Among patients with coronary artery disease, pet owners exhibit a greater 1-year survival rate than nonowners. Lifestyle-related diseases are well-known risk factors for coronary artery disease and induce imbalances in autonomic nervous activity. The purpose of the present study was to determine whether pet ownership modulates cardiac autonomic nervous activity imbalance in patients with lifestyle-related diseases such as diabetes mellitus, hypertension, and hyperlipidemia. A total of 191 patients (mean age 69 ± 8 years) were interviewed about their pet ownership status and were classified into pet owner and nonowner groups. After recording a 24-hour Holter electrocardiogram for heart rate variability analysis, frequency-domain and nonlinear-domain analyses were performed to determine the high-frequency (HF) and low-frequency (LF) components, LF/HF ratio, and entropy. The heart rate variability parameters were assessed for 24 hours, during the day (8.00 a.m. to 5.00 p.m. ), and during the night (0:00 a.m. to 6.00 a.m. ), and compared between the 2 groups. To evaluate the potential predictive factors for cardiac autonomic imbalance, univariate and multivariate analyses of HF and LF/HF were conducted for potential confounding variables. The pet owner group exhibited significantly greater HF 24h , HF day , HF night , entropy 24h , entropy day , and entropy night and significantly lower LF/HF 24h and LF/HF night compared to the nonowner group. On multivariate analysis, pet ownership was independently and positively associated with HF 24h, HF day , and HF night and inversely associated with LF/HF 24h and LF/HF night . In conclusion, these results suggest that pet ownership is an independent modulator of cardiac autonomic imbalance in patients with lifestyle-related diseases.
Lifestyle-related diseases, such as diabetes mellitus, hypertension, and hyperlipidemia, are well-known risk factors for coronary artery diseases. Moreover, patients with lifestyle-related diseases exhibit autonomic nervous activity imbalance. The effect of pet ownership on cardiac autonomic nervous activity has not been evaluated in patients with lifestyle-related diseases. Accordingly, the aim of the present study was to determine whether pet ownership modulates cardiac autonomic nervous activity imbalances in patients with lifestyle-related diseases.
Methods
The Ethics Committee on Human Research of Kitasato University approved the present study. Outpatients who regularly visited the cardiovascular center of Kitasato University Hospital from January 2009 to December 2010 because of diabetes mellitus, hypertension, and hyperlipidemia were eligible to participate. Patients with other major illnesses, such as old myocardial infarction, angina pectoris, chronic renal failure, and frequent arrhythmias, were excluded. A total of 244 patients who satisfied the initial criteria were informed about the study, and all patients provided written informed consent.
The patients were classified into 2 groups according to pet ownership: pet owner and nonowner groups. A pet owner was defined as a patient who currently had a pet and had had the pet for >6 months at study enrollment. Those patients who had had pets in the past, but not currently, were excluded from the present study. In the pet owner group, the patients were interviewed about their pet ownership status, including the number and species of pets, pet-keeping duration, where the pet is kept (inside or outside the house), the amount of time spent a day by the owners walking their dogs, and whether the patient was the main caretaker of the pet. Pet ownership status is listed in Table 1 .
| Variable | Dog Owners (n = 46) | Cat Owners (n = 27) | Other Owners ⁎ (n = 9) |
|---|---|---|---|
| Pet-keeping duration (years) | 15 ± 11 | 16 ± 12 | 15 ± 8 |
| Keeping area | |||
| Inside | 35 | 25 | 6 |
| Outside | 11 | 2 | 3 |
| Main caretaker | |||
| Yes | 17 | 17 | 4 |
| No | 23 | 3 | 2 |
| Do not know | 6 | 7 | 3 |
| Walking with dog | |||
| Yes | 29 | — | — |
| No | 17 | ||
| Amount of time spent with dog walking per day | |||
| <30 minutes | 6 | — | — |
| ≥30 minutes | 12 | — | — |
| ≥60 minutes | 8 | — | — |
| ≥120 minutes | 3 | — | — |
We assessed the disease-specific cardiovascular functional status using the specific activity scale. The specific activity scale included 21 items of self-reported data on the performance of well-defined daily activities (e.g., walking, climbing stairs, showering, dressing), which was developed as an alternative to the New York Heart Association functional classification.
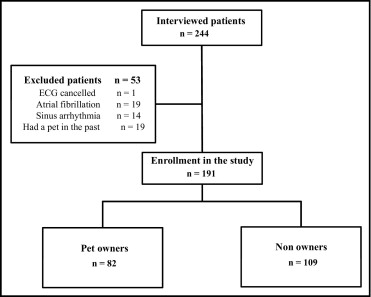
After the interview, the patients underwent physical and blood examinations, 24-hour Holter electrocardiogram, echocardiogram, and a measurement of brachial-ankle pulsewave velocity. After the 24-hour Holter electrocardiogram, the patients who exhibited atrial fibrillation, marked sinus arrhythmia, or frequent atrial or ventricular premature beats were excluded. Thus, 191 patients participated in the present study ( Figure 1 ) .
The clinical and sociodemographic variables, including gender, age, systolic blood pressure, diastolic blood pressure, heart rate, diagnosis, current smoking status, and medications, were obtained from the medical records at the beginning of the study. The routine biochemical parameters, such as the serum concentrations of low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, and hemoglobin A1c, were evaluated. The body mass index was calculated as the body weight in kilograms divided by height in square meters. Echocardiographic analysis was performed by an investigator who was unaware of the clinical and treatment status of patients. Left atrial diameter, left ventricular end-diastolic diameter, left ventricular end-systolic diameter, left ventricular posterior wall thickness, and interventricular septal thickness were measured to calculate the left ventricular ejection fraction and left ventricular muscle mass. The ventricular muscle mass was corrected by body surface area and expressed as the ventricular muscle mass index.
Autonomic nervous activity was evaluated by heart rate variability (HRV) analysis using a 24-hour Holter electrocardiogram (Aria, Del Mar Reynolds Medical, Irvine, California). The HRV based on the beat-to-beat RR intervals of normal sinus beats was assessed for 24 hours, during the day (8.00 a.m. to 5.00 p.m. ) and during the night (0:00 a.m. to 6.00 a.m. ). A Holter recording was considered suitable for time-domain, frequency-domain, or nonlinear-domain HRV analysis if it contained ≥95% analyzable data for each period.
The time-domain indexes included the standard deviation of a series of all-normal RR intervals (SDNN), standard deviation of mean RR intervals of a 5-minute electrocardiogram (SDANN), the square root of the average of squares of differences between consecutive RR intervals (RMSSD), and the percentage of RR intervals that differed from each other by >50 ms. SDNN and SDANN reflect overall HRV. RMSSD and percentage of RR intervals that differed from each other by >50 ms reflect the cardiac parasympathetic nervous activity. The time-domain parameter indexes for the 24-hour, daytime, and nighttime periods are presented as the SDNN 24h , SDNN day , SDNN night , RMSSD 24h , RMSSD day , RMSSD night , SDANN 24h , SDANN day , and SDANN night , respectively.
Using RR intervals obtained from a 24-hour Holter electrocardiogram, a beat-to-beat spectral analysis was performed with a combination of the maximum entropy method for spectral analysis and the nonlinear least squares method for fitting analysis (MemCalc, GMS, Tokyo, Japan) to obtain the HR and 2 frequency bands: a low frequency (LF) component of 0.04 to 0.15 Hz and a high frequency (HF) component of 0.15 to 0.4 Hz. The HF and LF/HF ratio indicate parasympathetic nervous activity and the dominance of sympathetic nervous activity over parasympathetic activity, respectively. The HR and frequency-domain parameters for the different periods are presented as HR 24h , HR day , HR night , HF 24h , HF day , HF night , LF/HF 24h , LF/HF day , and LF/HF night , respectively.
A nonlinear-domain analysis of HRV was also performed with MemCalc to assess entropy as a complexity of the cardiovascular system. Entropy was calculated from a pulse time series of 4 RR intervals and expressed as a scale from 0% (indicating no HRV randomness) to 100% (indicating complete HRV randomness). Entropy for the different periods is presented as entropy 24h , entropy day , and entropy night , respectively.
The Mann-Whitney U test, Student’s t test, and chi-square test were used to examine the differences in the clinical characteristics and autonomic nervous activity between pet owner and nonowner groups. The comparisons of the mean values for normally distributed continuous variables were performed using Student’s t test. For continuous variables with non-normal distributions, the Mann-Whitney U test was used. Univariate and multivariate linear regression analyses of the HF and LF/HF measurements were conducted for potential confounding variables: gender, age, HR, body mass index, left ventricular ejection fraction, brachial-ankle pulsewave velocity, diabetes mellitus, hypertension, hyperlipidemia, smoking status, and pet ownership, to evaluate potential predictive factors for autonomic nervous activity in patients with lifestyle-related diseases. p <0.05 was considered statistically significant. All statistical analyses were performed using SPSS, versions 16.0J for Windows (SPSS Japan, Tokyo, Japan).
Results
The patient characteristics are presented in Table 2 . No significant differences were found in the demographic and physiologic characteristics between the pet owner and nonowner groups.
| Characteristic | Total (n = 191) | Pet Owner | P Value | |
|---|---|---|---|---|
| Yes (n = 82) | No (n = 109) | |||
| Men | 143 (75%) | 60 (73%) | 83 (76%) | .38 |
| Age (years) | 69 ± 8 | 68 ± 10 | 70 ± 7 | .51 |
| Systolic blood pressure (mm Hg) | 126 ± 15 | 125 ± 15 | 126 ± 16 | .73 |
| Diastolic blood pressure (mm Hg) | 70 ± 11 | 70 ± 9.7 | 71 ± 11 | .23 |
| Heart rate (beats/min) | 68 ± 8 | 67 ± 8 | 69 ± 9 | .10 |
| Body mass index (kg/m 2 ) | 23.8 ± 3 | 23.9 ± 3 | 23.8 ± 3 | .79 |
| Low-density lipoprotein cholesterol (mg/dL) | 108 ± 26 | 110 ± 25 | 107 ± 27 | .11 |
| High-density lipoprotein cholesterol (mg/dL) | 57 ± 19 | 57 ± 16 | 57 ± 21 | .77 |
| Triglycerides (mg/dL) | .89 | |||
| Median | 112 | 109 | 113 | |
| Interquartile range | 74–162 | 71–163 | 76–161 | |
| Hemoglobin A1c (%) | 5.9 ± 0.9 | 5.9 ± 0.8 | 6.0 ± 1 | .68 |
| Left ventricular ejection fraction (%) | 62 ± 7.7 | 61 ± 8 | 62 ± 8 | .60 |
| Left ventricular muscle mass index | 126 ± 29 | 127 ± 27 | 125 ± 31 | .40 |
| Brachial ankle pulse wave velosity (cm/s) | .49 | |||
| Median | 1,620 | 1,619 | 1,614 | |
| Interquartile range | 1,421–1,763 | 1,393–1,759 | 1,447–1,826 | |
| Diagnosis | ||||
| Diabetes mellitus | 87 (46%) | 38 (46%) | 49 (45%) | .48 |
| Hypertension | 90 (47%) | 41 (50%) | 49 (45%) | .29 |
| Hyperlipidemia | 117 (61%) | 47 (57%) | 70 (64%) | .21 |
| Current smoker | 21 (11%) | 11 (13%) | 10 (9%) | .24 |
| Antidiabetic agents | ||||
| Insulin | 7 (8%) | 2 (5%) | 5 (10%) | .57 |
| Hypoglycemic agents | 29 (33%) | 12 (32%) | 17 (35%) | .43 |
| Diet therapy | 51 (59%) | 24 (63%) | 27 (55%) | .51 |
| Medication use | ||||
| β Blockers | 88 (46%) | 39 (48%) | 49 (45%) | .42 |
| Statins | 105 (55%) | 45 (55%) | 60 (55%) | .55 |
| Specific activity scale (METs) | 6.7 ± 0.9 | 6.6 ± 0.86 | 6.7 ± 1 | .86 |
The HR and time-domain analysis of HRV parameters are presented in Table 3 . HR night was significantly lower in the pet owner group than in the nonowner group (p <0.05). RMSSD 24h , RMSSD day , RMSSD night , and percentage of RR intervals that differed from each other by >50 ms were significantly greater in the pet owner group than in the nonowner group (p <0.01 for each). HF 24h , HF day , and HF night were significantly greater in the pet owner group than in the nonowner group (p <0.01 for each; Figure 2 ) . The LF/HF 24h and LF/HF night were significantly lower in the pet owner group than in the nonowner group (p <0.05 for each; Figure 3 ) ; and entropy 24h , entropy day , and entropy night were significantly greater in the pet owner group than in the nonowner group (p <0.01 for each; Figure 4 ) .
| Variable | Pet Owners | Nonowners | p Value |
|---|---|---|---|
| Heart rate | |||
| 24 hour | 67 ± 8 | 69 ± 9 | 0.10 |
| Day | 70 ± 10 | 73 ± 10 | 0.14 |
| Night | 59 ± 8 | 62 ± 9 | 0.05 ⁎ |
| Mean NN (ms) | 874 (772–957) | 837 (769–937) | 0.14 |
| pNN50 (%) | 5.2 (1.4–9.9) | 2.5 (0.9–5.8) | 0.001 † |
| SDNN 24h (ms) | 131 (109–153) | 119 (102–141) | 0.07 |
| SDNN day (ms) | 106 (84–127) | 102 (84–118) | 0.19 |
| SDNN night (ms) | 84 (71–111) | 82 (69–98) | 0.11 |
| RMSSD 24h (ms) | 28 (21–37) | 24 (18–29) | 0.001 † |
| RMSSD day (ms) | 25 (20–34) | 22 (17–28) | 0.002 † |
| RMSSD night (ms) | 31 (22–38) | 24 (19–31) | 0.003 † |
| SDANN 24h (ms) | 122 (102–142) | 111 (94–133) | 0.06 |
| SDANN day (ms) | 97 (78–118) | 95 (77–110) | 0.18 |
| SDANN night (ms) | 69 (57–91) | 64 (53–81) | 0.11 |
The univariate and multivariate regression analysis results of HF are presented in Table 4 . On multivariate analysis, pet ownership was positively associated with HF 24h , HF day , and HF night (p <0.01 for each), and HR was inversely associated with HF 24h , HF day , and HF night (p <0.01, p <0.05, and p <0.01, respectively). Diabetes mellitus was inversely associated with HF 24h and HF day (p <0.01 for each), and hyperlipidemia was inversely associated with HF 24h , HF day , and HF night (p <0.01 for each).
| High Frequency | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| B | 95% CI | p Value | B | 95% CI | p Value | |
| 24 hours | ||||||
| Gender | 7.4 | −27.1, 41.9 | 0.67 | 8.2 | −24.9, 41.3 | 0.63 |
| Age | −0.79 | −2.6, 1.0 | 0.38 | −0.56 | −2.4, 1.3 | 0.55 |
| Heart rate | −2.9 | −4.6, −1.2 | 0.001 ⁎ | −2.55 | −4.2, −0.9 | 0.003 ⁎ |
| Body mass index | 1.3 | −3.6, 6.3 | 0.60 | 2.2 | −2.5, 6.9 | 0.35 |
| Left ventricular ejection fraction | −0.04 | −2.0, 1.9 | 0.97 | −0.4 | −2.24, 1.5 | 0.70 |
| Brachial ankle pulse wave velosity | −0.04 | −0.09, 0.006 | 0.09 | −0.03 | −0.08, 0.02 | 0.27 |
| Diabetes mellitus | −30.53 | −60.3, −0.8 | 0.044 † | −38.3 | −67, −9.8 | 0.009 ⁎ |
| Hypertension | 12.5 | −17.4, 42.4 | 0.41 | 18.6 | −11.6, 48.8 | 0.24 |
| Hyperlipidemia | −44.2 | −74.3, −14.1 | 0.004 ⁎ | −40.5 | −69.2, −11.9 | 0.006 ⁎ |
| Smoking | 5.2 | −42.6, 53.0 | 0.83 | 7.9 | −37.9, 53.6 | 0.74 |
| Pet ownership | 66 | 37.3, 94.8 | 0.00 ⁎ | 54.0 | 25.8, 82.1 | 0.000 ⁎ |
| Day | ||||||
| Gender | 4.0 | −31.0, 39.1 | 0.82 | 0.9 | −34.0, 35.8 | 0.96 |
| Age | −0.3 | −2.1, 1.5 | 0.73 | −0.24 | −2.2, 1.7 | 0.81 |
| Heart rate | −2.5 | −4.3, −0.8 | 0.005 ⁎ | −1.9 | −3.7, 0.09 | 0.04 † |
| Body mass index | 1.1 | −4.0, 6.2 | 0.66 | 2.2 | −2.8, 7.1 | 0.39 |
| Left ventricular ejection fraction | 0.52 | −1.5, 2.5 | 0.61 | 0.28 | −1.7, 2.2 | 0.78 |
| Brachial ankle pulse wave velosity | −0.03 | −0.08, 0.02 | 0.26 | −0.02 | −0.08, 0.03 | 0.38 |
| Diabetes mellitus | −29 | −59.3, 1.2 | 0.06 | −38.1 | −68, −8.1 | 0.01 ⁎ |
| Hypertension | 17.5 | −12.9, 47.8 | 0.26 | 22.5 | −9.3, 54.3 | 0.16 |
| Hyperlipidemia | −46.2 | −76.6, −15.7 | 0.003 ⁎ | −42.7 | −72.9, −12.6 | 0.006 ⁎ |
| Smoking | 1.2 | −47.4, 49.7 | 1.0 | 3.3 | −44.9, 51.5 | 0.89 |
| Pet ownership | 52.1 | 22.3, 81.9 | 0.001 ⁎ | 42.56 | 12.93, 72.2 | 0.005 ⁎ |
| Night | ||||||
| Gender | 32.1 | −14.5, 78.6 | 0.18 | 35.08 | −10.2, 80.4 | 0.13 |
| Age | −2.1 | −4.5, 0.31 | 0.09 | −1.74 | −4.3, 0.81 | 0.18 |
| Heart rate | −4.1 | −6.4, −1.7 | 0.001 ⁎ | −3.55 | −5.9, −1.2 | 0.003 ⁎ |
| Body mass index | 2.6 | −4.1, 9.4 | 0.45 | 3.05 | −3.3, 9.4 | 0.35 |
| Left ventricular ejection fraction | 0.1 | −2.5, 2.8 | 0.91 | −0.72 | −3.3, 1.8 | 0.58 |
| Brachial ankle pulse wave velosity | −0.06 | −0.13, 0.003 | 0.06 | −0.04 | −0.1, 0.03 | 0.30 |
| Diabetes mellitus | −19.1 | −59.7, 21.6 | 0.36 | −28.5 | −67.5, 10.5 | 0.15 |
| Hypertension | 18.0 | −22.6, 58.5 | 0.38 | 25.64 | −15.7, 67.0 | 0.22 |
| Hyperlipidemia | −57.7 | −98.6, −16.9 | 0.006 ⁎ | −51.57 | −90.8, −12.4 | 0.01 ⁎ |
| Smoking | 18.5 | −46.4, 83.3 | 0.58 | 20.17 | −42.5, 82.8 | 0.53 |
| Pet ownership | 84.6 | 45.5, 123.8 | 0.00 ⁎ | 65.3 | 26.8, 103.8 | 0.001 ⁎ |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


