3 Use of Diagnostic Testing
The physician confronted with a patient with suspected cardiovascular disease has a multitude of tests available to provide diagnostic and prognostic information. Chapters 4 through 10 describe the various modalities for diagnosing cardiovascular diseases. This chapter focuses on the selection of the most appropriate tests for individual patients.
Diagnostic Tests
Electrocardiography
The resting ECG is the most frequently performed investigation in evaluating patients with cardiovascular disease (see Chapter 4). Electrocardiography is a highly versatile diagnostic test, providing information on a broad spectrum of clinical conditions, ranging from metabolic disturbances (e.g., hypo- and hyperkalemia) and pharmacologic toxicity to ischemic heart disease (e.g., acute myocardial infarction [MI], unstable angina), arrhythmia, and pericardial disease (see Chapter 4). With such versatility, this simple-to-perform test is cost effective.
Echocardiography
Echocardiography provides a versatile and cost-effective method for assessing cardiac anatomy and function (see Chapter 6). The greatest values of echocardiography are the capacity for simultaneous assessment of valvular, pericardial, myocardial, and extracardiac abnormalities. Because complex image processing is not needed, the results of the study are immediately available to the experienced echocardiographer. In addition, it is possible to perform echocardiography on critically ill patients who cannot be moved, or in other circumstances when a portable test is preferable. For these reasons, echocardiography is the preferred screening imaging test for further assessing suspected myocardial dysfunction. Moreover, the use of Doppler echocardiography (Doppler) to measure flow allows the measurement of peak velocity across valves, the mapping of regurgitant jets, the estimation of pulmonary artery pressures, and the detection of shunts (e.g., ventricular and atrial septal defects). The severity of valvular heart disease and its contribution to the clinical presentation can be determined immediately. For patients with chest pain, congestive heart failure, or arrhythmias, echocardiography provides a rapid means of determining underlying cardiovascular function.
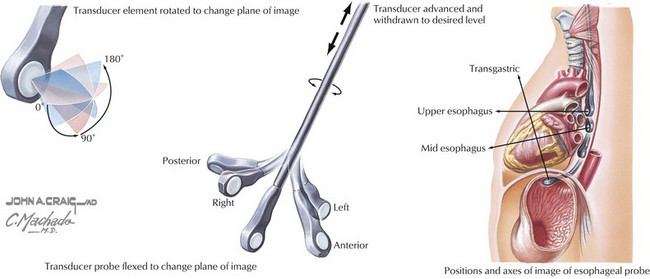
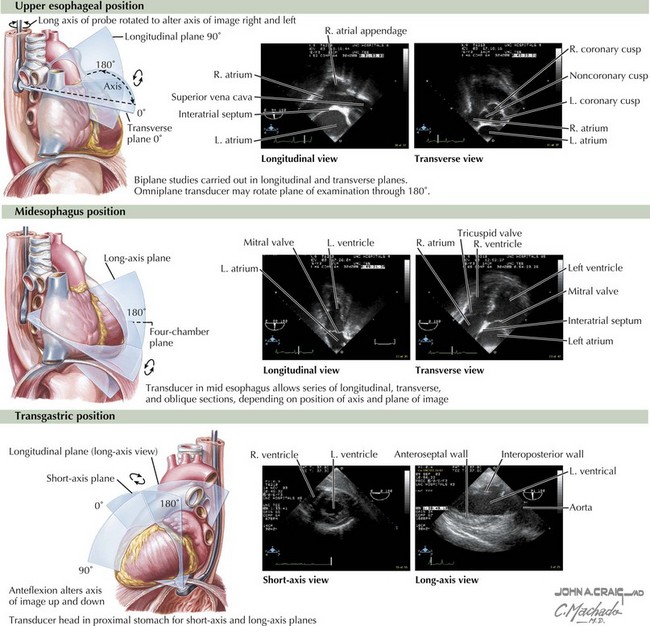
Transesophageal echocardiography adds to the sensitivity of transthoracic echocardiography, because views of the heart are not impeded by artifact related to the lungs or chest wall (Figs. 3-1 and 3-2). In addition, transesophageal echocardiography allows visualization of structures that are usually not well seen by transthoracic echocardiography (e.g., the left atrial appendage). The development of transesophageal echocardiography has also been an important advance in the management of patients who are undergoing cardiothoracic surgery, providing information on left ventricular (LV) function and the success of valvular repair. In addition, transesophageal echocardiography may allow a more accurate determination of valvular dysfunction and assessment for bacterial endocarditis, intracardiac thromboses, or both.
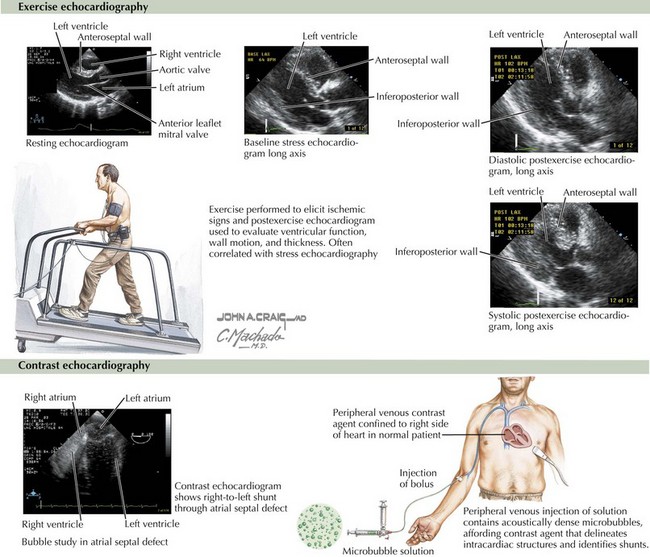
In addition to its usefulness in assessing valvular heart disease, echocardiography provides information on regional wall motion abnormalities suggestive of myocardial ischemia or necrosis in patients with CAD. The addition of pharmacologic or exercise-induced stress to detect inducible ischemia provides increased sensitivity and specificity compared with ECG exercise testing (Fig. 3-3, upper panel). In 21 studies, the sensitivity of exercise stress echocardiography averaged 84% (range 71% to 97%) and the specificity averaged 86% (range 64% to 100%). The use of echocardiography can be limited by technical considerations, including an inability to obtain diagnostic images in some patients (an estimated 15%). Stress echocardiography is indicated for individuals who have an intermediate prior probability of CAD and for individuals with abnormal ECGs or who are prescribed medications that can cause ECG abnormalities with stress (such as digoxin). In either of these cases the predictive value of exercise ECG is substantially reduced, justifying the use of an imaging technique during stress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree