The accuracy of 64-slice computed tomographic coronary angiography (CTA) and its ability to direct revascularization in patients with acute chest pain syndrome (ACPS) was investigated. A total of 107 patients with ACPS presenting to the emergency department and referred to cardiology were prospectively enrolled and underwent CTA. From the clinical features, the patients were categorized as having high-risk acute coronary syndrome features or no high-risk features. At the treating physician’s discretion, the patients underwent risk stratification with either invasive coronary angiography (ICA) or technetium-99m single photon emission computed tomography. All tests were interpreted by experts unaware of the clinical information. All 52 patients with high-risk acute coronary syndrome features underwent ICA. Of the 55 patients with no high-risk features, 36 underwent single photon emission computed tomography and 19 underwent ICA. The patients were followed up until a decision regarding revascularization was made. Compared with ICA, the operating characteristics of CTA (per-patient analysis) were excellent, with a sensitivity of 98% (95% confidence interval [CI] 87% to 100%), specificity of 100% (95% CI 85% to 100%), positive predictive value of 100% (95% CI 90% to 100%), and negative predictive value of 97% (95% CI 80% to 100%). The agreement between CTA and routine testing (single photon emission computed tomography or ICA) was very good (κ = 0.94). CTA correctly identified 40 patients (100%) who underwent revascularization and 61 (91.0%) who were treated medically (κ = 0.88, 95% CI 0.79 to 0.97). In conclusion, CTA might represent a single modality that could be used to triage a wide spectrum of patients with ACPS and could have the potential to rule out coronary disease and identify those who might require revascularization.
Computed tomographic coronary angiography (CTA) is an emerging diagnostic tool for the detection of coronary artery disease (CAD) in patients with stable symptoms. However, mounting data supports the use of CTA for both stable patients and those presenting to the emergency department with acute chest pain syndromes (ACPS). The high sensitivity and negative predictive value of CTA enables it to rule out obstructive CAD and potentially eliminate the need for hospital admission or additional cardiac testing. Similarly, if proved to be accurate in patients with obstructive CAD, CTA might have a role in directing patient treatment. The present study prospectively assessed the potential accuracy of CTA in a wide spectrum of patients with ACPS compared to routine testing and CTA’s ability to direct patient revascularization therapy.
Methods
From October 2006 to June 2008, nonconsecutive patients presenting to the emergency department with ACPS and referred to cardiology for cardiac investigations or follow-up were prospectively enrolled and categorized as (1) having high-risk acute coronary syndrome features (HR-ACS) or (2) without high-risk features (i.e., low- or intermediate-risk patients). HR-ACS was defined as an accelerating pattern or a prolonged episode (>20 minutes) or recurrent episodes of chest pain at rest or with minimal effort within the preceding 24 hours and an elevated troponin or electrocardiographic changes consistent with ischemia (ST-segment depression of ≥0.1 mV or transient [<20 minutes] ST-segment elevation of ≥0.1 mV).
Patients were excluded because of age <18 years, an allergy or contraindication to contrast agents, refractory angina requiring urgent/emergent invasive coronary angiography (ICA), pregnancy, a history of coronary revascularization, atrial fibrillation, frequent ectopy, an uncontrolled heart rate, or the inability to perform a 20-second breath hold.
All patients with HR-ACS were treated with an invasive strategy and underwent ICA. The patients without high-risk features underwent examination at the discretion of the treating physician and were either referred for ICA or technetium-99m single photon emission computed tomographic myocardial perfusion imaging. CTA for the present study was performed before all ICA. For patients undergoing single photon emission computed tomography, the timing of CTA was determined by test availability. All patients provided informed consent, and the institutional human research ethics board approved the protocol.
The medical history and laboratory test results were recorded for all patients.
Using the National Cholesterol Education Program/Adult Treatment Panel III guidelines, the cardiac risk factors were collected. Hypertension was defined as blood pressure >140/90 mm Hg or if the patient was taking antihypertensive medication. The diagnosis of dyslipidemia was determined by the fasting lipid profile results or drug treatment of hyperlipidemia. Before image acquisition, the patients received metoprolol, targeting a heart rate of ≤65 beats/min, and nitroglycerin 0.8 mg sublingually. A biphasic timing bolus (Visipaque 320 or Omnipaque 350, GE Healthcare, Princeton, New Jersey) was used to calculate the transit time. Final images were acquired using a triphasic protocol (100% contrast, 40%/60% contrast/saline, and 40 ml saline). The contrast volume and infusion rate (5 to 8 ml/s) were individualized according to the scan time and patient body habitus.
Retrospective electrocardiographic-gated data sets were acquired using the GE volume computed tomographic scanner (GE Healthcare, Milwaukee, Wisconsin) at 64 × 0.625 mm slice collimation, a gantry rotation of 350 ms (300 to 800 mA, 120 kVp), with electrocardiographic-gated tube modulation and a pitch (0.16 to 0.24) that was individualized to the patient’s heart rate. The computed tomographic data sets were reconstructed with a slice thickness of 0.625 mm (0.4 mm increment) using the cardiac phases with the least cardiac motion.
The images were postprocessed using the GE Advantage Volume Share Workstation (GE Healthcare) and visually interpreted by an expert observer unaware of the clinical data. A 17-segment model of the coronary arteries and a 4-point grading score (normal, mild [<50%], moderate [50% to 69%], and severe [≥70%]) were used to evaluate coronary stenosis. Using the computed tomographic angiographic coronary anatomy, lesion characteristics, and target vessels, the patients were allocated to a revascularization strategy (medical therapy, percutaneous coronary intervention, or coronary artery bypass grafting). Significant obstructive CAD was defined as ≥70% luminal diameter stenosis or ≥50% left main stenosis. High-risk CAD was defined as left main stenosis of ≥50%, triple vessel CAD of ≥70%, or 2-vessel disease (≥70%) with one vessel the proximal left anterior descending artery.
ICA was performed according to the clinical routine. Using the same grading system as for CTA, all invasive coronary angiograms were reviewed by 2 observers unaware of the clinical data or computed tomographic angiographic results.
Recognizing that the decision for revascularization is often influenced by clinical information, the blinded ICA observers allocated patients to a “theoretical” revascularization strategy according to the findings from ICA (anatomy) alone (medical therapy, percutaneous coronary intervention, or coronary artery bypass surgery). Nonobstructive CAD on ICA was allocated to medical therapy and obstructive CAD was allocated to a revascularization strategy. Patients with high-risk coronary anatomy were allocated to coronary artery bypass grafting.
Technetium-99m (tetrofosmin) single photon emission computed tomographic myocardial perfusion imaging was performed according to the clinical routine. In brief, a 1-day rest–stress protocol was used. Patients unable to exercise underwent vasodilator stress (dipyridamole 0.142 mg/kg/min for 5 minutes). Image acquisition was performed on dual-headed cameras using low-energy, high-resolution collimators and a 15% energy window centered on the 140-keV photopeak. Electrocardiographic-gated single photon emission computed tomographic data were acquired for 180° (25 s/projection for 60 projections) and reconstructed with filtered back-projection using a 64 × 64 matrix.
All single photon emission computed tomographic images were reviewed by 2 observers unaware of the clinical data and computed tomographic angiographic results. The findings were considered abnormal in the presence of perfusion abnormalities not attributable to attenuation artifact, the presence of transient ischemic dilation, or the presence of increased lung uptake.
To determine the accuracy of the CAD diagnosis, CTA was compared with routine testing (ICA or single photon emission computed tomography).
The need for ICA after single photon emission computed tomography and all treatment decisions (medical therapy or revascularization) after single photon emission computed tomography and ICA were left to the discretion of the physician who was unaware of the computed tomographic angiographic results. All patients were followed up until a clinical decision regarding therapy or revascularization had been made, and all revascularization decisions were made without knowledge of the results from CTA.
Along with the “actual” (clinical) revascularization decision, the patients were allocated to a “theoretical” revascularization strategy according the findings from ICA (anatomy) alone without clinical data. Patients with high-risk CAD and suitable distal target vessels were allocated to coronary artery bypass grafting. Patients with high-risk CAD but not amenable to complete revascularization with coronary artery bypass grafting and patients with nonhigh-risk CAD with suitable target lesions were allocated to percutaneous coronary intervention. Patients without obstructive CAD and patients with CAD not amenable to revascularization were allocated to medical therapy.
Statistical analyses were performed using Statistical Analysis Systems, version 9.1.3 (SAS Institute, Cary, North Carolina). Continuous outcomes are presented as the mean ± SD and categorical outcomes as frequencies with percentages. Agreements between categorical variables were assessed using κ analysis.
Results
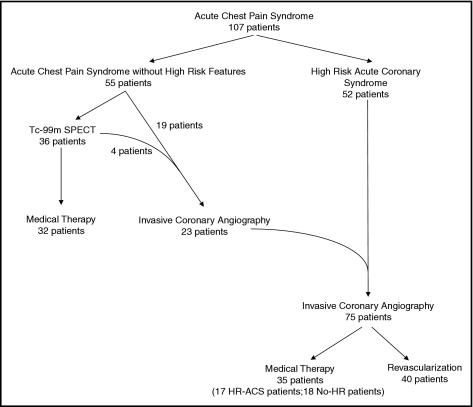
A total of 108 patients were prospectively enrolled, but 1 patient did not undergo CTA because of a heart rate >65 beats/min. The final study included 107 patients (52 HR-ACS and 55 without high-risk features; Table 1 ). All 52 patients with HR-ACS underwent ICA. Of the 55 patients without high-risk features, 36 underwent technetium-99m single photon emission computed tomography and 19 underwent ICA. During the study period, 4 patients initially evaluated using technetium-99m single photon emission computed tomography subsequently underwent ICA. Thus, 23 (42%) of the 55 patients without high-risk features in the present study underwent ICA ( Figure 1 ).
| Variable | All Patients (n = 107) | HR-ACS (n = 52) | No-HR (n = 55) |
|---|---|---|---|
| Age (years) | 54 ± 10 | 55 ± 10 | 53 ± 9 |
| Men | 73 (68%) | 41 (79%) | 32 (58%) |
| Thrombolysis In Myocardial Infarction score ⁎ | |||
| Median | 1 | 2 | 0 |
| Range | 0–2 | 1–3 | 0–1 |
| Global Registry of Acute Cardiac Events score ⁎ | |||
| Median | 99 | 112 | 78 |
| Range | 75–112 | 100–128 | 67–96 |
| Creatinine (μmol/L) | 85 ± 50 | 91 ± 71 | 78 ± 14 |
| Diabetes mellitus | 11 (10%) | 6 (12%) | 5 (9%) |
| Current smoker | 31 (29%) | 19 (37%) | 12 (22%) |
| Dyslipidemia | 53 (50%) | 25 (48%) | 28 (51%) |
| Hypertension | 46 (43%) | 18 (35%) | 28 (51%) |
| Previous coronary artery disease | 9 (8%) | 9 (17%) | 0 (0%) |
| Abnormal troponin level | 49 (47%) † | 46 (89%) | 3 (6%) † |
| Imaging heart rate (beats/min) | 56 ± 6 | 58 ± 6 | 55 ± 5 |
| Radiation dose (mSv) | 15 ± 3 | 15 ± 3 | 15 ± 3 |
⁎ Three patients were excluded because of insufficient information.
† Troponin values were not recorded in 2 patients in no high-risk features group.
A total of 75 patients underwent ICA (52 HR-ACS and 23 without high-risk features). The operating characteristics of CTA for the detection of anatomic obstructive CAD (left main diameter stenosis of ≥50% or ≥70% in any other vessel), with a per-patient analysis, were excellent ( Table 2 ). CTA was similarly accurate in the HR-ACS population ( Table 2 ).
| Variable | Patients (n) | True Positive | True Negative | False Positive | False Negative | κ | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|---|---|---|---|---|---|---|
| All patients ⁎ | 107 | 46 | 59 | 0 | 2 | 0.96 |
|
|
|
|
| Patients undergoing coronary angiography | 75 | 46 | 29 | 0 | 0 | 1.00 |
|
|
|
|
| Patients with high-risk acute coronary syndrome † | 52 | 35 | 17 | 0 | 0 | 1.00 |
|
|
|
|
Examining an anatomic threshold of ≥50% diameter stenosis in any vessel, the operating characteristics of CTA compared to ICA, in a per-patient analysis, were equally excellent ( Table 3 ).
| Variable | Patients (n) | True Positive | True Negative | False Positive | False Negative | κ | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|---|---|---|---|---|---|---|
| All patients ⁎ | 107 | 47 | 51 | 6 | 3 | 0.83 |
|
|
|
|
| Patients undergoing coronary angiography | 75 | 47 | 23 | 4 | 1 | 0.85 |
|
|
|
|
| Patients with high-risk acute coronary syndrome † | 52 | 35 | 13 | 3 | 1 | 0.81 |
|
|
|
|
Using a vessel-based analysis (left main artery of ≥50% and left anterior, circumflex, and right coronary arteries of ≥70%), CTA demonstrated very good operating characteristics in the 75 patients who had undergone ICA (sensitivity of 89%, 95% confidence interval [CI] 80% to 95%), specificity of 94% (95% CI 90% to 97%), positive predictive value of 83% (95% CI 73% to 91%), and negative predictive value of 96% (95% CI 93% to 98%). Using a vessel-based analysis and a threshold of ≥50% for obstructive CAD, the sensitivity, specificity, positive predictive value, and negative predictive value for CTA was 92% (95% CI 83% to 96%), 87% (95% CI 82% to 91%), 75% (95% CI 65% to 82%), and 96% (95% CI 92% to 98%), respectively.
The accuracy of CTA in all 107 patients and the agreement between CTA and “routine testing” for the diagnosis of CAD were very good (κ = 0.94).
Of the 36 patients who underwent single photon emission computed tomography, myocardial perfusion was normal in all but 1 patient, yet 4 patients were referred for ICA. All 4 patients (3 of whom had normal myocardial perfusion) had severe CAD requiring revascularization ( Figure 1 ).
At follow-up, 67 patients had been treated medically and 40 had undergone revascularization (30 percutaneous coronary intervention and 10 coronary artery bypass grafting). Of the 75 patients referred for ICA, 40 (53%) required revascularization. No significant CAD was identified in 17 (33%) of the 52 patients clinically identified as HR-ACS. CTA correctly identified all 40 patients (100%) who underwent revascularization, but incorrectly allocated 6 patients to revascularization who were subsequently treated medically (κ = 0.88; 95% CI 0.79 to 0.97; Table 4 ). CTA correctly predicted the mode of treatment (medical therapy, percutaneous coronary intervention, or coronary artery bypass grafting) in 94 (88%) of the 107 patients (κ = 0.78; 95% CI 0.66 to 0.89) and correctly allocated 25 (83%) of 30 patients to percutaneous coronary intervention and 8 (80%) of 10 to coronary artery bypass grafting ( Table 5 ).



