A normal coronary angiogram (CA) has been reported to confer a good prognosis. However, how this applies to patients aged ≥65 years is not well known. From 1986 to 1996, 11,625 patients aged ≥65 underwent coronary angiography. We identified 271 patients with either normal (NORM, n = 160) CA or <30% diameter stenosis disease (NEAR-NORM, n = 111). Using the Myocardial Infarction Data Acquisition System, we examined the probability of survival and the risk of developing an ischemic event or undergoing a revascularization procedure during an average of 15.1 ± 6.2 years (range 0.5 to 25.8 years). Matched actuarial subjects were used to compare survival to the general population. The incidence of an ischemic event was low (2.0 events per 100 persons/year for the NORM and 2.8 patients per 100 persons/year for the NEAR-NORM group, p = NS). Rates of revascularization were higher in the NEAR-NORM group compared to the NORM group (1 per 100 persons/year vs 0.5 per 100 persons/year, p = 0.04). During the 25.8-year follow-up, there were 77 deaths (48.4%) for the NORM and 64 (57.1%) for the NEAR-NORM group (χ2 = 1.7, NS). The NORM group survived 6,789 days, 1,517 more days than the actuarial subjects (95% confidence interval [CI] 1,072 to 1,956; p <0.0001) and the NEAR-NORM group survived 5,922 days, 875 more days (95% CI 368 to 1,376; p <0.005). In conclusion, patients with normal or near-normal CA at age ≥65 years have a low rate of myocardial ischemic events and have significantly longer survival than matched subjects from the general population.
The clinical course of patients with normal or minimally abnormal coronary angiograms (CA) has motivated great interest throughout the years. Most studies published on this topic have shown that angiographically normal coronary arteries are associated with a favorable prognosis. These studies however have the limitation of being performed in young subjects and include only short-term follow-up. Currently, there is not enough information to answer the question whether a normal or near-normal CA in patients aged ≥65 years is associated with long survival. In the present analysis, we studied the natural history of patients aged ≥65 years with normal or near-normal (<30% diameter stenosis) CA. In this population, we examined the incidence of myocardial ischemic events, revascularization procedures, and survival. We then compared the survival of these patients to that of actuarial matched subjects from the general population.
Methods
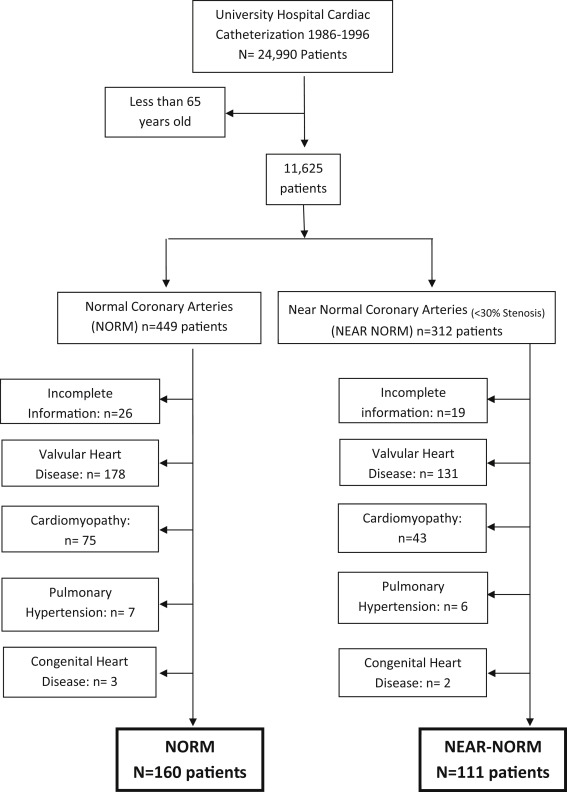
All patients who had a catheterization procedure from 1986 to 1996 at a single-site university hospital and had either a normal CA (no diameter stenosis, NORM) or near-normal CA (<30% diameter stenosis, NEAR-NORM) were identified from medical records. Information regarding family history of coronary artery disease, history of smoking, hypertension, hyperlipidemia, and diabetes mellitus at the time of the angiogram was also obtained. Indications for coronary angiography were (1) abnormal stress test; (2) chest pain with or without electrocardiographic changes; (3) syncope; and (4) unexplained dyspnea. In cases where an abnormal stress test and chest pain were indications, the indication was classified as abnormal stress test. Outcomes were admissions for stable angina pectoris, unstable angina pectoris, myocardial infarction, percutaneous coronary intervention (PCI), coronary artery bypass grafting, and death (cardiovascular and all cause). This information was obtained from Myocardial Infarction Data Acquisition System, a New Jersey (NJ) statewide repository of all nonfederal hospital discharges of patients with cardiovascular diagnosis and procedures. The accuracy of the information in the database was previously validated. Out-of-hospital death information was obtained by matching Myocardial Infarction Data Acquisition System records with the NJ death registration files using public automated software (The Link King, www.the-link-king.com ). From 1986 to 1996, 11,625 catheterizations were performed on patients aged ≥65 years. We identified 761 subjects with normal or near-normal CA. Patients with cardiomyopathy, pulmonary hypertension, congenital, and valvular disease were excluded, leaving 271 patients with either NORM (n = 160) or NEAR-NORM CA (n = 111), Figure 1 .
Chi-square test was used to test differences in demographics (age, gender, and race) risk factors (hypertension, diabetes, hyperlipidemia, smoking, and family history) and indications for CA between the 2 groups. Age was grouped into 3 categories (65 to 69, 70 to 74, and ≥75 years). Fisher’s exact test was used when the number of patients per cell was <5. Cumulative incidence and incidence rate were calculated for each outcome. We studied differences in time to event for the 2 groups using Cox proportional hazard models on 4 outcomes: ischemic events, revascularization procedures, cardiovascular, and all-cause death. A “cardiac event” outcome, including ischemic events, revascularization, and cardiovascular death, was also examined. We adjusted for the competing risk of death when considering ischemic events or revascularization as outcome and noncardiac death when considering cardiovascular deaths or the “cardiac event” outcome. Hazard ratios for each outcome in the NEAR NORMs compared to NORMs at various time points were estimated after adjusting for demographic and risk factors. Kaplan–Meier survival curves were constructed for the NORM and NEAR-NORM groups for each outcome. The survival rate of the studied population was compared with that of the general population in the United States. For this purpose, we obtained actuarial subjects matched by age, race, gender, and year of catheterization. To determine whether patients with angiographically normal or near-normal coronary arteries lived longer than actuarial subjects, a Monte Carlo technique was used to obtain the expected survival curves. All statistical analyses were performed using the software SAS version 9.3 (SAS Institute Inc, Cary, North Carolina) and R . A p value <0.05 was considered significant. The study was approved by the institutional review board.
Results
The baseline clinical characteristics of the population and the indications for CA are shown in Table 1 . There were no significant differences between the NORM and NEAR-NORM groups in any of the clinical characteristics or indication for CA. Chest pain with or without changes in the electrocardiogram was the most frequent indication for CA followed by abnormal stress test. The average follow-up time for this study was 15.1 years (total of 4,096 person-years), and the inter quartile range was between 11 and 20 years.
| Variables | Normal (n=160) | Near Normal (n=111) | Total (n=271) | p Value |
|---|---|---|---|---|
| Age (years) | ||||
| Mean Age (± SD) | 70(±4.5) | 71(±4.6) | 0.89 | |
| 65-69 | 82 (51%) | 48 (43%) | 130(48%) | 0.34 |
| 70-74 | 55 (34%) | 41 (37%) | 96 (35%) | |
| ≥ 75 | 23 (15%) | 22 (20%) | 45 (17%) | |
| Male | 40 (25%) | 38 (34%) | 78 (29%) | 0.10 |
| Female | 120 (75%) | 73 (66%) | 193 (71%) | |
| White | 117 (73%) | 77 (70%) | 194 (72%) | 0.72 |
| Black | 37 (23%) | 28 (25%) | 65 (24%) | |
| Others | 6 (4%) | 6 (5%) | 12 (4%) | |
| Hypertension | 86 (54%) | 72 (65%) | 158 (58%) | 0.07 |
| Diabetes mellitus | 22 (14%) | 21 (19%) | 43 (16%) | 0.25 |
| Hyperlipidemia | 48 (30%) | 37 (33%) | 85 (31%) | 0.56 |
| Smoker | 37 (23%) | 33 (30%) | 70 (26%) | 0.22 |
| Family History of CAD | 34 (21%) | 30 (27%) | 64 (24%) | 0.27 |
| Indication For Coronary Arteriography | ||||
| Chest Pain w or w/o Abnormal EKG | 74 (46%) | 59 (53%) | 133 (48%) | 0.26 |
| Abnormal Stress Test | 58 (36%) | 40 (36%) | 98 (35%) | 0.97 |
| Syncope | 6 (4%) | 2 (2%) | 8 (3%) | 0.35 |
| Unexplained Dyspnea | 16 (10%) | 8 (7%) | 24 (9%) | 0.42 |
| Unknown | 6 (4%) | 2 (2%) | 8 (3%) | 0.35 |
During the entire follow-up period, there were 38 patients with 51 ischemic events (17 myocardial infarction, 11 unstable angina, and 23 stable angina) in the NORM group and 34 patients with 45 ischemic events (17 myocardial infarction, 11 unstable angina, and 17 stable angina) in the NEAR-NORM group. The incidence of an ischemic event was 2.0 events per 100 persons/year for the NORM group and 2.8 events per 100 persons/year for the NEAR-NORM GROUP (p = 0.13). The incidence of revascularization procedures was twice as higher in the NEAR-NORM group with 15 patients (1.0 per 100 persons/year) compared to the 11 patients (0.5 per 100 persons/year, p = 0.04) in the NORM group. In those patients who underwent revascularization, percutaneous coronary intervention was used in 91% of the NORM group and in 60% of the NEAR-NORM group (p = 0.08). Hypertension was the only independent predictor of cardiovascular events (hazard ratio [HR] 2.1, 95% confidence interval [CI] 1.0 to 4.1), and there were no independent predictors of revascularization ( Table 2 ).
| Ischemic Event HR (95% CI) | Revascularization HR (95% CI) | Cardiovascular Death HR (95% CI) | All-cause Death HR (95% CI) | ||
|---|---|---|---|---|---|
| Normal Coronary Arteries | Age (≥70) | 1.3 (0.7, 2.5) | 2.2 (0.7, 7.6) | 1.1 (0.5, 2.3) | 1.4 (0.9, 2.2) |
| Female | 0.9 (0.4, 1.9) | 1.6 (0.3, 7.2) | 1.3 (0.5, 3.2) | 0.9 (0.6, 1.5) | |
| White | 0.7 (0.3, 1.3) | 1.3 (0.3, 4.8) | 3.3 (1.1, 9.5) * | 2.6 (1.4, 4.7) ** | |
| Hypertension | 2.1 (1.0, 4.1) * | 4.3 (0.9, 19.9) | 1.9 (0.9, 4.0) | 1.5 (1.0, 2.4) | |
| Diabetes | 1.9 (0.9, 4.1) | 1.5 (0.3, 7.1) | 1.5 (0.6, 3.9) | 1.2 (0.7, 2.2) | |
| Hyperlipidemia | 1.3 (0.7, 2.5) | 0.9 (0.2, 3.4) | 0.9 (0.4, 2.0) | 1.0 (0.6, 1.7) | |
| Smoking | 1.1 (0.5, 2.1) | 0.9 (0.2, 4.0) | 2.5 (1.2, 5.4) ** | 1.8 (1.1, 2.9) ** | |
| Family history | 1.6 (0.8, 3.2) | 0.3 ( 0.04, 2.6) | 1.2 (0.6, 2.8) | 0.8 (0.4, 1.3) | |
| Near Normal Coronary Arteries | Age (≥70) | 1.4 (0.7, 2.9) | 1.8 (0.6, 5.2) | 1.1 (0.5, 2.6) | 1.4 (0.9, 2.4) |
| Female | 1.2 (0.6, 2.5) | 0.6 (0.2, 1.8) | 0.8 (0.3, 1.9) | 06 (0.4, 1.0) | |
| White | 1.2 (0.6, 2.5) | 0.4 (0.1, 1.0) | 2.3 (0.1, 6.9) | 1.8 (1.0, 3.1) * | |
| Hypertension | 1.9 (0.9, 4.3) | 1.6 (0.5, 5.2) | 0.9 (0.4, 2.1) | 1.0 (0.6, 1.7) | |
| Diabetes | 1.9 (0.8, 4.1) | 3.2 (1.1, 9.4) | 1.5 (0.5, 4.4) | 1.8 (1.0, 3.1) | |
| Hyperlipidemia | 0.7 (0.4, 1.5) | 1.1 (0.4, 3.1) | 0.4(0.1, 1.3) | 0.5 (0.3, 0.9) ** | |
| Smoking | 0.5 (0.2, 1.2) | 2.1 (0.7, 5.9) | 0.7 (0.2, 2.2) | 1.6 (1.0, 2.6) | |
| Family history | 1.3 (0.7, 2.7) | 1.0 (03, 3.1) | 0.7 (0.2, 2.0) | 1.0 (0.6, 1.7) | |
There was no significant difference between the ischemic event-free survival of the NORM and NEAR-NORM groups (HR 1.3, 95% CI 0.8 to 2.1) after adjusting for demographics and risk factors. Similarly, there was no significant difference between the revascularization-free survival of the NORM and NEAR-NORM group (HR 1.8, 95% CI 0.8 to 4.1), Figure 2 .

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


