Protocols to minimize the time between 2 measurements of troponin or a combination with copeptin have been developed to rapidly rule-in or rule-out myocardial injury (MI) in patients with chest pain. These fast track protocols to rule-in and rule-out MI are not sufficiently validated for early chest pain presenters. The “early presenter” model was tested in 107 stable patients after a short period of myocardial ischemia, induced by stenting of a significant coronary artery stenosis. High-sensitivity troponin T (hsTnT), high-sensitivity troponin I (hsTnI), and copeptin were measured at the start and 90, 180, and 360 minutes after stent implantation. MI was defined as a troponin level more than the upper limit of normal (ULN) and an absolute increase of >50% ULN on the 360-minute sample. A single combined measurement of troponin and copeptin 90 minutes after the onset of ischemia has a low diagnostic value. This increases when serial measurements with 90-minute intervals are included. For ruling in MI, the highest positive predictive value (with a 95% confidence interval [CI]) can be obtained when focusing only on the increase in troponin level, with a positive predictive value of 86% (70, 93) and 80% (67, 90) for hsTnT and hsTnI, respectively. For ruling out MI, a combined absence of any troponin more than the ULN and any significant increase in troponin level perform best with a negative predictive value of 75% (55, 89) and 75% (55, 89) for hsTnT and hsTnI, respectively. In conclusion, in early presenters, rapid biomarker protocols underestimate MI. A standard biomarker assessment after 3 hours is required to adequately rule-in or rule-out myonecrosis.
Since the development of more sensitive assays for cardiac troponins, myocardial injury (MI) can be detected earlier. Recent studies have tested biomarker protocols with a very short delay (e.g., 1 hour) or with a single measurement of troponin and copeptin to rule-in or to rule-out MI in a population with chest pain. Although these newer protocols appear to be promising, early presenters (chest pain for <2 hours) are under-reported. In the Chopin trial with copeptin, a marker of acute endogenous stress, early presenters, defined as patients with chest pain for <3 hours from onset, constituted 75% of the patient sample. In this trial, a detailed evaluation of the effect of time delay on diagnosis was lacking, especially for the very early presenters (<2 hours). Furthermore, a subgroup analysis of the study by Rubini Gimenez et al showed that high-sensitivity troponin values at admission were more frequently below the upper limit of normal (ULN) in early presenters compared with patients admitted >3 hours after pain onset. This may reduce accuracy when short biomarker protocols are used. Therefore, improved knowledge of the diagnostic performance of these new protocols in patients presenting early after onset of chest pain is a prerequisite to the application and validation of these biomarker protocols in a general population of patients with chest pain.
Methods
The “early presenter” model was tested in 107 consecutive stable patients in whom a short period of myocardial ischemia was induced during a percutaneous coronary intervention (PCI) of a significant coronary artery stenosis. The time between the onset of pain/ischemia and the first biomarker evaluation was fixed at 90 minutes, and a subsequent biomarker measurement was taken 90 minutes after this first biomarker assessment. Exclusion criteria included a recent myocardial infarction (<1 week), a left ventricular ejection fraction <40%, a serum creatinine >2 mg/dl, and hemodynamic unstable patients. All patients provided written informed consent, and the study was approved by the ethics committee of the institution. Patient data were prospectively collected: age, gender, body mass index, and coronary risk factors. Concomitant medication use was recorded. Laboratory analysis before the intervention included serum creatinine levels and a lipid profile. During the PCI, we determined the number of vessels treated, the severity of the coronary artery stenosis, the Thrombolysis in Myocardial Infarction (TIMI) flow before and after the intervention, the length and nature of the coronary stent implanted, and balloon inflation pressure and time. The lengths of the coronary lesions and stents implanted were expressed as total length, consisting of a summation of the individual lesions/stents.
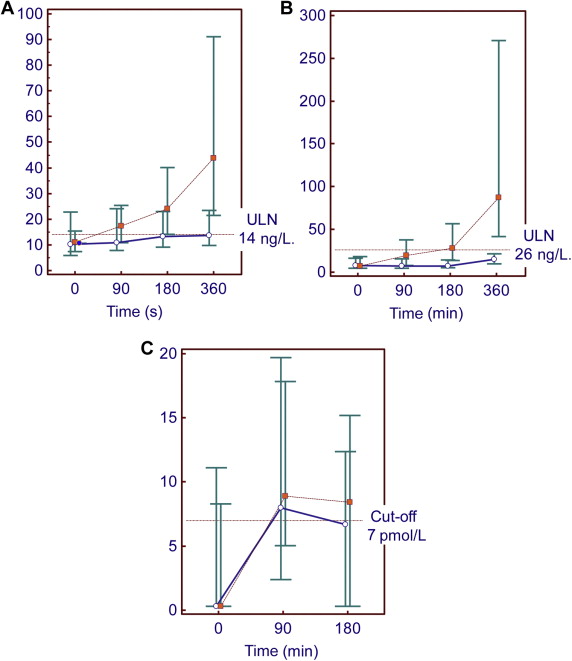
Blood samples were taken at the start of the PCI and 90, 180, and 360 minutes after first stent implantation. Both serum and EDTA plasma were stored at −80°C. High-sensitivity troponin T (hsTnT) in serum and high-sensitivity troponin I (hsTnI) in EDTA were measured with Modular E170 (Roche Diagnostics, Vilvoorde, Belgium) and Architect i1000SR (Abbott Diagnostics, Wavre, Belgium) instruments, respectively. Copeptin in serum was measured on a Kryptor (B.R.A.H.M.S.; Thermofisher Scientific, Henningsdorf, Germany) instrument. MI was defined for each high-sensitivity troponin assay separately as a troponin level more than the ULN at 6 hours and an absolute increase of >50% ULN of troponin in the 360-minute blood sample versus the first measurement at the start. For hsTnT and hsTnI, the ULN was 14 and 26 ng/L, respectively. Additionally, copeptin was analyzed at the beginning and 90 and 180 minutes after first stent implantation.
Variables are expressed as the median and the 25th and 75th percentiles. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for detecting MI, with their 95% confidence intervals (CI), were calculated. Receiver operating characteristic curves were used to identify the optimal cut-off points for copeptin and troponin increases. A net reclassification index (NRI) was calculated as measure of the incremental prognostic impact of a new biomarker when added to an existing prediction model for a binary outcome. A p value <0.05 was considered statistically significant. Sample size was calculated based on an anticipated MI prevalence of 33%. We required 103 patients to estimate a sensitivity of 0.90 with a precision of 0.1 and at a confidence level of 95%. With this sample size, a specificity of 0.75 can be estimated with a precision of 0.1. Analyses were performed with MedCalc, version 13 (MedCalc Software bvba, Ostend, Belgium).
Results
A total of 107 patients with a planned PCI were enrolled. Table 1 describes the patient characteristics and procedure-related details. Most patients had a TIMI 3 flow before the percutaneous procedure; there was a TIMI 2 flow in 1 patient and a TIMI 1 flow in 8 patients. The PCI was complicated by 5 dissections of the coronary artery and 1 perforation, which were adequately covered by stents. In 1 patient, there was temporarily no reflow phenomenon during the procedure, and 1 patient showed occlusion of a side branch. After treatment, all treated vessels showed a TIMI 3 flow. In 2 patients, a rotablator was used before implanting the stent.
| Variable | |
|---|---|
| Age (years) | 70 (54, 79) |
| Men | 78% |
| Coronary risk factors | |
| Hypertension | 74% |
| Smokers | 64% |
| Diabetes mellitus | 26% |
| Hypercholesterolemia | 74% |
| Total cholesterol (mg/dl) | 179 (147, 216) |
| LDL cholesterol (mg/dl) | 103 (78, 126) |
| Statin therapy | 79% |
| Body Mass Index (kg/m 2 ) | 26.2 (24.4-28.5) |
| Invasive procedure data | |
| Total inflation time (seconds) | 26 (14, 45) |
| Inflation pressure (atmosphere) | 20 (16, 20) |
| >1 coronary artery treated | 23% |
| Total length lesions treated (mm) | 18 (12, 27) |
| Number of stents used | 1 (1, 2) |
| Diameter stenosis before PCI (%) | 76 (63, 86) |
| Diameter stenosis after PCI (%) | 7 (0, 13) |
MI, as defined on the 360-minute sample for hsTnT and hsTnI separately, was present in 56% (46 to 66) of the total population for hsTnT and 62% (51 to 72) for hsTnI. For hsTnT, we could evaluate all 107 patients. For hsTnI, only 90 patients were fully documented. Biomarkers were sampled at the start of the PCI procedure (baseline), 90 minutes (90, 90), 180 minutes (180, 180), and 395 minutes (369, 430) after the first stent implantation. Figure 1 shows the evolution of the different biomarkers after stratification for the presence or absence of MI.
Tables 2 and 3 describes the diagnostic value of various protocols to rule-in or rule-out MI. For ruling in MI, a single measurement of high-sensitivity troponin underestimates the presence of MI in the early presenters, with a positive predictive value of 66% (51, 78) and 79% (59, 92) for hsTnT and hsTnI, respectively. The negative predictive value for ruling out MI is very low for both high-sensitivity troponin assays: 54% and 47%, respectively.
| Sensitivity % (CI) | Specificity % (CI) | PPV % (CI) | NPV % (CI) | NRI % | |
|---|---|---|---|---|---|
| Single/combined measurement | |||||
| High-sensitivity TnT >ULN | |||||
| 90 min after onset of ischemia | 63 (49, 76) | 57 (41, 72) | 66 (51, 78) | 54 (39, 69) | |
| hsTnT >ULN, copeptin >7 pmol/l | |||||
| 90 min after onset of ischemia | 84 (72, 93) | 34 (20, 50) | 62 (51, 73) | 63 (41, 81) | -2* |
| Serial troponin measurement | |||||
| hsTnT rise >1.73 ng/l | |||||
| Troponin rise in 90 min | 75 (62-86) | 84 (71-94) | 86 (70-93) | 73 (58-84) | 39** |
| hsTnT >ULN, hsTnT rise >1.73 ng/l | |||||
| Troponin rise in 90 min | 88 (76-95) | 48 (32-63) | 68 (57-79) | 75 (55-89) | 16** |
| Sensitivity % (CI) | Specificity % (CI) | PPV % (CI) | NPV % (CI) | NRI % | |
|---|---|---|---|---|---|
| Single/combined measurement | |||||
| High sensitivity TnI >ULN | |||||
| 90 min after onset of ischemia | 40 (27,54) | 82 (66, 93) | 79 (59, 92) | 47 (34, 60) | |
| hsTnI >ULN , copeptin >7pmol/l | |||||
| 90 min after onset of ischemia | 81 (69,91) | 49 (31, 66) | 71 (59, 82) | 63 (42, 81) | 8* |
| Serial troponin measurement | |||||
| hsTnI rise >1.3 ng/l | |||||
| Troponin rise in 90 min | 77 (64-880) | 70 (51-84) | 80 (67-90) | 66 (48-81) | 25** |
| hsTnI>ULN , hsTnI rise 1.3 ng/l | |||||
| Troponin rise in 90 min | 87 (75-95) | 64 (45-80) | 79 (67-89) | 75 (55-89) | 29** |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


