Fig. 3.1
Low-magnification view of a transbronchial biopsy (left, a) and a cryobiopsy (right, b) for comparison. Notice also the lost tissue from the center of the biopsy due to overfreezing
Ancillary Studies on Biopsy Material
Microbiology Studies: These could be performed on the fluid from the bronchoalveolar lavage collected in the course of bronchoscopy. Alternatively the tissue that is removed with the staple lines from the wedge biopsy could be used for this purpose if sterile techniques are followed.
Other possibility is to dedicate one pass or more from the fine-needle aspiration procedure for that purpose if adequacy assessment is provided, and it is one of the invaluable reasons to provide the service. If there is a cell block, special stains could be performed on the material to rule out infections.
Flow Cytometry: Fine-needle aspiration passes are used for this purpose especially from lymph nodes in the chest when lymphoma is entertained in the differential diagnosis. Needle cores could be submitted in the suitable media, RPMI, for further testing.
Immunohistochemical Staining: This should be readily performed on sections from the tissue biopsies regardless of the method of obtaining them. Cell block material is also invaluable in this regard as it is better to validate the control tissue with formalin-fixed cell block than with alcohol-fixed slides. An excellent cell block technique involves letting the material clot first on a slide and then scraping the clotted material in formalin. The advantages are several. It is cheap requiring no additional reagents and uses the patient’s blood as a medium. It provides colored material that is easy to visualize in paraffin unlike agar, for instance, that is hard to distinguish from paraffin.
Molecular Testing: The emergence of targeted chemotherapy in recent years required pathologist to anticipate this type of testing on newly diagnosed lung malignancies. At the current time, only adenocarcinoma is the candidate tumor for the testing for EGFR mutations and reflex testing for ALK mutations. However, there is a new trend for genetic profiling of lung tumors to detect any mutations that could be targeted by the available drugs used in other tumors. For example, a BRAF mutation in a lung tumor, while uncommon, may help in choosing a chemotherapeutic agent used in the treatment of melanoma with the same mutation to treat the lung tumor.
The minimum number of cells for adequate DNA extraction is often cited as 150 cells. Reports of using the needle rinse for molecular have claimed high percentage of recovery of tumor cells and DNA for testing [10]. Different factors play a role in the final adequacy as the presence of necrosis, normal cell contamination, and noncellular debris or material contamination. Every effort should be made to provide adequate material for such testing whenever possible as the repeat biopsies are time consuming and expensive to arrange for.
Common Artifacts and Nonspecific Findings Identified in Small Lung Biopsy
Several artifacts are known to be present in the lung and could represent diagnostic pitfalls in the interpretation of these biopsies. Some result from the instrumentation handling and processing of the tissue (Fig. 3.2).
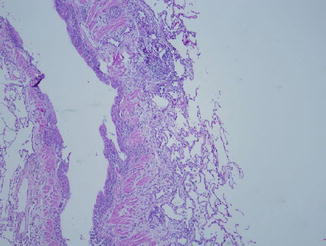
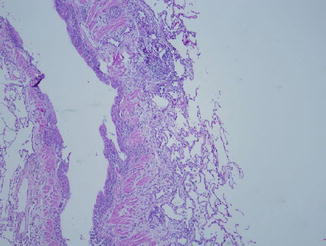
Fig. 3.2
Nonspecific peribronchial fibrosis and chronic inflammation are common, especially in older patients or smokers. The abrupt transition from fibrosed areas to normal lung parenchyma should suggest that this is a focal phenomenon and has no bearing on the disease process
Pseudo-atelectasis
Compression and squeezing the tissue between the forceps jaws causes this artifact. One way to differentiate this is to find sharp transition between the area of compression and the normal surrounding well-alveolated lung parenchyma. On higher magnification, the slit-like air spaces can discerned within those areas of compression. This artifact makes it difficult to interpret those areas affected by it. Gentle handling of the tissue and keeping it moist should help eliminate most of these artifacts. Careful interpretation is also warranted by the pathologist.
Fresh Blood in the Biopsy
Usually this is the result of bleeding from the biopsy procedure and does not indicate intra-alveolar hemorrhage. In our experience, most descriptive diagnoses of small biopsies list this blood as one of the findings for lack of any specific diagnosis. This could be confusing to the clinicians and could lead them along the wrong path investigating the underlying etiology for the alveolar hemorrhage. True intra-alveolar hemorrhage is recognized by the presence of numerous hemosiderin-laden macrophages that do not require iron stains to be recognized as they are usually engorged with the characteristic chunky refractile material, which is hemosiderin. In fact, iron stain could be problematic as it is positive on pigmented macrophages from smokers and is reported as positive in those cases, which again lead to the wrong conclusion of presence of intra-alveolar hemorrhage where in reality it is not the case (Fig. 3.3). It takes only 24 h for hemosiderin-laden macrophages to present in the lung. If they are accompanied by clotted fibrin in the alveolar space, blood vessels should be scrutinized for evidence of vasculitis.
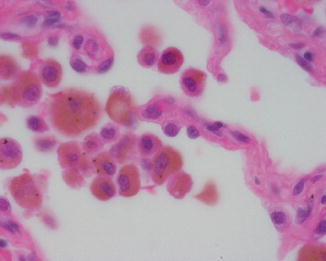
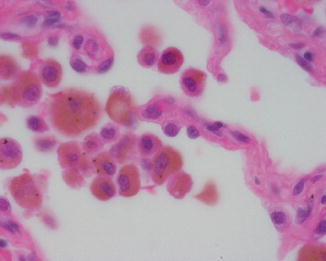
Fig. 3.3
Pigmented macrophages with tiny anthracotic pigmentation are a frequent finding in smokers’ lungs and should not be confused with hemosiderin-laden macrophages from alveolar hemorrhage
Intra-alveolar Macrophages
It is a frequent finding in many conditions to the point that it is almost nonspecific on a small biopsy if the background disease is not readily recognized. Smokers and patients with pulmonary edema or pneumonia or any type of fibrosis or condition that causes the lung to lose its elasticity are likely to result in numerous macrophages in the alveoli.
Pseudolipoid Artifact
Occasionally air bubbles in the alveolar spaces could assume a rounded configuration that is similar to fat globules noted in exogenous lipoid pneumonia (Fig. 3.4). The difference is that in true lipoid there are foamy macrophages surrounding the fat globules. Other features of aspiration pneumonia could be seen like multinucleated giant cells and vegetable matter.
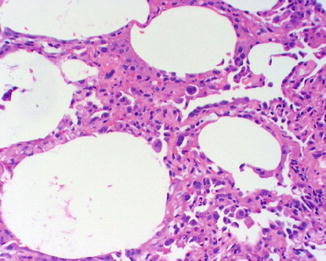
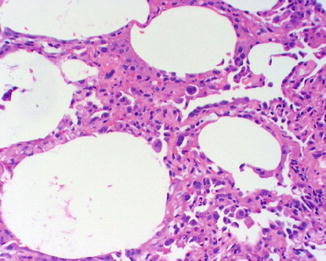
Fig. 3.4




Pseudolipoid artifact showing air bubbles with globular shape similar to that of fat globules in lipoid pneumonia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


