Studies have demonstrated that the apolipoprotein B/apolipoprotein A-I (apoB/apoA-I) ratio predicts cardiovascular risk better than any of the cholesterol indexes. A number of factors that define the metabolic syndrome (MS) differ across African-American and European-American ethnicities. We assessed the relation of the apoB/apoA-I ratio to MS and coronary artery disease (CAD) in 224 African Americans and 304 European Americans. The MS was defined using the revised National Cholesterol Education Program Adult Treatment Panel III criteria, and CAD was assessed as ≥50% stenosis or a continuous cardiovascular score (0 to 75). The European Americans had a greater apoB/apoA-I ratio than the African Americans (1.15 vs 1.07, p = 0.008). The apoB/apoA-I ratio was associated with presence of the MS in both European Americans (odds ratio 5.9, 95% confidence interval 2.53 to 13.57, p <0.001) and African Americans (odds ratio 8.3, 95% confidence interval 3.52 to 19.25, p <0.001) and was greater in subjects with the MS than in those without the MS (1.21 vs 1.04, p <0.001, for European Americans and 1.20 vs 0.94, p <0.001, for African Americans). A stepwise increase was seen in the prevalence of the MS across the apoB/apoA-I ratio tertiles in both ethnic groups (chi-square = 13.1, p <0.001, for European Americans and chi-square = 19.6, p <0.001, for African Americans). On multiple regression analyses, the apoB/apoA-I ratio independently predicted CAD in African Americans (β = 0.242, p = 0.011). The cardiovascular score was significantly increased across the apoB/apoA-I ratio tertiles in the European-American subjects with the MS (p = 0.001). However, this association was seen in the African-American subjects without the MS (p = 0.023). In conclusion, the apoB/apoA-I ratio differed across ethnicities and was associated with presence of the MS in both groups. Among African Americans, an elevated apoB/apoA-I ratio independently predicted a greater risk of CAD.
A number of population-based studies have suggested that the apolipoprotein B (apoB)/apolipoprotein A-I (apoA-I) ratio, an indicator of the balance between atherogenic and atheroprotective cholesterol transport, predicts cardiovascular risk more accurately and more strongly than the use of either apoB or apoA-I alone or any of the other cholesterol indexes. On the other hand, a cluster of metabolic abnormalities defined as the metabolic syndrome (MS) has been associated with increased cardiovascular risk. We have previously reported on the differential distribution of the MS components across the African-American and European-American ethnicities, with less frequent lipid abnormalities (hypertriglyceridemia and low high-density lipoprotein [HDL] cholesterol) among African Americans. Furthermore, patients with atherogenic dyslipidemia such as the MS most likely have an increased number of small, dense, low-density lipoprotein particles (corresponding to higher apoB levels) at relatively modest low-density lipoprotein cholesterol levels. Thus, in the present study, we investigated whether the apoB/apoA-I ratio is related to the MS and its components and coronary artery disease (CAD) in the 2 ethnic groups with varying frequencies of the MS components.
Methods
The subjects were recruited from a patient population scheduled for diagnostic coronary angiography either at Harlem Hospital Center (New York, New York) or at the Mary Imogene Bassett Hospital (Cooperstown, New York). The study design and inclusion and exclusion criteria have been previously described. In brief, 648 patients, self-identified as European American (n = 344), African American (n = 232), or other ethnicity (n = 72), were enrolled. Of the 576 European-American and African-American subjects, 48 were excluded because of incomplete data (16 had missing coronary angiographic data, 17 lacked information on waist circumference, 8 had missing HDL cholesterol levels, and 7 lacked information on hypertension). The exclusion criteria for the present study included the use of lipid-lowering drugs. The present report was therefore based on the findings from 528 subjects (304 European Americans and 224 African Americans). The institutional review boards at Harlem Hospital Center, Mary Imogene Bassett Hospital, Columbia University College of Physicians and Surgeons, and University of California, Davis, School of Medicine approved the study, and all subjects provided informed consent.
The blood pressure was measured using a random-zero mercury sphygmomanometer. The mean of 3 measurements of the systolic and diastolic blood pressure was used. The waist circumference was calculated as the average of 2 measurements taken after inspiration and expiration at the midpoint between the lowest rib and the iliac crest. The participants were asked to fast for 12 hours, and blood samples were drawn approximately 2 to 4 hours before the catheterization procedure. The serum and plasma samples were separated and stored at −80°C before analysis. The concentrations of triglycerides (Sigma Diagnostics, St. Louis, Missouri), total cholesterol, and glucose (Roche, Somerville, New Jersey) were determined using standard enzymatic procedures. The HDL cholesterol levels were measured after precipitation of apoB-containing lipoproteins with dextran sulfate. ApoB and apoA-I were measured using rate immunonephelometry (Array, Beckman, Brea, California).
We defined the MS according to the revised National Cholesterol Education Program Adult Treatment Panel III criteria by the presence of ≥3 of the following: fasting plasma glucose level ≥100 mg/dl, serum triglyceride level ≥150 mg/dl, serum HDL cholesterol level <40 mg/dl for men and <50 mg/dl for women, blood pressure ≥130/85 mm Hg or hypertension treatment, and waist circumference >102 cm for men and >88 cm for women.
The coronary angiograms were read by 2 experienced readers who were unaware of the patients’ identity, clinical diagnosis, and laboratory results. The readers recorded the location and extent of luminal narrowing for 15 segments of the major coronary arteries. A composite cardiovascular score (0 to 75) was calculated according to the determination of the presence of stenosis on a scale of 0 to 5 of the 15 predetermined coronary artery segments. The presence of CAD was defined as the presence of ≥50% stenosis in any 1 of the 15 coronary artery segments.
The data analyses were done using the Statistical Package for Social Sciences statistical analysis software (SPSS, Chicago, Illinois). The results are expressed as the mean ± SE and the median with interquartile ranges for non-normally distributed values. The triglyceride and insulin levels and cardiovascular scores were logarithmically transformed to achieve normal distributions. Group means were compared using the Student t test. Age- and gender-adjusted Pearson’s partial correlation coefficients were calculated for the apoB/apoA-I ratio and the MS components across ethnicities. Proportions were compared between groups using chi-square analysis and Fisher’s exact test, as appropriate. Logistic regression analysis was applied to assess the association between the apoB/apoA-I ratio and the presence of the MS. Multiple linear regression analyses were used to explore the independent association of the variables with the cardiovascular score. One-way analysis of variance was used to compare the mean levels of the independent variables across the apoB/apoA-I ratio tertiles, and post hoc analyses were performed using the Tukey honestly significant difference test. Unless otherwise noted, a nominal 2-sided p value <0.05 was used to assess significance.
Results
As expected, African Americans had greater HDL cholesterol (p <0.001) and apoA-I (p <0.001) levels and lower levels of triglycerides (p <0.001) than the European Americans ( Table 1 ). The total cholesterol, low-density lipoprotein cholesterol, and apoB levels were similar in the 2 ethnic groups. The apoB/apoA-I ratio was significantly greater in the European Americans compared to the African Americans (1.15 vs 1.07, p = 0.008; Table 1 ).
| Characteristic | European Americans (n = 304) | African Americans (n = 224) | p Value |
|---|---|---|---|
| Men/women | 195/109 | 126/98 | NS |
| Metabolic syndrome (n) | 199 (65%) | 110 (49%) | <0.001 |
| Coronary artery disease (n) | 173 (57%) | 99 (44%) | 0.003 |
| Diabetes mellitus (n) | 63 (21%) | 66 (29%) | 0.018 |
| Age (years) | 56.6 ± 0.6 | 54.8 ± 0.6 | 0.023 |
| Systolic blood pressure (mm Hg) | 125 ± 1.0 | 129 ± 2.0 | NS |
| Diastolic blood pressure (mm Hg) | 75 ± 0.6 | 79 ± 1.4 | 0.005 |
| Waist circumference (cm) | 105 ± 1.0 | 96 ± 1.1 | <0.001 |
| Total cholesterol (mg/dl) | 197 ± 2.3 | 198 ± 3.0 | NS |
| Low-density lipoprotein cholesterol (mg/dl) | 123 ± 2.0 | 126 ± 2.8 | NS |
| High-density lipoprotein cholesterol (mg/dl) | 41 ± 0.7 | 49 ± 1.1 | <0.001 |
| Triglycerides (mg/dl) | 151 (110–216) | 106 (80–144) | <0.001 |
| Glucose (mg/dl) | 132 ± 3.8 | 119 ± 3.3 | 0.013 |
| Insulin (μU/ml) | 15.1 (9.2–25.2) | 14.1 (8.7–21.7) | NS |
| Apolipoprotein B (mg/dl) | 136 ± 2.0 | 134 ± 2.7 | NS |
| Apolipoprotein A-I (mg/dl) | 122 ± 1.3 | 130 ± 1.9 | <0.001 |
| Apolipoprotein B/Apolipoprotein A-I ratio | 1.15 ± 0.33 | 1.07 ± 0.37 | 0.008 |
| Composite cardiovascular score | 12.9 (1.9–27.1) | 8.3 (1.5–24.9) | NS |
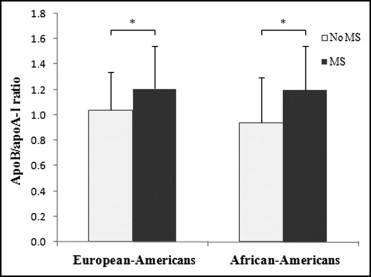
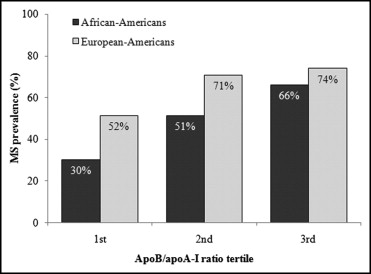
The apoB/apoA-I ratio was significantly associated with presence of the MS in both European Americans (odds ratio 5.9, 95% confidence interval 2.53 to 13.57; p <0.001) and African Americans (odds ratio 8.3%, 95% confidence interval 3.52 to 19.25; p <0.001). As seen in Figure 1 , the apoB/apoA-I ratio was significantly greater in the subjects with the MS compared to those without the MS in both ethnic groups (1.21 vs 1.04, p <0.001, for European Americans and 1.20 vs 0.94, p <0.001, for African Americans). To explore the association between the apoB/apoA-I ratio and the MS in more detail, we dichotomized the study subjects into 3 groups according to their apoB/apoA-I level. A stepwise increase was seen in the prevalence of the MS across the apoB/apoA-I ratio tertiles in both ethnic groups (chi-square = 13.1, p <0.001, for European Americans and chi-square = 19.6, p <0.001, for African Americans; Figure 2 ). Furthermore, as seen in Figure 2 , European Americans had a greater prevalence of the MS than did the African Americans for all apoB/apoA-I ratio tertiles. Irrespective of ethnicity, the apoB/apoA-I ratio significantly and positively correlated with the systolic blood pressure and triglyceride levels and negatively with the HDL cholesterol levels ( Table 2 ). In addition, among the European Americans, the apoB/apoA-I ratio correlated significantly with the waist circumference (p = 0.008). The apoB/apoA-I ratio was significantly increased with an increasing number of the MS components in both European Americans (p <0.001) and African Americans (p <0.001; Supplemental Figure e1 ).
| Variable | European Americans | p Value | African Americans | p Value |
|---|---|---|---|---|
| Waist circumference (cm) | 0.154 | 0.008 | 0.170 | NS |
| Systolic blood pressure (mm Hg) | 0.144 | 0.013 | 0.304 | 0.005 |
| Diastolic blood pressure (mm Hg) | 0.059 | NS | 0.156 | NS |
| High-density lipoprotein cholesterol (mg/dl) | −0.454 | <0.0001 | −0.579 | <0.0001 |
| Triglycerides (mg/dl) | 0.415 | <0.0001 | 0.406 | <0.0001 |
| Glucose (mg/dl) | 0.080 | NS | 0.190 | NS |
Additional analysis using multiple linear regression models was performed to explore whether the apoB/apoA-I ratio predicts CAD (as measured by the composite cardiovascular score) and whether this association would be independent of other established cardiovascular disease risk factors and/or the presence of the MS ( Table 3 ). When the apoB/apoA-I ratio and other major cardiovascular disease risk factors were considered (i.e., model 1), age (β = 0.375, p <0.001), gender (β = −0.237, p <0.001), hypertension (β = 0.168, p = 0.002), and smoking (β = 0.158, p = 0.002) were key determinants, explaining 30% of the cardiovascular score in European Americans. No significant association was found between the apoB/apoA-I ratio and CAD in this particular ethnic group. In contrast, for African Americans, the apoB/apoA-I ratio (β = 0.335, p = 0.014) and age (β = 0.395, p <0.001) were independently and strongly associated with the cardiovascular score. When the MS was included in the model (i.e., model 2), in European Americans, the independent association of age (β = 0.395, p <0.001), gender (β = −0.249, p <0.001), and smoking (β = 0.156, p = 0.003) with CAD all remained significant, with the addition of the MS (β = 0.114, p = 0.037). For African Americans, the association of the apoB/apoA-I ratio (β = 0.242, p = 0.011) and age (β = 0.383, p <0.001) with CAD both remained significant, but no association was seen with the MS.
| Model | Independent Variables | R 2 | F | β | p Value |
|---|---|---|---|---|---|
| Model 1 | |||||
| European Americans | 0.301 | 13.0 | <0.001 | ||
| Age (years) | 0.375 | <0.001 | |||
| Gender (male/female) | −0.237 | <0.001 | |||
| Low-density lipoprotein cholesterol (mg/dl) | 0.012 | NS | |||
| High-density lipoprotein cholesterol (mg/dl) | −0.035 | NS | |||
| Triglycerides (mg/dl) | 0.002 | NS | |||
| Waist circumference (cm) | −0.001 | NS | |||
| Hypertension (yes/no) | 0.168 | 0.002 | |||
| Smoking (yes/no) | 0.158 | 0.002 | |||
| Apolipoprotein B/apolipoprotein A-I | 0.112 | NS | |||
| African Americans | 0.225 | 6.8 | <0.001 | ||
| Age (years) | 0.395 | <0.001 | |||
| Gender (male/female) | −0.042 | NS | |||
| Low-density lipoprotein cholesterol (mg/dl) | −0.044 | NS | |||
| High-density lipoprotein cholesterol (mg/dl) | 0.116 | NS | |||
| Triglycerides (mg/dl) | 0.106 | NS | |||
| Waist circumference (cm) | −0.044 | NS | |||
| Hypertension (yes/no) | −0.039 | NS | |||
| Smoking (yes/no) | 0.085 | NS | |||
| Apolipoprotein B/apolipoprotein A-I | 0.335 | 0.014 | |||
| Model 2 | |||||
| European Americans | 0.287 | 18.9 | <0.001 | ||
| Age (years) | 0.395 | <0.001 | |||
| Gender (male/female) | −0.249 | <0.001 | |||
| Low-density lipoprotein cholesterol (mg/dl) | 0.014 | NS | |||
| Smoking (yes/no) | 0.156 | 0.003 | |||
| Metabolic syndrome (yes/no) | 0.114 | 0.037 | |||
| Apolipoprotein B/apolipoprotein A-I | 0.126 | NS | |||
| African Americans | 0.209 | 9.5 | <0.001 | ||
| Age (years) | 0.383 | <0.001 | |||
| Gender (male/female) | −0.049 | NS | |||
| Low-density lipoprotein cholesterol (mg/dl) | 0.014 | NS | |||
| Smoking (yes/no) | 0.097 | NS | |||
| Metabolic syndrome (yes/no) | 0.046 | NS | |||
| Apolipoprotein B/apolipoprotein A-I | 0.242 | 0.011 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


