In many patients with left ventricular (LV) systolic dysfunction, the LV ejection fraction (LVEF)—a surrogate for reverse remodeling—fails to improve despite optimal medical therapy. The early identification of such patients would allow instituting aggressive treatment, including early therapy with implantable cardioverter defibrillators. We sought to establish the predictors of reverse remodeling in patients with LV systolic dysfunction receiving optimal medical therapy. Patients (n = 568) with newly documented LVEF of ≤0.35, who had ≥1 follow-up echocardiogram after ≥3 months, were evaluated. Reverse remodeling was defined as improvement in LVEF to >0.35. The clinical, laboratory, and echocardiographic data were compared between patients with (n = 263) and without (n = 305) reverse remodeling. The mean follow-up was 27 ± 16 months. Patients who demonstrated reverse remodeling had a significantly greater mean follow-up LVEF (0.51 ± 0.09 vs 0.25 ± 0.08; p <0.001). On multivariate analysis, the baseline LV end-systolic diameter index was the strongest predictor of reverse remodeling (odds ratio 5.79; 95% confidence interval 1.82 to 18.46; p <0.001). Other independent predictors of reverse remodeling were female gender (odds ratio 1.88; 95% confidence interval 1.19 to 2.98; p = 0.007), and nonischemic cardiomyopathy (odds ratio 1.65; 95% confidence interval 1.05 to 2.58; p = 0.03). Baseline LVEF was not an independent predictor of reverse remodeling. In conclusion, among patients with newly diagnosed LV systolic dysfunction, the LV end-systolic diameter index, but not the LVEF, at diagnosis, was a strong predictor of reverse remodeling. Patients with a low likelihood of reverse remodeling might benefit from more aggressive heart failure therapy, including the possible early use of implantable cardioverter defibrillators.
Predicting whether a patient with left ventricular (LV) systolic dysfunction is likely to undergo reverse remodeling is challenging. Small studies evaluating the baseline LV size as a predictor, not only yielded conflicting results, but were also performed in the era when the combined use of angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARBs) and β blockers was not widespread. Although β blockers and/or ACE inhibitors have been demonstrated to result in reverse remodeling, despite their combined use, reverse remodeling does not occur in a number of patients with systolic heart failure. Although a number of studies have evaluated reverse remodeling after cardiac resynchronization therapy, a paucity of data is available in patients with LV systolic dysfunction who are only receiving optimal medical therapy with both ACE inhibitors/ARBs and β blockers. The early identification of patients whose LV systolic function will not improve might allow for more aggressive therapy, such as the use of implantable cardioverter defibrillators (ICDs) earlier in the disease course. Therefore, the aims of our study were to evaluate the incidence of LV reverse remodeling in patients with LV systolic dysfunction optimally treated with ACE inhibitors/ARBs and β blockers and to determine the predictors of LV reverse remodeling.
Methods
This was a retrospective study conducted at the MetroHealth Campus of Case Western Reserve University in Cleveland, Ohio. The local institutional review board approved the study. The echocardiographic hospital database was used to identify all patients who underwent echocardiography for the evaluation of clinical signs and symptoms of heart failure and had a newly documented left ventricular ejection fraction (LVEF) of ≤0.35. From this group, all patients who had ≥1 follow-up echocardiogram done ≥3 months after the index echocardiogram were included in the present study. The echocardiograms were read by the staff cardiologists not directly involved in the care of the study patients, and the LVEF was measured using the biplane area-length method. In our study, reverse remodeling was defined as an improvement in LVEF to >0.35 at last follow-up echocardiogram.
The patients were categorized into 2 groups: those who demonstrated reverse remodeling (reverse remodeling [+RR] group) and those who did not (no reverse remodeling [−RR] group). The clinical, electrocardiographic, and laboratory variables were recorded at both the baseline and the follow-up echocardiographic visit and were compared between the 2 groups. The variables included age, gender, race, history of hypertension, etiology of cardiomyopathy (ischemic or nonischemic), and QRS duration. The use of ACE inhibitors/ARBs and β blockers, including their doses, were recorded for each visit. The echocardiographic chamber dimensions obtained from 2-dimensional recordings (parasternal long-axis view) were normalized for body surface area to obtain the LV end-diastolic diameter index (LVEDDI) and LV end-systolic diameter index (LVESDI). The percentage of change in the LVEDDI and LVESDI between the initial and final echocardiogram was recorded. Mitral regurgitation was assessed semiquantitatively by color Doppler echocardiography and graded as mild, moderate, or severe. It was considered significant if it was moderate or greater. Patients were excluded if the LV dimensions could not be measured accurately or if they had received cardiac resynchronization therapy during the study period.
Ischemic cardiomyopathy was defined as either the presence of an obstructive coronary lesion (≥70% diameter narrowing) or a history of revascularization (percutaneous coronary intervention or coronary artery bypass grafting) in ≥1 of the 3 major coronary arteries. Nonischemic cardiomyopathy was defined as the absence of ischemic cardiomyopathy according to the above criteria. The target doses of β blockers and ACE inhibitors/ARBs were defined in accordance with the current best evidence (i.e., metoprolol ≥200 mg/day; carvedilol ≥50 mg/day; lisinopril 40 mg/day; valsartan 320 mg/day; and losartan 100 mg/day).
The categorical variables are reported as counts and percentages and were compared using chi-square statistics. Continuous variables are presented as the mean ± SD and were compared using Student’s t test or the Wilcoxon nonparametric statistic. A p value of <0.05 was considered statistically significant. The clinical, laboratory, and echocardiographic variables were initially evaluated individually and, if found significant, were analyzed using a multivariate logistic regression model. Odds ratios were calculated to determine the independent predictors of reverse remodeling. The data were analyzed using PASW Statistics, version 18 (SPSS, Chicago, Illinois).
Results
A total of 700 patients were identified with a documented LVEF of ≤0.35 and a follow-up echocardiogram performed ≥3 months later. A total of 32 patients who received cardiac resynchronization therapy were excluded and another 100 were excluded for the lack of data on LV dimensions. The remaining 568 patients were included in the present study. The duration of heart failure symptoms before the first echocardiogram was 4 ± 9 months, and the duration of follow-up was 27 ± 16 months. The cause of cardiomyopathy was ischemic in 230 patients (40%) and nonischemic in 338 (60%). A total of 256 patients (45%) in our study were black. Most patients (n = 542; 95%) were taking both an ACE inhibitor/ARB and a β blocker at baseline.
A total of 263 patients (46%) exhibited reverse remodeling, and the remaining 305 (54%) did not. The clinical and electrocardiographic characteristics of the 2 groups are listed in Table 1 . A history of hypertension was more common in the +RR group, and the use of digoxin and diuretics was more common in the −RR group. The use of ACE inhibitors/ARBs and β blockers, including their target doses, was similar in both groups. In the +RR group, 131 patients (50%) were receiving the target dose of ACE inhibitors/ARBs and 123 (47%) the target β-blocker dose. The corresponding data for the −RR group were 143 (47%) for ACE inhibitors/ARBs and 132 (43%) for β blockers.
| Variable | Reverse Remodeling | p Value | |
|---|---|---|---|
| Yes (n = 263) | No (n = 305) | ||
| Age (years) | 57 ± 14 | 58 ± 14 | 0.57 |
| Women | 119 (45%) | 110 (36%) | 0.02 |
| Race | 0.16 | ||
| White | 125 (47%) | 132 (43%) | |
| Black | 108 (41%) | 148 (48%) | |
| Diabetes mellitus | 98 (37%) | 106 (35%) | 0.08 |
| Hypertension | 210 (80%) | 219 (72%) | 0.02 |
| Cardiomyopathy | 0.01 | ||
| Ischemic | 98 (37%) | 142 (47%) | |
| Nonischemic | 165 (63%) | 163 (53%) | |
| History of myocardial infarction | 35 (13%) | 49 (16%) | 0.16 |
| Duration of heart failure (months) | 3 ± 7 | 5 ± 10 | 0.17 |
| Atrial fibrillation/flutter | 44 (17%) | 48 (16%) | 0.45 |
| Heart rate (beats/min) | 86 ± 19 | 83 ± 18 | 0.23 |
| Systolic blood pressure (mm Hg) | 133 ± 23 | 128 ± 25 | 0.007 |
| Diastolic blood pressure (mm Hg) | 72 ± 17 | 69 ± 18 | 0.06 |
| New York Heart Association functional class | 3.05 ± 0.97 | 3.02 ± 0.96 | 0.73 |
| B-type natriuretic peptide (pg/ml) | 1,126 ± 658 | 1,001 ± 631 | 0.85 |
| Medications | |||
| β Blocker | 251 (95%) | 291 (95%) | 0.57 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 249 (95%) | 285 (93%) | 0.33 |
| Digoxin | 78 (30%) | 158 (52%) | <0.001 |
| Diuretics | 195 (74%) | 255 (84%) | 0.004 |
| Nitrates | 102 (39%) | 134 (44%) | 0.12 |
| Hydralazine | 75 (28%) | 87 (28%) | 0.49 |
| Baseline QRS (ms) | 109 ± 30 | 113 ± 30 | 0.04 |
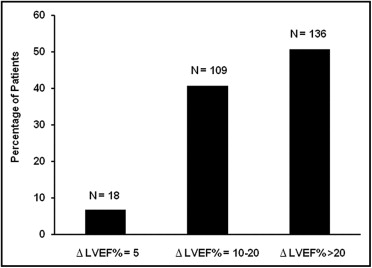
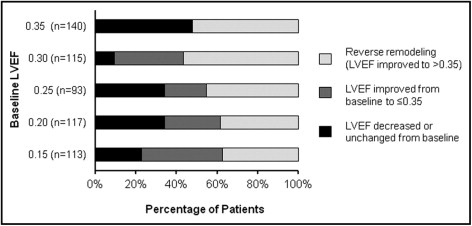
The mean baseline LVEF was 0.27% in the +RR group and 0.25 in the −RR group ( Table 2 ). Patients in the +RR group had a lower baseline LVEDDI and LVESDI. The 2 groups were similar with respect to the follow-up duration and the number of follow-up echocardiograms. At follow-up, 263 patients (46%) achieved an LVEF >0.35 and 143 of them (25% of all patients) achieved an LVEF of ≥0.50. The patients in the +RR group had a significantly greater follow-up LVEF and a significant reduction in both LVEDDI and LVESDI ( Table 2 ). Of the 263 patients who demonstrated reverse remodeling, 245 patients (93%) demonstrated a clinically meaningful increase in LVEF of ≥10% ( Figure 1 ) . Also, patients in the +RR group were distributed across a number of baseline LVEFs and not limited to those with the greatest baseline LVEF ( Figure 2 ) .
| Variable | Reverse remodeling | p value | |
|---|---|---|---|
| Yes | No | ||
| Follow-up (months) | 25 ± 14 | 28 ± 17 | 0.06 |
| Total number of follow-up echocardiograms | 2.5 ± 0.6 | 2.5 ± 0.7 | 0.84 |
| Left ventricular ejection fraction (%) | |||
| Baseline | 27 ± 7 | 25 ± 7 | 0.001 |
| Final | 51 ± 9 | 25 ± 8 | <0.001 |
| Left ventricular end-diastolic diameter index | |||
| Baseline (cm/m 2 ) | 2.73 ± 0.46 | 3.02 ± 0.53 | <0.001 |
| Percentage of change between baseline and final | −6.3 ± 15.9 | 0.68 ± 12.0 | <0.001 |
| Left ventricular end-systolic diameter index | |||
| Baseline (cm/m 2 ) | 2.28 ± 0.47 | 2.58 ± 0.52 | <0.001 |
| Percentage of change between baseline and final | −15.1 ± 21.1 | 1.69 ± 16.4 | <0.001 |
| Left ventricular mass index (g/m 2 ) | 138 ± 47 | 149 ± 43 | 0.001 |
| Significant mitral regurgitation | 38 (14%) | 63 (21%) | 0.03 |
When we evaluated the study population for events that could potentially influence reverse remodeling during the follow-up period, we found no difference in the 2 groups with respect to the rates of acute myocardial infarction occurring at enrollment (+RR, 18 [7%] vs −RR, 20 (6%); p = NS), the rates of acute myocardial infarction during the follow-up period (+RR 10 [4%] vs −RR 16 [5%]; p = NS); or the rates of revascularization procedures during the study period (+RR, 40 [15%] vs −RR, 39 [13%]; p = NS).
The univariate predictors of reverse remodeling were female gender, history of hypertension, presence of nonischemic cardiomyopathy, digoxin use, diuretic use, baseline QRS duration, baseline systolic blood pressure, and baseline echocardiographic variables (i.e., LVEF, rates of significant mitral regurgitation, LV mass index, LVEDDI, and LVESDI). In a multivariate model that included these variables, the strongest predictor of reverse remodeling was the baseline LVESDI ( Table 3 ). Other independent predictors of reverse remodeling were female gender and the presence of nonischemic cardiomyopathy. Although the QRS duration was increased in patients in the −RR group, it was not a strong predictor of reverse remodeling (109 ± 30 ms vs 113 ± 30 ms; odds ratio 1.01; 95% confidence interval 1.00 to 1.02; p = 0.003). Similarly, the baseline systolic blood pressure was not a strong predictor of reverse remodeling (odds ratio 0.99; 95% confidence interval 0.98 to 1.00; p = 0.03). Although the initial LVEF was slightly greater in patients in the +RR group, it was not an independent predictor of reverse remodeling.



