Frequent supraventricular extrasystoles (SVEs) are associated with the subsequent first-time appearance of atrial fibrillation (AF) and ischemic stroke. The aim of this study was to investigate the combined role of SVEs and an AF-related risk score for ischemic stroke, the CHADS 2 score, on the occurrence of new AF in patients in sinus rhythm. The Shinken Database 2004–2010 lists 3,263 patients who underwent 24-hour Holter monitoring. A total of 2,589 patients were analyzed, after excluding 674 patients previously diagnosed with AF. Frequent SVEs were defined as ≥102 beats/day (the top quartile) and the presence of a clinical background for a CHADS 2 score ≥2 points as a high CHADS 2 score. During the mean follow-up period of 571.4 ± 606.4 days, new AF occurred in 38 patients (9.4 per 1,000 patient-years). The incidence of new AF was 2.7 and 37.7 per 1,000 patient-years for patients with nonfrequent SVEs (<102 beats/day) and low CHADS 2 scores and those with frequent SVEs and high CHADS 2 scores, respectively. Multivariate Cox regression analysis showed that the hazard ratio for frequent SVEs and a high CHADS 2 score compared with nonfrequent SVEs and a low CHADS 2 score was 9.49 (95% confidence interval 3.20 to 28.15, p <0.001), even after adjustment for gender, age, medications, and echocardiographic parameters. In conclusion, frequent SVEs and a high CHADS 2 score independently and synergistically predict the first-time appearance of AF in patients in sinus rhythm, indicating an approximately 10-fold higher risk. Patients meeting these criteria should have more aggressive early intervention for preventing AF.
Several recent reports have indicated that frequent supraventricular extrasystoles (SVEs) can predict the subsequent first-time appearance of atrial fibrillation (AF) and ischemic stroke in healthy subjects and symptomatic patients, independent of the patients’ backgrounds. The relation between SVEs and AF is attributed, at least in part, to a common origin (possibly the pulmonary veins) or by confounding clinical factors (age, hypertension, or cardiovascular diseases). However, it is unclear why SVEs are associated with the future incidence of ischemic stroke. Currently, the CHADS 2 score is widely used for predicting the future incidence of ischemic stroke in patients with AF. In this respect, a high CHADS 2 score might be applicable even in patients in sinus rhythm, especially those at high risk for AF development. This is because whenever such patients subsequently develop new AF, they would be at high risk for ischemic stroke. Although AF is more prevalent in subjects with high CHADS 2 scores than in those with low CHADS 2 scores, the combined role of SVEs and the CHADS 2 score on new AF development in patients in sinus rhythm remains unclear. Therefore, in the present study, we investigated the combined role of SVEs and the CHADS 2 score on new AF development in patients in sinus rhythm.
Methods
The Shinken Database contains data on all new patients visiting the Cardiovascular Institute Hospital in Tokyo, Japan (Shinken is an abbreviated name in Japanese for the name of the hospital); those with active cancer and foreign travelers are excluded. The principal aim of establishing this hospital-based database is surveillance of the prevalence and prognosis of cardiovascular diseases in the urban areas of Japan. The registry has been maintaining annual records of patient data since June 2004. Data on health status and the incidence of cardiovascular events and mortality are maintained in the database by linking to the medical records of the hospital and collecting data from mail sent to the patients approximately once or twice a year. Details on this procedure have been published elsewhere.
The data in the present study were derived from records maintained for the period from June 2004 to March 2011 (Shinken Database 2004–2010) for 15,227 new visiting patients. The database contains Holter recordings of 3,263 patients obtained at the first visit to our hospital. After excluding 674 patients with preexisting AF or AF on Holter recordings, we included 2,589 patients as the study population of the present analysis. The ethics committee at the Cardiovascular Institute approved the study protocol, and all patients provided written informed consent.
All 24-hour electrocardiographic recordings were reviewed and edited manually. Recordings had to exceed 23 hours and be of good quality to be analyzed by trained personnel. The number of SVEs in the top quartile (SVEs ≥102 beats/day) was classified as frequent. The first-time appearance of AF was determined by electrocardiograms recorded during visits to the outpatient clinic and inpatient stay at our hospital until March 31, 2012.
Analyses were performed as follows. First, crude incidence rates of the first-time appearance of AF stratified by quartiles of SVEs and CHADS 2 scores were determined, and the differences between categories were tested using Cochran-Armitage trend tests. Second, the study population was classified into 2 categories, which were then further subdivided: (1) frequent SVEs (≥102 beats/day) and nonfrequent SVEs (<102 beats/day), and (2) high CHADS 2 score (≥2 points) and low CHADS 2 score (<2 points). Differences in the cumulative incidence rates of the first-time appearance of AF were then estimated using the Kaplan-Meier method and tested using log-rank tests. Finally, Cox regression analysis was performed by testing the nonadjusted and adjusted models for the synergistic effects of frequent SVEs and high CHADS 2 score. In the adjusted model, the effect of frequent SVEs and a high CHADS 2 score was adjusted by age, gender, medications, and echocardiographic parameters, including left atrial dimension and the left ventricular ejection fraction.
For baseline characteristics, the differences in consecutive and categorical variables were tested using unpaired Student’s t tests and chi-square tests, respectively. All analyses were performed using SPSS version 19.0 for Windows (SPSS, Inc., Chicago, Illinois). Statistical significance was set at p <0.05.
Results
Table 1 lists the baseline clinical characteristics of the study population. A total of 2,589 patients were recruited for this study. The average number of SVEs was 696.8 ± 3,401.7 beats/day, and the median number of SVEs was 24 beats/day (range 0 to 63,381, interquartile range 8 to 102). The top quartile (SVEs ≥102 beats/day) included 647 patients (25.0%) who were considered to have frequent SVEs. The population included 230 patients (8.9%) with CHADS 2 scores ≥2 points (note that patients did not have AF but were evaluated using an AF-related score), which were considered high scores in this study.
| Variable | Value |
|---|---|
| Age (yrs) | 54.2 ± 15.5 |
| Age ≥75 yrs | 219 (8.5%) |
| Men | 1,436 (55.5%) |
| Heart failure | 152 (5.9%) |
| Valvular heart disease | 105 (4.1%) |
| Coronary heart disease | 205 (7.9%) |
| Dilated cardiomyopathy | 30 (1.2%) |
| Hypertrophic cardiomyopathy | 42 (1.6%) |
| Left ventricular noncompaction | 20 (0.8%) |
| Hypertension | 752 (29.0%) |
| Diabetes mellitus | 200 (7.7%) |
| Cigarette smoker | 845 (32.6%) |
| Current alcohol intake | 1,810 (69.9%) |
| Chronic kidney disease | 278 (10.7%) |
| Cerebral infarction or transient ischemic attack | 25 (1.0%) |
| CHADS 2 score | |
| 0 | 1,655 (63.9%) |
| 1 | 704 (27.2%) |
| 2 | 184 (7.1%) |
| 3 | 36 (1.4%) |
| 4 | 9 (0.3%) |
| 5 | 1 (0.0%) |
| 6 | 0 (0.0%) |
| ≥2 | 230 (8.9%) |
| CHA 2 DS 2 -VASc score | |
| 0 | 776 (30.0%) |
| 1 | 1,014 (39.2%) |
| 2 | 438 (16.9%) |
| 3 | 234 (9.0%) |
| 4 | 93 (3.6%) |
| 5 | 31 (1.2%) |
| 6 | 2 (0.1%) |
| 7 | 1 (0.0%) |
| Left atrial dimension (mm) | 33.9 ± 6.0 |
| Left ventricular ejection fraction (%) | 66.0 ± 9.2 |
| Palpitation or chest discomfort | 1,437 (55.5%) |
| Dizziness, faintness, or syncope | 137 (5.3%) |
| Others | 1,073 (41.4%) |
| Calcium channel blockers | 352 (13.6%) |
| β blockers | 218 (8.4%) |
| Angiotensin-converting enzyme inhibitors | 68 (2.6%) |
| Angiotensin receptor blockers | 344 (13.3%) |
| Anticoagulants | 56 (2.2%) |
| Antiplatelet medications | 354 (13.7%) |
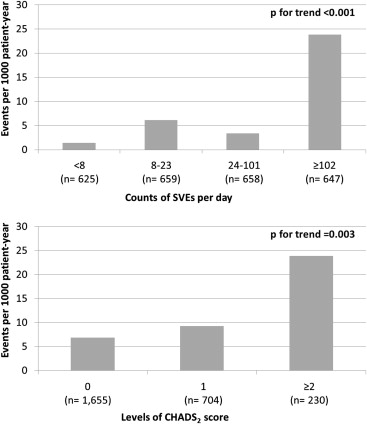
During the mean follow-up period of 571.4 ± 606.4 days, new AF occurred in 38 patients (9.4 per 1,000 patient-years). Figure 1 shows the incidence of new AF in relation to the number of SVEs and CHADS 2 scores. The incidence of new AF was 1.4 per 1,000 patient-years for patients with SVEs <8 beats/day and 6.1 and 3.4 per 1,000 patient-years for patients with SVEs of 8 to 23 and 24 to 101 beats/day, respectively. This incidence was markedly high at 23.8 per 1,000 patient-years for patients with SVEs ≥102 beats/day (the top quartile, p <0.001). Similarly, the incidence of new AF increased from 6.9 to 9.3 and 23.9 per 1,000 patient-years in patients with CHADS 2 scores of 0, 1, and ≥2, respectively (p = 0.003).
Patients were classified into 2 categories: frequent and nonfrequent SVEs and high and low CHADS 2 scores. Their clinical characteristics are listed in Tables 2 and 3 . Kaplan-Meier curves showed that frequent SVEs were more closely associated with a higher incidence rate of new AF than nonfrequent SVEs (p <0.001; Figure 2 ). Similarly, a high CHADS 2 score was associated with a higher incidence rate of new AF than a low CHADS 2 score (p = 0.001; Figure 2 ).
| Variable | SVEs (beats/day) | p Value | |
|---|---|---|---|
| ≥102 (n = 647) | <102 (n = 1,942) | ||
| Age (yrs) | 63.7 ± 13.3 | 51.0 ± 14.8 | <0.001 |
| Age ≥75 yrs | 132 (20.4%) | 87 (4.5%) | <0.001 |
| Men | 316 (48.8%) | 1,120 (57.7%) | <0.001 |
| Heart failure | 46 (7.1%) | 106 (5.5%) | 0.123 |
| Valvular heart disease | 53 (8.2%) | 52 (2.7%) | <0.001 |
| Coronary heart disease | 50 (7.7%) | 155 (8.0%) | 0.867 |
| Dilated cardiomyopathy | 5 (0.8%) | 25 (1.3%) | 0.396 |
| Hypertrophic cardiomyopathy | 16 (2.5%) | 26 (1.3%) | 0.070 |
| Left ventricular noncompaction | 4 (0.6%) | 16 (0.8%) | 0.797 |
| Hypertension | 258 (39.9%) | 494 (25.4%) | <0.001 |
| Diabetes mellitus | 60 (9.3%) | 140 (7.2%) | 0.090 |
| Cigarette smoker | 197 (30.4%) | 648 (33.4%) | 0.176 |
| Current alcohol intake | 422 (65.2%) | 1,388 (71.5%) | 0.003 |
| Chronic kidney disease | 112 (17.3%) | 166 (8.5%) | <0.001 |
| Cerebral infarction or transient ischemic attack | 10 (1.5%) | 15 (0.8%) | 0.102 |
| CHADS 2 score | |||
| 0 | 309 (47.8%) | 1,346 (69.3%) | <0.001 |
| 1 | 237 (36.6%) | 467 (24.0%) | |
| 2 | 77 (11.9%) | 107 (5.5%) | |
| 3 | 18 (2.8%) | 18 (0.9%) | |
| 4 | 5 (0.8%) | 4 (0.2%) | |
| 5 | 1 (0.2%) | 0 (0.0%) | |
| 6 | 0 (0.0%) | 0 (0.0%) | |
| ≥2 | 101 (15.6%) | 129 (6.6%) | <0.001 |
| Left atrial dimension (mm) | 35.4 ± 6.7 | 33.4 ± 5.7 | <0.001 |
| Left ventricular ejection fraction (%) | 66.5 ± 9.7 | 65.8 ± 9.1 | 0.14 |
| Calcium channel blockers | 124 (19.2%) | 228 (11.7%) | <0.001 |
| β blockers | 66 (10.2%) | 152 (7.8%) | 0.072 |
| Angiotensin-converting enzyme inhibitors | 18 (2.8%) | 50 (2.6%) | 0.777 |
| Angiotensin receptor blockers | 109 (16.8%) | 235 (12.1%) | 0.003 |
| Anticoagulants | 26 (4.0%) | 30 (1.5%) | <0.001 |
| Antiplatelet medications | 121 (18.7%) | 233 (12.0%) | <0.001 |
| Variable | CHADS 2 Score | p Value | |
|---|---|---|---|
| ≥2 (n = 231) | <2 (n = 2,361) | ||
| Age (yrs) | 71.8 ± 10.4 | 52.4 ± 14.8 | <0.001 |
| Age ≥75 yrs | 137 (59.3%) | 83 (3.5%) | <0.001 |
| Men | 127 (55.0%) | 1,311 (55.5%) | 0.890 |
| Heart failure | 34 (14.7%) | 119 (5.0%) | <0.001 |
| Valvular heart disease | 9 (3.9%) | 96 (4.1%) | 1.000 |
| Coronary heart disease | 47 (20.3%) | 160 (6.8%) | <0.001 |
| Dilated cardiomyopathy | 2 (0.9%) | 28 (1.2%) | 1.000 |
| Hypertrophic cardiomyopathy | 4 (1.7%) | 38 (1.6%) | 0.785 |
| Left ventricular noncompaction | 0 (0.0%) | 20 (0.8%) | 0.249 |
| Hypertension | 212 (91.8%) | 541 (22.9%) | <0.001 |
| Diabetes mellitus | 121 (52.4%) | 81 (3.4%) | <0.001 |
| Cigarette smoker | 83 (35.9%) | 763 (32.3%) | 0.271 |
| Current alcohol intake | 127 (55.2%) | 1,683 (71.3%) | <0.001 |
| Chronic kidney disease | 70 (30.3%) | 209 (8.9%) | <0.001 |
| Cerebral infarction or transient ischemic attack | 25 (10.8%) | 0 (0.0%) | <0.001 |
| Number of SVEs | <0.001 | ||
| <8 | 20 (8.7%) | 605 (25.6%) | |
| 8–23 | 43 (18.6%) | 617 (26.1%) | |
| 24–101 | 66 (28.6%) | 593 (25.1%) | |
| ≥102 | 102 (44.2%) | 546 (23.1%) | |
| Left atrial size (mm) | 37.7 ± 5.8 | 33.6 ± 5.9 | <0.001 |
| Left ventricular ejection fraction (%) | 66.8 ± 11.8 | 65.9 ± 9.0 | 0.254 |
| Calcium channel blockers | 102 (44.2%) | 250 (10.6%) | <0.001 |
| β blockers | 47 (20.3%) | 173 (7.3%) | <0.001 |
| Angiotensin-converting enzyme inhibitors | 23 (10.0%) | 45 (1.9%) | <0.001 |
| Angiotensin receptor blockers | 84 (36.4%) | 260 (11.0%) | <0.001 |
| Anticoagulants | 11 (4.8%) | 47 (2.0%) | 0.016 |
| Antiplatelet medications | 92 (39.8%) | 263 (11.1%) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


