There is currently no reliable method of predicting the success of weaning from intra-aortic balloon pumping (IABP). The aim of this study was to investigate the ability of serum N-terminal pro–brain natriuretic peptide (NT-proBNP) level to predict the success of weaning from IABP. Consecutive patients scheduled for weaning from IABP were prospectively enrolled. NT-proBNP levels were measured at baseline (before the start of weaning) and cessation (just before cessation of IABP). Changes in NT-proBNP level between baseline and cessation were analyzed in 2 groups of patients: those who were successfully weaned and those who were not successfully weaned for any reason, including a decision to discontinue weaning, worsening of pulmonary edema after cessation of IABP, or unstable hemodynamics after cessation of IABP. A total of 30 patients were enrolled (mean age 66 ± 12 years, 16 men, 16 with acute myocardial infarctions, and 14 with acute exacerbation of chronic heart failure). Median (interquartile range) baseline NT-proBNP levels were not significantly different between the successful and unsuccessful weaning groups (4,200 [1,400 to 8,752] pg/ml vs (5,620 [2,035 to 13,950] pg/ml, p = 0.30). In the unsuccessful weaning group, the median NT-proBNP level was significantly higher at cessation (9,995 [2,920 to 15,100] pg/ml) than at baseline (p = 0.008). All patients with decreases in NT-proBNP level between baseline and cessation were successfully weaned from IABP. In conclusion, these results show that NT-proBNP levels were useful for predicting the success of weaning from IABP. If the NT-proBNP level increases during weaning from IABP, more intense management should be considered.
Natriuretic peptide levels are used to diagnose heart failure and to predict prognosis and determine the efficacy of treatment in patients with heart failure. Changes in natriuretic peptide levels can reflect changes in hemodynamic status, such as a treatment-induced decrease or stress-induced increase in pulmonary capillary wedge pressure in patients with heart failure. In this study, we investigated whether serum N-terminal pro–brain natriuretic peptide (NT-proBNP) level is useful for predicting the success of weaning from intra-aortic balloon pumping (IABP). The ability of empirical markers to predict the success of weaning was also investigated, including urine volume, blood pressure, heart rate, and serum bilirubin level.
Methods
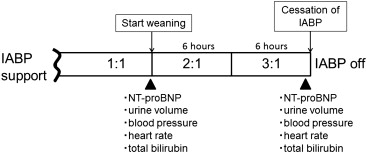
Consecutive patients scheduled for weaning from IABP in the cardiac care unit of Nippon Medical School Hospital from May 2008 to December 2009 were prospectively enrolled. This study was approved by our institutional ethics committee, and informed consent was obtained from all patients. The IABP weaning protocol at our hospital, which was used in this study, is shown in Figure 1 . NT-proBNP level and empirical markers (urine volume, blood pressure, heart rate, and total serum bilirubin level) were measured at baseline (before the start of weaning) and cessation (just before cessation of IABP). Serum NT-proBNP level was measured using an electrochemiluminescence immunoassay (Elecsys proBNP; Roche Diagnostics, Tokyo, Japan). The baseline IABP assist ratio of 1:1 was changed to 2:1 for 6 hours and then to 3:1 for 6 hours, after which IABP was discontinued and the pump removed. Decisions to discontinue weaning were made by the attending physician according to each patient’s clinical status. The attending physician was blinded to NT-proBNP level. The clinical courses of all patients were monitored until 24 hours after cessation of IABP.
Patients were classified into 2 groups: those who were successfully weaned from IABP and those who were not successfully weaned. Weaning was considered unsuccessful if it was discontinued for any reason, if there was worsening of pulmonary edema requiring increased oxygen supplementation or initiation of mechanical ventilation <24 hours after cessation of IABP, or if unstable hemodynamics required increased use of inotropic agents <24 hours after cessation of IABP.
The NT-proBNP level is expressed as median (interquartile range), and other continuous variables are expressed as mean ± SD. The Mann-Whitney U test was used to compare NT-proBNP levels between the successful and unsuccessful weaning groups, and Wilcoxon’s signed-rank test was used to compare baseline and cessation NT-proBNP levels within each group. Other differences between the 2 groups were compared using Student’s t test for continuous variables or the chi-square test for categorical variables. Receiver-operating characteristic curve analysis was used to determine the threshold of percentage change in NT-proBNP level for failure to wean. All statistical analyses were performed using SPSS version 18 (SPSS, Inc, Chicago, Illinois). A p value <0.05 was considered statistically significant.
Results
A total of 30 patients were enrolled (mean age 66 ± 12 years, 16 men, 14 women). Weaning from IABP was successful in 20 patients and unsuccessful in 10. The reasons for unsuccessful weaning were discontinuation of weaning because of worsening of pulmonary edema in 4 patients, worsening of pulmonary edema requiring the initiation of noninvasive positive-pressure ventilation after cessation of IABP in 3 patients, and unstable hemodynamics requiring increased inotropic support after cessation of IABP in 3 patients. There were no significant differences in baseline characteristics, including indication for IABP, between the successful and unsuccessful weaning groups ( Table 1 ).
| Group | Age (years) | Sex | Diagnosis | Indication of IABP | Duration of IABP Support (days) | EF (%) | sCr (mg/dl) | Augmented BP (mmHg) | MBP (mmHg) | Heart rate (bpm) | NT-proBNP at Baseline (pg/ml) | NT-proBNP at Cessation (pg/ml) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S | 40 | M | AMI | RHF | 8 | 47 | 0.79 | 116 | 86 | 92 | 3160 | 2670 |
| S | 54 | M | AMI | Shock | 3 | 35 | 0.90 | 100 | 65 | 80 | 957 | 612 |
| S | 57 | F | CHF (DC) | RHF | 7 | 25 | 1.02 | 92 | 62 | 80 | 9540 | 8180 |
| S | 57 | F | CHF (DC) | RHF | 11 | 44 | 0.72 | 88 | 58 | 90 | 3910 | 4100 |
| S | 60 | M | AMI | Shock | 2 | 40 | 0.74 | 112 | 89 | 72 | 944 | 773 |
| S | 60 | F | CHF (IC) | RHF | 6 | 23 | 1.81 | 160 | 77 | 64 | 13200 | 14800 |
| S | 61 | M | AMI | Shock | 2 | 17 | 0.96 | 100 | 70 | 72 | 8490 | 7140 |
| S | 61 | M | AMI | RHF | 2 | 57 | 1.08 | 92 | 65 | 72 | 1120 | 1630 |
| S | 62 | M | CHF (HHD) | RHF | 6 | 31 | 0.84 | 140 | 100 | 72 | 925 | 1000 |
| S | 63 | F | CHF (IC) | RHF | 2 | 15 | 0.70 | 112 | 64 | 68 | 1190 | 933 |
| S | 65 | F | AMI | Shock | 2 | 38 | 0.73 | 112 | 69 | 112 | 5410 | 4530 |
| S | 67 | M | CHF (DC) | RHF | 12 | 21 | 1.77 | 104 | 61 | 92 | 73600 | 54400 |
| S | 68 | M | CHF (IC) | RHF | 2 | 32 | 4.22 | 128 | 69 | 72 | 9570 | 11000 |
| S | 72 | M | AMI | Shock | 2 | 27 | 0.78 | 148 | 94 | 64 | 1470 | 2440 |
| S | 72 | M | AMI | RHF | 4 | 34 | 0.80 | 124 | 76 | 72 | 4490 | 5490 |
| S | 72 | F | AMI | Shock | 7 | 42 | 0.73 | 128 | 82 | 100 | 9740 | 10500 |
| S | 75 | M | AMI | RHF | 7 | 46 | 1.00 | 152 | 90 | 88 | 2070 | 2120 |
| S | 79 | F | AMI | Shock | 3 | 40 | 0.74 | 132 | 70 | 88 | 1720 | 1750 |
| S | 84 | F | AMI | Shock | 3 | 64 | 1.22 | 100 | 57 | 76 | 8230 | 4250 |
| S | 87 | M | AMI | Shock | 3 | 46 | 2.65 | 130 | 79 | 68 | 7670 | 8810 |
| US | 40 | M | AMI | RHF | 4 | 45 | 0.83 | 100 | 76 | 76 | 1120 | 1660 |
| US | 57 | F | CHF (DC) | RHF | 8 | 25 | 0.99 | 90 | 68 | 80 | 8060 | 9790 |
| US | 58 | F | CHF (DC) | RHF | 18 | 25 | 0.73 | 112 | 61 | 68 | 3040 | 10200 |
| US | 58 | F | CHF (DC) | RHF | 6 | 27 | 0.90 | 100 | 65 | 70 | 1700 | 2920 |
| US | 65 | M | AMI | Shock | 9 | 22 | 0.49 | 104 | 78 | 92 | 14000 | 15100 |
| US | 67 | M | CHF (DC) | RHF | 6 | 23 | 1.98 | 110 | 60 | 104 | 113000 | 146000 |
| US | 67 | F | CHF (DC) | RHF | 3 | 16 | 0.32 | 96 | 60 | 80 | 1620 | 1870 |
| US | 77 | M | CHF (IC) | RHF | 3 | 36 | 1.00 | 126 | 82 | 72 | 3180 | 4340 |
| US | 79 | F | CHF (IC) | RHF | 3 | 68 | 1.71 | 140 | 84 | 88 | 13800 | 13800 |
| US | 92 | F | AMI | Shock | 4 | 27 | 1.03 | 104 | 61 | 126 | 18600 | 20000 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


