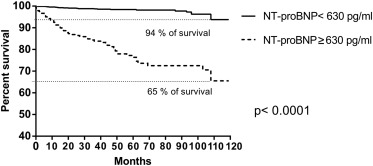
Natriuretic peptides are often elevated in congenital heart disease (CHD); however, the clinical impact on mortality is unclear. The aim of our study was to evaluate the prognostic value of N -terminal pro-brain natriuretic peptide (NT-proBNP) in the prediction of all-cause mortality in adults with different CHD. In this prospective longitudinal mortality study, we evaluated NT-proBNP in 1,242 blood samples from 646 outpatient adults with stable CHD (mean age 35 ± 12 years; 345 women). Patients were followed up for 6 ± 3 (1 to 10) years. The mortality rate was 5% (35 patients, mean age 40 ± 14 years, 17 women). Median NT-proBNP (pg/ml) was 220 in the whole cohort, 203 in survivors, and 1,548 in deceased patients. The best discrimination value for mortality prediction was 630 pg/ml with 74% sensitivity and 84% specificity. During the follow-up, the survival rate was 65% for those with median NT-proBNP ≥630 pg/ml and 94% for NT-proBNP <630 pg/ml; p <0.0001. There was only 1% mortality among 388 patients with at least 1 NT-proBNP value ≤220 pg/ml compared with 41% mortality among 54 patients with at least 1 NT-proBNP value >1,548 pg/ml. Even the first (baseline) measurements of NT-proBNP were strongly associated with a high risk of death (log 10 NT-proBNP had hazard ratio 7, p <0.0001). In conclusion, NT-proBNP assessment is a useful and simple tool for the prediction of mortality in long-term follow-up of adults with CHD.
Natriuretic peptides are powerful independent markers of prognosis in patients with symptomatic or asymptomatic heart failure, coronary artery disease, pulmonary hypertension, acquired valve disease, and general population but not in the healthy population without cardiovascular risk factors. Patients with low level of N -terminal pro-brain natriuretic peptide (NT-proBNP) have excellent prognosis irrespective of echocardiographic findings. For patients with advanced chronic heart failure, natriuretic peptides have been accepted as a gold standard in predicting mortality. It is less clear which levels of NT-proBNP may be considered normal and which have negative prognostic impact in the population of adults with congenital heart disease (ACHD). The average (reference) values of NT-proBNP for the main congenital heart diagnoses in adulthood were proposed by 2 larger studies. The usefulness of natriuretic peptides for mortality prediction in ACHD has been studied in smaller studies for specific complex lesions. The aim of our study was to assess the prognostic value of NT-proBNP for mortality prediction in a large cohort of ACHD during long-term follow-up. To the best of our knowledge, this is the largest study in ACHD evaluating NT-proBNP in mortality prediction.
Methods
During the period 2003 to 2013, we measured NT-proBNP prospectively in 646 consecutive adults with different congenital heart lesions referred to our center. All blood samples were obtained during the planned outpatient visit. Only adult patients in stable state were included in this study; those referred to hospitalization with manifest heart failure or arrhythmia during the first visit were excluded. Patients with renal failure and creatinine level >160 μmol/l were not included in the study.
The first NT-proBNP measurement was considered baseline. Repeated NT-proBNP assessments were performed during the controls in our center. All patients were regularly followed up either in our tertiary referral center for ACHD or by local cardiologists. The mortality rate of our patients was confirmed by the confrontation of all patients with the National Mortality Register. If the death happened outside the hospital, we tried to find out the cause of the death by a telephone call to the family, local cardiologist, or general practitioner.
Blood samples for NT-proBNP were withdrawn during the outpatient visit in the morning in a sitting position at rest from a peripheral vein together with blood samples for routine biochemistry and blood count evaluation. Serum samples were analyzed immediately after the transport to the laboratory. Serum levels of NT-proBNP were measured using commercially available electrochemiluminescence sandwich immunoassay (Elecsys 2010; Roche, Mannheim, Germany).
The Kaplan–Meier analysis with the log-rank Mantel–Cox test was used for evaluation of survival curves. The negative and positive predictive values, sensitivity, specificity, and area under the curve (AUC) were assessed for different NT-proBNP cut-off values. The effect of log 10 NT-proBNP on survival was assessed by Cox proportional hazard ratio (HR) analysis and resulting significance, HR, and confidence intervals of HR were reported; fulfillment of Cox proportional hazards assumptions were tested using R function cox.zph. The Mann–Whitney U test was used to compare the differences in NT-proBNP values between survivors and deceased patients. The value of p <0.05 was considered statistically significant. The GraphPad Prism version 6.0 (San Diego, California) and R software version 3.1.2 were used to perform the statistical analysis.
The study was approved by the local ethics committee. All patients were informed about the purpose of NT-proBNP assessment and gave their informed consent with the NT-proBNP analysis.
Results
The mean follow-up was 6 ± 3 (1 to 10) years in the period between 2003 and 2013. The mean age of our patients was 35 ± 12 years (18 to 79 years), there were 301 men and 345 women. The overview of different CHD diagnoses, number of patients and blood samples, history of repair, and deaths are summarized in Table 1 .
| Diagnosis | Pts | N of NT-proBNP samples | Pts after repair N (%) | Pts without radical repair N (%) | N of deaths/ deaths after radical repair | Rate of deaths within dg group | Rate of deaths within all 35 deaths |
|---|---|---|---|---|---|---|---|
| Pulmonary atresia | 24 | 46 | 18 (75 %) | 6 (25 %) | 2/2 | 8 % | 6 % |
| Congenitally corrected transposition of the great arteries | 22 | 43 | 9 (41 %) | 13 (59 %) | 0 | 0 | 0 |
| Ventricular septal defect ∗ | 34 | 57 | 22 (65 %) | 12 (35 %) | 0 | 0 | 0 |
| Fontan correction † | (27) | (57) | (27) (100 %) | 0 (0) | 0 | 0 | 0 |
| Single ventricle † incl. Tricuspid atresia | 48 | 92 | 31 (65 %) | 17 (35 %) | 5/1 | 10 % | 14 % |
| Eisenmenger syndrome or severe pulmonary hypertension ∗ | 51 | 106 | 15 (29 %) | 36 (71 %) | 6/2 | 12 % | 17 % |
| Coarctation of the aorta | 25 | 38 | 22 (88 %) | 3 (12 %) | 0 | 0 | 0 |
| Ebstein anomaly | 49 | 120 | 31 (63 %) | 18 (37 %) | 6/3 | 12 % | 17 % |
| Transposition of the great arteries | 86 | 185 | 84 (98 %) | 2 (2 %) | 9/8 | 10 % | 26 % |
| Tetralogy of Fallot | 96 | 188 | 92 (96 %) | 4 (4 %) | 2/1 | 2 % | 6 % |
| Atrial septal defect | 90 | 142 | 57 (63 %) | 33 (37 %) | 1/1 | 1 % | 2.8 % |
| Atrio-ventricular septal defect | 29 | 50 | 25 (86 %) | 4 (14 %) | 3/3 | 10 % | 8.6 % |
| Truncus arteriosus | 3 | 3 | 3 (100 %) | 0 | 0 | 0 | 0 |
| Pulmonary stenosis | 29 | 44 | 23 (79 %) | 6 (21 %) | 1/1 | 3% | 2.8 % |
| Congenital aortic valve disease | 56 | 118 | 16 (29 %) | 40 (71 %) | 0 | 0 | 0 |
| Other | 4 | 10 | 3 (75 %) | 1 (25 %) | 0 | 0 | 0 |
| Together | 646 | 1242 | 451 (70 %) | 195 (30 %) | 35/22 | 100 % |
∗ Patients with ventricular septal defect, atrial septal defect, or any other lesion with severe pulmonary hypertension are included only in the Eisenmenger group.
† All patients with Fontan correction are included also in the single ventricle group.
Most patients (70%) had a history of radical repair of their CHD, mostly in childhood (58%), less frequently in adulthood (12%); the remaining 30% did not have any operation or had only a palliative shunt. The group with unrepaired CHD comprised patients with severe inoperable lesions and patients with mild lesions not indicated for surgery. Most patients (81%) were only mildly symptomatic (New York Heart Association [NYHA] classes I to II) and 19% had NYHA classes III to IV. Cyanosis with oxygen saturation ≤90% was present in 7% of patients without radical correction (Eisenmenger syndrome, Ebstein anomaly, functionally single ventricle or palliated tetralogy of Fallot). All our patients had normal creatinine levels except one with mild renal failure and serum creatinine 150 μmol/l. Repeated NT-proBNP assessment was performed in 46% of the whole cohort (295 patients).
Thirty-five patients (5%) died during follow-up at the mean age of 40 ± 14 years, 17 were women. The most frequent diagnoses in the deceased group were transposition of the great arteries after Mustard or Senning correction or without correction (26% of deaths), Ebstein anomaly (17%), Eisenmenger syndrome or severe pulmonary hypertension (17%), and unoperated or palliated complex CHD with functionally single ventricle (14% of deaths; Table 1 ). Interestingly, there was no death in the Fontan group of patients. Low or zero mortality was found also in coarctation of the aorta, tetralogy of Fallot, pulmonary stenosis, atrial septal defect type secundum, congenitally corrected transposition of the great arteries, ventricular septal defect, and congenital aortic valve disease ( Table 1 ). The cause of death was cardiovascular in 97%. Most patients (28; 80%) died from heart failure either without relation to operation (25 patients) or in the early postoperative period (3 patients). Other causes of death were arrhythmia or sudden death (3 patients), hemoptysis (1 patient), stroke (1 patient), complication of ventricular assist device (1 patient), and tumor (1 patient).
The median of NT-proBNP was 220 (interquartile range 110 to 474) pg/ml in the whole cohort, 203 (101 to 420) pg/ml in the group of survivors, and 1,548 (473 to 3,828) pg/ml in the group of deceased patients ( Table 2 ). The difference between survivors and deceased patients was highly significant (p <0.0001; Mann–Whitney U test). The median values of NT-proBNP in survivors and deceased patients with particular congenital heart diagnoses are listed in Table 3 .
| NT-proBNP cut-off (pg/ml) | Type of cut-off | Samples | Sensitivity | Specificity | PPV | NPV | AUC |
|---|---|---|---|---|---|---|---|
| 220 | Median of all samples | 1242 | 92 % | 53 % | 10 % | 99 % | 0.85 |
| 1548 | Median of deceased | 77 | 49 % | 93 % | 36 % | 97 % | |
| 203 | Median of survivors | 1165 | 94 % | 51 % | 10 % | 99 % | |
| 630 | Maximal sensitivity and specificity | 1242 | 74 % | 84 % | 18 % | 98 % |
| Diagnosis | Survivors | Deceased | ||
|---|---|---|---|---|
| NT-proBNP (pg/ml) | Patients | NT-proBNP (pg/ml) | Patients | |
| Pulmonary atresia | 296 | 22 | 3264 | 2 |
| Congenitally corrected transposition of the great arteries | 211 | 22 | – | 0 |
| Ventricular septal defect ∗ | 170 | 34 | – | 0 |
| Fontan correction † | 220 | (27) | – | 0 |
| Single ventricle † incl. Tricuspid atresia | 470 | 43 | 1184 | 5 |
| Eisenmenger syndrome or severe pulmonary hypertension ∗ | 351 | 45 | 2706 | 6 |
| Coarctation of the aorta | 101 | 25 | – | 0 |
| Ebstein anomaly of the tricuspid valve | 250 | 43 | 304 | 6 |
| Transposition of the great arteries | 220 | 77 | 4352 | 9 |
| Tetralogy of Fallot | 183 | 94 | 300 | 2 |
| Atrial septal defect | 206 | 89 | 2410 | 1 |
| Atrio-ventricular septal defect | 195 | 26 | 1548 | 3 |
| Truncus arteriosus | 144 | 3 | – | 0 |
| Pulmonary stenosis | 101 | 28 | 1412 | 1 |
| Congenital aortic valve disease | 118 | 56 | – | 0 |
| Other | 80 | 4 | – | 0 |
| Together | 203 | 611 | 1548 | 35 |
∗ Patients with ventricular septal defect, atrial septal defect, or any other lesion with severe pulmonary hypertension are included only in the Eisenmenger group.
† All patients with Fontan correction are included also in the single ventricle group.
The optimal discrimination value of NT-proBNP for the prediction of death was 630 pg/ml with 74% sensitivity, 84% specificity, 18% positive predictive value, and 98% negative predictive value. The optimal discrimination value was estimated at a value of maximal specificity and sensitivity. The AUC was 0.85 ( Table 2 ). The long-term survival rate was 94% in the group with NT-proBNP <630 pg/ml compared to 65% survival rate in patients with NT-proBNP ≥630 pg/ml, p <0.0001 ( Figure 1 ).
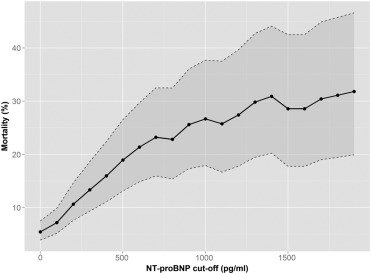
The use of median of all samples (220 pg/ml) as the discrimination value for mortality had higher sensitivity (92%) but lower specificity (53%). The cutoff 1,548 pg/ml had high specificity (93%) but lower sensitivity (49%; Table 2 ). There was only 1% mortality (4 patients) in the 388 patients who had at least 1 of their NT-proBNP value ≤220 pg/ml. On the contrary, the mortality rate was as high as 41% (22 deceased patients) in 54 patients with at least 1 NT-proBNP value >1,548 pg/ml during the follow-up. The relation between different NT-proBNP cut-off values and the mortality is shown in Figure 2 .
Maximal NT-proBNP was highly predictive of mortality (AUC 0.87) with significantly different survival curves for cut-off value of 630 pg/ml (p <0.0001; Table 4a ). Interestingly, also the baseline NT-proBNP was similarly predictive (AUC 0.85) with significantly different survival curves for cut-off value of 630 pg/ml (p <0.0001; Table 4b ).



