Atrioventricular (AV) dyssynchrony as well as ventricular-ventricular dyssynchrony plays an important role in the selection of candidates for cardiac resynchronization therapy (CRT), but no method for assessing the AV dyssynchrony has been established. The aim of this study was to investigate whether the degree of overlap of the E and A waves can predict response to CRT. The study subjects were 48 consecutive patients maintaining sinus rhythm and intrinsic AV conduction who underwent de novo dual-chamber CRT device implantation. CRT responders were defined as those with reductions in left ventricular end-systolic volume >15% at 6 months after CRT device implantations. Twenty-three patients (48%) were CRT responders. In a multivariate analysis, the overlap ratio of the E and A waves was the only independent predictor of response to CRT (odds ratio 1.03, 95% confidence interval 1.01 to 1.06, p = 0.01). Using a cut-off value of 33%, patients with overlap ratios of the E and A waves ≥33% had a significantly higher rate of response to CRT than those with ratios <33% (73% vs 27%, p = 0.002). In conclusion, the overlap ratio of the E and A waves before CRT device implantation may predict CRT response. This simple method may be helpful in evaluating dyssynchrony in patients, particularly with severe reduced left ventricular wall motion, because this method does not require any wall motion analysis.
One of the reasons for a lack of a hemodynamic and functional improvement obtained with cardiac resynchronization therapy (CRT) is that the assessment of atrioventricular (AV) dyssynchrony as well as ventricular-ventricular dyssynchrony before CRT device implantation has been controversial. Left ventricular (LV) diastolic filling time measured by transmitral flow for the cardiac cycle length (DFT/RR) has previously been proposed as a parameter of AV dyssynchrony before CRT device implantation. However, this parameter was not sufficient for predicting CRT response in large clinical trials. In this study, we focused on the degree of overlap of the E and A waves of transmitral flow before CRT device implantation because timely atrial contraction would be desirable, especially in patients with heart failure and reduced LV ejection fractions (LVEFs). We hypothesized that patients with more overlap of the E and A waves of transmitral flow might be better CRT candidates, and we retrospectively investigated predictors of response to CRT.
Methods
Patients were selected for CRT device implantations according to current guidelines and criteria: (1) severe heart failure (New York Heart Association functional class III or IV) despite optimal medical treatment, (2) an LVEF <35%, and (3) prolonged QRS duration (>120 ms). Of 80 consecutive patients who underwent de novo dual-chamber CRT device implantations at 2 institutions from June 2007 to June 2012, patients with external LV assist devices (n = 4), acquired second- or third-degree AV block (n = 7), persistent atrial tachycardia and/or atrial fibrillation (n = 12), and upgraded pacemakers from right ventricular apical pacing (n = 5) and those without follow-up data (n = 4) were excluded from this study. Ultimately, 48 patients maintained in sinus rhythm and with intrinsic AV conduction were retrospectively analyzed. The study protocol conformed to the Declaration of Helsinki and was accepted by each hospital’s ethics committee. Written informed consent was obtained from all patients. All patients underwent baseline evaluations and echocardiographic examinations, including evaluations of dyssynchrony before and 6 months after CRT.
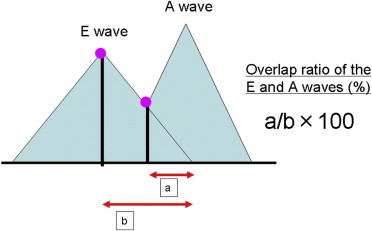
Before hospital discharge, optimization of the AV and ventricular-ventricular intervals was performed by echocardiography or an intracardiac electrocardiographically guided timing cycle optimization algorithm. Echocardiographic images were all obtained before CRT device implantation and 6 months after implantation. LV volumes were determined using the method previously reported. The grade of mitral regurgitation was assessed according to the guidelines of the American Society of Echocardiography. We calculated the overlap ratio of the E and A waves. This overlap ratio was defined as in Figure 1 . In Figure 1 , ‘a’ is the interval between a point of intersection of the E and A waves and the termination of the E wave, while ‘b’ is the interval between the peak of the E wave and the termination of the E wave. The overlap ratio of the E and A waves was calculated as (a/b) × 100%. When the E and A waves were completely separated, the overlap ratio of the E and A waves was 0%. When the E and A waves were totally fused, the overlap ratio was 100%. We determined the level of intraventricular and interventricular mechanical dyssynchrony with using M-mode echocardiography and tissue Doppler imaging. A septal-posterior wall motion delay obtained on M-mode imaging in the parasternal long-axis view of ≥130 ms or the opposing wall delay between the anteroseptal-to-posterior wall or the septal-to-lateral wall of ≥65 ms was defined as intraventricular mechanical dyssynchrony. Interventricular electromechanical delay was the difference between the LV pre-ejection period and the right ventricular pre-ejection period. An interventricular electromechanical delay of ≥40 ms was defined as interventricular dyssynchrony. A reduction in the LV end-systolic volume of >15% at 6 months after CRT was used as an objective measure of response to CRT in this study.
Continuous variables are expressed as mean ± SD. Factors were determined using chi-square tests, and between-group comparisons were made using Mann-Whitney U tests for continuous variables and Fisher’s exact tests for dichotomous variables. Only variables with p values <0.05 on univariate analysis were entered into a multivariate logistic regression analysis to identify independent factors of CRT response. A p value <0.05 was considered statistically significant. Receiver-operating characteristic curves were generated, and the area under the curve was determined as a measure of the ability to predict a positive response at any cut-off value. JMP version 9.0 (SAS Institute Inc., Cary, North Carolina) was used for all statistical tests.
Results
Patient characteristics are listed in Table 1 . β blockers were administered in 47 patients: carvedilol (average dose 8.5 ± 6 mg) in 42 patients, bisoprolol (2.8 ± 0.3 mg) in 2 patients, metoprolol (40 ± 20 mg) in 2 patients, and atenolol (12.5 mg) in 1 patient. The various analyses of the echocardiographic measurements are listed in Table 2 . At 6-month follow-up, 23 patients (48%) were CRT responders. Three patients in the nonresponder group experienced progression to persistent atrial fibrillation, whereas all patients in the responder group maintained sinus rhythm. The 2 groups were generally comparable in terms of baseline demographic, clinical, and echocardiographic characteristics ( Tables 1 and 2 ). The overlap ratio of the E and A waves was higher in the responder group than in the nonresponder group (44 ± 34% vs 19 ± 23%, p = 0.006). New York Heart Association functional class and electrocardiographic and echocardiographic parameters 6 months after CRT device implantation are listed in Table 3 . Significant reductions in heart rate were more frequently observed in the responder group than in the nonresponder group (67 ± 10 vs 76 ± 10 beats/min, p = 0.004), although the incidence of patients increasing the doses of β blockers was similar between the responder group and the nonresponder group (39% vs 36%, p = NS). New York Heart Association functional class improved in 91% of the responders and only 40% of the nonresponders (p = 0.0002). Representative cases in the 2 groups are shown in Figure 2 .
| Variable | Overall (n = 48) | Responders (n = 23) | Nonresponders (n = 25) | p Value |
|---|---|---|---|---|
| Age (yrs) | 59 ± 14 | 64 ± 13 | 55 ± 14 | 0.035 |
| Men | 34 (71%) | 14 (61%) | 20 (80%) | 0.15 |
| CRT defibrillator | 46 (96%) | 21 (91%) | 25 (100%) | 0.13 |
| New York Heart Association class III/IV | 36/12 | 20/3 | 16/9 | 0.067 |
| Nonischemic cardiomyopathy | 37 (77%) | 18 (78%) | 19 (76%) | 0.85 |
| Heart rate (beats/min) | 75 ± 15 | 74 ± 15 | 76 ± 15 | 0.58 |
| PQ interval (ms) | 177 ± 40 | 173 ± 35 | 180 ± 45 | 0.56 |
| QRS duration (ms) | 147 ± 31 | 145 ± 27 | 150 ± 35 | 0.56 |
| Left bundle branch block | 16 (33%) | 11 (48%) | 5 (20%) | 0.048 |
| B-type natriuretic peptide (pg/ml) | 389 ± 326 | 401 ± 409 | 380 ± 244 | 0.83 |
| Medications | ||||
| β blockers | 47 (98%) | 22 (96%) | 25 (100%) | 0.29 |
| Angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers | 37 (77%) | 19 (83%) | 18 (72%) | 0.38 |
| Spironolactone | 32 (67%) | 16 (70%) | 16 (64%) | 0.68 |
| Diuretics | 41 (85%) | 17 (74%) | 24 (96%) | 0.030 |
| Amiodarone | 17 (35%) | 7 (30%) | 10 (40%) | 0.48 |
| Digoxin | 8 (17%) | 4 (17%) | 4 (16%) | 0.89 |
| Intravenous inotropic agents | 10 (21%) | 2 (9%) | 8 (32%) | 0.047 |
| Variable | Overall (n = 48) | Responders (n = 23) | Nonresponders (n = 25) | p Value |
|---|---|---|---|---|
| LVEF (%) | 26 ± 7 | 28 ± 6 | 23 ± 8 | 0.04 |
| LV end-diastolic volume (ml) | 247 ± 88 | 239 ± 78 | 254 ± 97 | 0.56 |
| LV end-systolic volume (ml) | 184 ± 82 | 173 ± 66 | 195 ± 94 | 0.37 |
| Left atrial dimension (mm) | 46 ± 8 | 45 ± 8 | 47 ± 7 | 0.45 |
| Mitral regurgitation grade ≥II | 28 (58%) | 13 (57%) | 15 (60%) | 0.81 |
| Deceleration time of the E wave (ms) | 182 ± 64 | 190 ± 49 | 173 ± 75 | 0.35 |
| Tei index | 0.56 ± 0.15 | 0.56 ± 0.15 | 0.56 ± 0.16 | 0.97 |
| DFT/RR | 0.47 ± 0.07 | 0.47 ± 0.07 | 0.46 ± 0.07 | 0.87 |
| DFT/RR <0.4 | 9 (19%) | 4 (17%) | 5 (20%) | 0.82 |
| Overlap ratio of the E and A waves (%) | 30 ± 31 | 44 ± 34 | 19 ± 23 | 0.006 |
| Septal posterior wall motion delay >130 ms | 20/33 (61%) | 13/19 (68%) | 7/14 (50%) | 0.28 |
| Interventricular mechanical delay >40 ms | 14/36 (39%) | 9/20 (45%) | 5/16 (31%) | 0.40 |
| Ts (anteroseptal-posterior, septal-lateral) >65 ms | 14/27 (52%) | 7/15 (47%) | 7/12 (58%) | 0.55 |
| Variable | Overall (n = 48) | Responders (n = 23) | Nonresponders (n = 25) | p Value |
|---|---|---|---|---|
| New York Heart Association class I/II/III/IV | 6/21/14/7 | 6/14/3/0 | 0/7/11/7 | 0.002 |
| Heart rate (beats/min) | 72 ± 11 | 67 ± 10 | 76 ± 10 | 0.004 |
| PQ interval (ms) | 158 ± 47 | 139 ± 30 | 173 ± 53 | 0.01 |
| QRS duration (ms) | 141 ± 22 | 141 ± 23 | 142 ± 22 | 0.95 |
| B-type natriuretic peptide (pg/ml) | 324 ± 361 | 135 ± 129 | 505 ± 418 | 0.0003 |
| Echocardiographic parameters | ||||
| LVEF (%) | 31 ± 12 | 40 ± 9 | 22 ± 6 | 0.0001 |
| Deceleration time of the E wave (ms) | 185 ± 66 | 202 ± 52 | 170 ± 75 | 0.11 |
| DFT/RR | 0.48 ± 0.08 | 0.50 ± 0.07 | 0.46 ± 0.08 | 0.08 |
| Overlap ratio of the E and A waves (%) | 13 ± 23 | 10 ± 16 | 16 ± 28 | 0.36 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


