.
Differences in survival rates were tested using Kaplan-Meier survival curve analysis and log-rank tests. Univariate Cox regression analysis was performed to identify significant predictors of outcomes. Predictors significant at the 0.20 level were included in the multivariate analysis with a forward selection method. The following variables were tested in univariate analyses: age, gender, history of diabetes mellitus, hypertension, myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, congestive heart failure, cerebrovascular disease, and clinical scores (Lee and Eagle criteria) as well as laboratory measures obtained before surgery (hs-CRP, cTnT, creatinine, eGFR, and NT–pro-BNP concentrations). In a separate multivariable analysis, we included copeptin, NT–pro-BNP, cTnT, creatinine, and hs-CRP as dichotomized variables according to the cutoffs described previously. In separate multivariable models, we also tested whether preoperative copeptin concentrations are predictive of outcome independent of the Lee index and the Eagle score. The proportional-hazards assumption was confirmed by the Schoenfeld residual test. To estimate the predictive value of copeptin concentrations in addition to clinical variables, we calculated and compared C-statistics of the 2 models (model 1: clinical characteristics and laboratory parameters; model 2: model 1 plus copeptin concentrations) and also calculated net reclassification improvement (NRI). Clinical variables used for estimation of 2-year outcomes by multivariate logistic regression analysis (model 1) were age, gender, type of surgery, history of diabetes mellitus, hypertension, myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, congestive heart failure, cerebrovascular disease, and laboratory measures (hs-CRP, cTnT, creatinine, and NT–pro-BNP).
All statistical tests were 2 tailed, and statistical significance was accepted for p values <0.05. SPSS version 15 (SPSS, Inc., Chicago, Illinois) was used for all statistical calculations except for comparing the areas under receiver-operating characteristic curves (Stata version 10.1 SE; StataCorp LP, College Station, Texas).
Results
The baseline characteristics of patients according to copeptin levels are listed in Table 1 . Median copeptin concentrations were 7.0 pmol/L (interquartile range 3.1 to 14.2) and in 49 patients (24.7%) exceeded the recommended cutoff of >14.0 pmol/L and in 38 patients (19.2%) exceeded 17.4 pmol/L (97.5th percentile of healthy subjects). Patients with higher copeptin concentrations were significantly older and had significantly higher plasma NT–pro-BNP, cTnT, hs-CRP, and creatinine concentrations as well as significantly lower eGFRs compared to patients with copeptin levels within the normal range. Especially concentrations of NT–pro-BNP after surgery (determined between the third and fifth postoperative day) were substantially higher in patients with higher copeptin levels before surgery.
| Variable | All Patients | Copeptin ≤14 pmol/L | Copeptin >14 pmol/L | p Value |
|---|---|---|---|---|
| (n = 198) | (n = 149) | (n = 49) | ||
| Age (years) | 69 ± 9 | 69 ± 9 | 75 ± 8 | <0.001 |
| Women | 44 (22.2%) | 34 (22.8%) | 10 (20.4%) | 0.725 |
| Abdominal aortic aneurysm | 47 (23.7%) | 34 (22.8%) | 13 (26.5%) | 0.284 |
| Infrainguinal arterial reconstruction | 116 (58.6%) | 85 (57.0%) | 31 (63.3%) | |
| Carotid endarterectomy | 35 (17.7%) | 30 (20.1%) | 5 (10.2%) | |
| Diabetes mellitus | 69 (34.8%) | 47 (31.5%) | 22 (44.9%) | 0.089 |
| Hypertension | 147 (74.2%) | 111 (74.5%) | 36 (73.5%) | 0.887 |
| Smoking | 59 (29.8%) | 44 (29.5%) | 15 (30.6%) | 0.786 |
| Previous percutaneous coronary intervention | 8 (4.0%) | 5 (3.4%) | 3 (6.1%) | 0.760 |
| Previous coronary artery bypass grafting | 15 (7.6%) | 11 (7.4%) | 4 (8.2%) | 0.858 |
| Previous myocardial infarction | 51 (25.8%) | 34 (22.8%) | 17 (34.7%) | 0.099 |
| Previous congestive heart failure | 10 (5.1%) | 7 (4.7%) | 3 (6.1%) | 0.693 |
| Stroke or transient ischemic attack | 35 (17.7%) | 30 (20.1%) | 5 (10.2%) | 0.114 |
| Preoperative troponin T ≤0.01 ng/ml | 181 (91.4%) | 141 (94.6%) | 40 (81.6%) | 0.017 |
| Troponin T 0.02–0.03 ng/ml | 12 (6.1%) | 6 (4.0%) | 6 (12.2%) | |
| Troponin T >0.03 ng/ml | 5 (2.5%) | 2 (1.3%) | 3 (6.1%) | |
| hs-CRP (mg/dl) | 5.5 (1.9–13.8) | 3.6 (1.7–12.2) | 8.1 (3.8–20.0) | 0.007 |
| Creatinine (mg/dl) | 1.1 (1.0–1.2) | 1.1 (0.9–1.2) | 1.2 (1.0–1.4) | 0.002 |
| eGFR (ml/min/1.73 m 2 ) | 68 (57–77) | 65 (53–80) | 52 (43–71) | 0.005 |
| Preoperative NT–pro-BNP (pg/ml) | 204 (79–457) | 168 (75–397) | 367 (137–937) | <0.001 |
| NT–pro-BNP, postoperative day 3 to 5 (pg/ml) | 549 (206–1,162) | 393 (167–999) | 1,129 (541–3,112) | <0.001 |
| Angiotensin converting enzyme inhibitors | 103 (52.0%) | 74 (49.7%) | 29 (59.2%) | 0.247 |
| β blockers | 150 (75.8%) | 117 (78.5%) | 33 (67.3%) | 0.113 |
| Diuretics | 7 (3.5%) | 5 (3.4%) | 2 (4.1%) | 0.811 |
| Statins | 74 (37.4%) | 59 (39.6%) | 15 (30.6%) | 0.259 |
| Aspirin | 169 (85.4%) | 128 (85.9%) | 41 (83.7%) | 0.701 |
| Duration of surgery (hours) | 140 (108–205) | 130 (90–180) | 180 (120–215) | 0.027 |
| Surgical complications | 16 (8.1%) | 11 (7.4%) | 5 (10.2%) | 0.530 |
| Reoperation | 8 (4.0%) | 6 (4.0%) | 2 (4.1%) | 0.987 |
| Hospital stay (days) | 12 (9–16) | 12 (9–15) | 13 (10–18) | 0.269 |
| In-hospital event | 18 (9.1%) | 8 (5.4%) | 10 (20.4%) | 0.001 |
| Primary end point | 40 (20.2%) | 19 (12.8%) | 21 (42.9%) | <0.001 |
With respect to surgical parameters, we found that patients with high copeptin concentrations had significantly longer durations of surgery, but length of hospital stay did not differ significantly. Preoperative medications were not significantly different with respect to copeptin levels. In-hospital events and adverse events occurring during long-term follow-up after index surgery were substantially higher in patients with higher preoperative copeptin levels.
Median concentrations of copeptin were not significantly different in patients with different Lee index (Lee index 1 [n = 127]: 6.9 [4.0 to 12.9]; Lee index ≥2 [n = 71]: 7.8 [2.4 to 15.7]; p = 0.913) but were significantly higher in patients with higher Eagle scores (Eagle score 0: 5.8 [2.4 to 9.5]; Eagle score 1 to 3: 7.3 [3.4 to 15.6]; Eagles core ≥4: 17.1 [3.4 to 29.7]; p = 0.026).
Copeptin concentrations showed weak but significant positive correlations with age (r = 0.248, p <0.001), NT–pro-BNP (r = 0.256, p <0.001), hs-CRP (r = 0.263, p <0.001), cTnT (r = 0.228, p = 0.001), and creatinine levels (r = 0.226, p = 0.001) and negative correlation with eGFR (r = −0.177, p = 0.013).
In multivariate linear regression analysis, only age, hs-CRP, and creatinine concentrations were independent determinants of copeptin levels, but these 3 variables accounted only for 18.1% of variation of copeptin.
Overall, 40 patients (20.2%) reached the primary end point (cardiac death n = 15, nonfatal myocardial infarction n = 22, acute coronary revascularization n = 3), and 45% of these events (n = 18) occurred during the index hospital stay. Plasma copeptin concentrations were significantly higher in patients who developed cardiac events compared to those who remained event free (primary end point 15.5 pmol/L [5.4 to 30.5] vs no event 6.5 pmol/L [2.7 to 10.6], p <0.001). On receiver-operating characteristic analysis, copeptin levels were significant predictors of the primary end point, with an area under the curve of 0.679 (95% confidence interval [CI] 0.576 to 0.782, p <0.001, Figure 1 ), which was lower than that for NT–pro-BNP (0.750, 95% CI 0.658 to 0.842, p <0.001) (p = 0.23 vs copeptin) but higher than that for cTnT (0.605, 95% CI 0.534 to 0.676, p = 0.039) (p = 0.170 vs copeptin) and hs-CRP (0.604, 95% CI 0.512 to 0.697, p = 0.041) (p = 0.199 vs copeptin).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


