Tuberculous Pleural Effusions
The diagnosis of tuberculous pleuritis should be considered in any patient with an exudative pleural effusion. A pleural effusion as an isolated manifestation of tuberculosis (TB) has been likened to a primary chancre as a manifestation of syphilis. Both are self-limited and of little immediate concern, but both may lead to serious disease many years later.
PATHOGENESIS AND PATHOPHYSIOLOGIC FEATURES
When a tuberculous pleural effusion occurs in the absence of radiologically apparent TB, it may be the sequel to a primary infection 6 to 12 weeks previously or it may represent reactivation TB (1). In industrialized countries, more pleural effusions may be due to reactivation than are due to postprimary infection (1). However, in a relatively recent study from San Francisco, pleural TB cases were approximately two times more likely to be clustered (as assessed by genotyping of the mycobacterial organisms) than were pulmonary TB and three times more likely to be clustered than nonrespiratory TB cases (2). Thirty-five percent of the pleural TB cases were clustered (2). These findings suggest that at least in San Francisco, primary infection accounts for a large percentage of pleural TB (2). However, two subsequent studies from Houston (3) and Baltimore (4) were unable to confirm these findings.
The tuberculous pleural effusion is thought to result from rupture of a subpleural caseous focus in the lung into the pleural space (5). Supporting evidence comes from the operative findings of Stead et al. (6), who reported that they could demonstrate a caseous tuberculous focus in the lung contiguous with the diseased pleura in 12 of 15 patients with tuberculous pleuritis. The remaining three patients in this series were found to have parenchymal TB, although these patients did not have caseous foci adjacent to the pleura.
It appears that delayed hypersensitivity plays a large role in the pathogenesis of tuberculous pleural effusion. As mentioned in the previous paragraph, the hypersensitivity reaction is initiated when tuberculous protein gains access to the pleural space. When guinea pigs are immunized to tuberculous protein by injecting Freund’s adjuvant containing dead tubercle bacilli into their footpads, an intrapleural injection of purified protein derivative (PPD) of tuberculin 3 to 5 weeks later causes the rapid appearance (˜within 12 to 48 hours) of an exudative pleural effusion (7). The development of the pleural effusion is suppressed when the animals are given antilymphocyte serum (8).
The neutrophil appears to play a key role in the development of experimental tuberculous pleuritis. When bacillus Calmette-Guérin (BCG)-sensitized rabbits are given BCG intrapleurally, the resulting pleural fluid contains predominantly neutrophils for the first 24 hours (9). If the animals are made neutropenic, the accumulation of pleural fluid and inflammatory cells, particularly macrophages, is decreased. The intrapleural injection of neutrophils in the neutropenic animals restores the response to control levels. The neutrophils in the pleural space appear to secrete a monocyte chemotaxin that recruits monocytes to the pleural space and thereby contributes to the formation of granulomas (9).
In this BCG model of experimental tuberculous pleuritis, macrophages predominate in the pleural fluid from day 2 to day 5 (9). It has been shown that
mesothelial cells stimulated with BCG or interferon-gamma produce macrophage inflammatory protein and monocyte chemotactic peptide (10). These two proteins account for more than 75% of the mononuclear chemotactic factor in tuberculous pleural fluid (10). After this period, lymphocytes are the predominant cells in the pleural fluid (11). When the lymphocytes first appear in the pleural fluid approximately on day 3, they do not respond to PPD. From day 5 onward, however, reactivity to PPD is found in most cases (12). The reactivity of the lymphocytes in the peripheral blood parallels that of the pleural lymphocytes (12). (See Chapter 4 for further discussion of these experimental models of tuberculous pleuritis.)
mesothelial cells stimulated with BCG or interferon-gamma produce macrophage inflammatory protein and monocyte chemotactic peptide (10). These two proteins account for more than 75% of the mononuclear chemotactic factor in tuberculous pleural fluid (10). After this period, lymphocytes are the predominant cells in the pleural fluid (11). When the lymphocytes first appear in the pleural fluid approximately on day 3, they do not respond to PPD. From day 5 onward, however, reactivity to PPD is found in most cases (12). The reactivity of the lymphocytes in the peripheral blood parallels that of the pleural lymphocytes (12). (See Chapter 4 for further discussion of these experimental models of tuberculous pleuritis.)
It is probable that delayed hypersensitivity also plays a large role in the development of tuberculous pleural effusions in humans. The mycobacterial cultures of the pleural fluid from most patients with tuberculous pleural effusions are negative (2,13,14). T lymphocytes specifically sensitized to tuberculous protein are present in the pleural fluid (15). In one report, approximately 1 in 2,000 of the lymphocytes in the pleural fluid was specifically sensitized to tuberculous protein (15). In the same report, only 1 in 15,000 of the lymphocytes in the peripheral blood was specifically sensitized to the tuberculous protein. It is unknown whether the increased percentage of specifically sensitized lymphocytes in the pleural fluid is due to their clonal expansion in the pleural fluid or is due to the migration of PPD-responding T lymphocytes from the blood to the pleural space. When pleural lymphocytes from patients with tuberculous pleural effusions are cocultured with PPD, lymphokines are produced (16). The level of lymphokine production is much greater with pleural lymphocytes than with peripheral blood lymphocytes (16).
Although delayed hypersensitivity to tuberculous protein is probably responsible for most clinical manifestations of tuberculous pleuritis, many patients when first evaluated have a negative PPD skin test. The explanation for this paradox may be a combination of two factors. First, in some (17), but not in all (18) patients with tuberculous pleuritis, a circulating mononuclear adherent cell suppresses the specifically sensitized circulating T lymphocytes in the peripheral blood. Second, there may be sequestration of PPD-reactive T lymphocytes in the pleural space involving both Leu-2 (suppressor/cytotoxic) and Leu-3 (helper) positive T cells (18).
Tuberculous pleural effusions are enriched with many potentially immunoreactive cells and substances that comprise the vigorous local cell-mediated immune response (19). Compared with peripheral blood, pleural fluid is enriched with T lymphocytes. The CD4 (helper-inducer) to CD8 (suppressor/cytotoxic) ratio is 3:4 in pleural fluid, compared with 1:7 in blood (19). Pleural fluid lymphocytes from patients with tuberculous pleuritis show greater responsiveness to PPD than do peripheral blood lymphocytes (20).
The obvious explanation for the development of the tuberculous pleural effusion is that the delayed hypersensitivity reaction increases the permeability of the pleural capillaries to protein, and the increased protein levels in the pleural fluid result in a much higher rate of pleural fluid formation and accordingly result in the accumulation of pleural fluid. However, this does not appear to be the mechanism for the pleural fluid accumulation. Apicella and Allen (21) were unable to demonstrate any striking increase in the inflow of protein into the pleural space in their experimental model of delayed hypersensitivity tuberculous pleuritis. They did, however, demonstrate a dramatic decrease in the clearance of protein from the pleural space (21). Leckie and Tothill (22) reported that the pleural lymphatic flow from patients with TB was approximately 50% that of patients with congestive heart failure. It is probable that the intense inflammatory reaction in the parietal pleura impedes the lymphatic drainage from the pleural space (see Chapter 2) and leads to the accumulation of pleural fluid. It should be noted, however, that when mesothelial cells are cultured in the presence of BCG, vascular endothelial growth factor (VEGF) is released from the mesothelial cells, and the expression of adherens junction protein is down regulated (23). However, extrapolation of these results in monolayers to the in vivo situation remains to be verified.
INCIDENCE
In many areas of the world, TB remains the most common cause of pleural effusions in the absence of demonstrable pulmonary disease. For example, in one series of 642 pleural effusions from northern Spain in the mid-1990s, TB was the most common etiology of pleural effusion, accounting for 25% of all pleural effusions (24). A study from Saudi Arabia about the same time demonstrated that TB was also the most common cause of pleural effusions in that country, accounting for 37% of all pleural effusions (25).
In the United States, the annual incidence of tuberculous pleuritis has been estimated to be approximately 1,000 cases, and it is said that 3% to 5% of patients with TB will have tuberculous pleuritis (3,26,27).
It is likely that both these numbers are low. Patients with tuberculous pleuritis tend to be underreported because their mycobacterial cultures are frequently negative. Between 1988 and 1994, there were 2,817 cases of TB in patients without the acquired immunodeficiency syndrome (AIDS) who were reported to the South Carolina state TB registry; 6% of these patients had pleural effusions (28). However, in non-AIDS patients with new-onset intrathoracic TB, pleural effusions occur in more than 25% of patients in Burundi (29) and 20% in South Africa (30).
It is likely that both these numbers are low. Patients with tuberculous pleuritis tend to be underreported because their mycobacterial cultures are frequently negative. Between 1988 and 1994, there were 2,817 cases of TB in patients without the acquired immunodeficiency syndrome (AIDS) who were reported to the South Carolina state TB registry; 6% of these patients had pleural effusions (28). However, in non-AIDS patients with new-onset intrathoracic TB, pleural effusions occur in more than 25% of patients in Burundi (29) and 20% in South Africa (30).
Patients who are immunocompromised are more likely to develop TB than nonimmunocompromised individuals. Pleural TB also occurs frequently in the immunocompromised individual. Mycobacterial infection occurred in 27 of 1,261 patients (2.1%) who received renal transplants in Valencia, Spain and 3 of these had pleural effusions (31). TB occurred in 48 of 330 patients (14.5%) who were on renal dialysis in Saudi Arabia and 5 of them had pleural effusions (32).
One might anticipate that the incidence of tuberculous pleuritis would be relatively low in patients with AIDS and TB because the patient with AIDS has a compromised immunologic system, and pleural TB is thought to be due to hypersensitivity. However, overall it appears that the incidence of pleural effusions is higher in patients with AIDS. One possible explanation for this apparent paradox is that the pleural effusion in patients with AIDS is related to pleural invasion by the mycobacteria rather than to delayed hypersensitivity (33). The fact that smears and cultures are more often positive in the human immunodeficiency virus (HIV)-positive patient lends support to this hypothesis.
Although in the series referenced in the preceding text from Burundi, a slightly smaller percentage of HIV-positive patients (24%) than HIV-negative patients (28%) had pleural effusions (29), other series have shown that pleural effusions are more common in HIV-positive patients. The percentage of patients with thoracic TB who also had a pleural effusion was higher in HIV-positive patients than in HIV-negative patients in series from South Africa (38% vs. 20%) (29), Uganda (23% vs. 11%) (34), and Zimbabwe (27% vs. 13%) (35).
CLINICAL MANIFESTATIONS
Although TB is usually considered a chronic illness, tuberculous pleuritis most commonly manifests as an acute illness. In one series of 71 patients, 25 (35%) had initial symptoms of less than 1 week in duration, whereas 50 (70%) had been symptomatic for less than a month (36). In another series, 31 of 49 patients (63%) had an acute illness that most commonly mimicked acute bacterial pneumonia (5). Most patients (˜70%) have a cough, usually nonproductive, and most (˜75%) have chest pain, usually pleuritic in nature (1,5,37). If both cough and pleuritic chest pain are present, the pain usually precedes the cough. Most patients are febrile, but a normal temperature does not rule out the diagnosis. In one series, 7 of 49 patients (14%) were afebrile (5). Occasionally, the onset of TB is less acute, with only mild chest pain, perhaps with a low-grade fever and a nonproductive cough, weight loss, and easy fatigability.
In general, patients with tuberculous pleuritis are younger than patients with parenchymal TB. In one recent series from Qatar, the mean age of 100 patients with tuberculous pleuritis was 31.5 years (38). In industrialized countries, the mean age of patients with TB tends to be older. In a recent study from the United States, the mean age of the 14,000 patients with tuberculous pleuritis reported to the Communicable Disease Center in the United States between 1993 and 2003 was 49.9 years (27). Patients with pleural effusions secondary to reactivation tend to be older than those with postprimary pleural effusion (1).
Pleural effusions secondary to tuberculous pleuritis are usually unilateral and can be of any size. In one series, the effusions occupied more than two thirds of the hemithorax in 18%, between one third and two thirds of the hemithorax in 47%, and less than one third of the hemithorax in 34% (39). In another series of 46 patients with massive pleural effusions (40), 4% of the effusions were due to TB. In approximately 20 to 25% of patients with pleural effusions secondary to TB (39,41), coexisting parenchymal disease is visible on the chest radiograph. If chest CT scans are done, approximately 90% will have parenchymal abnormalities (41,42). In such patients, the pleural effusion is almost always on the side of the parenchymal infiltrate and invariably indicates active parenchymal disease. On rare occasions, pleural TB can present with pleural-based nodules and thickening (43).
Clinical Manifestations in HIV-Positive Patients
The clinical manifestations of pleural TB tend to be somewhat different in the HIV-positive patient. Patients with HIV tend to have a longer duration of illness and a lower incidence of chest pain (44).
Systemic signs and symptoms such as night sweats, fatigue, diarrhea, hepatomegaly, splenomegaly, and lymphadenopathy are significantly more common in HIV-infected patients (37). Patients with HIV are more likely to have concomitant parenchymal lesions (3). Their pleural fluid is more likely to be smear positive for acid-fast bacilli (AFB) and culture positive for AFB (44,45). If the CD4 count is less than 100, approximately 50% have a positive smear for AFB on their pleural fluid (44). HIV patients have significantly lower lymphocyte counts (45). Interestingly, the viral load per mL pleural fluid was higher than that in simultaneously obtained serum in each of eight patients in one study (46).
Systemic signs and symptoms such as night sweats, fatigue, diarrhea, hepatomegaly, splenomegaly, and lymphadenopathy are significantly more common in HIV-infected patients (37). Patients with HIV are more likely to have concomitant parenchymal lesions (3). Their pleural fluid is more likely to be smear positive for acid-fast bacilli (AFB) and culture positive for AFB (44,45). If the CD4 count is less than 100, approximately 50% have a positive smear for AFB on their pleural fluid (44). HIV patients have significantly lower lymphocyte counts (45). Interestingly, the viral load per mL pleural fluid was higher than that in simultaneously obtained serum in each of eight patients in one study (46).
NATURAL HISTORY OF UNTREATED TUBERCULOUS PLEURITIS
Without treatment, tuberculous pleuritis usually resolves spontaneously, only to return as active TB at a later date. Patiala (47) followed up for at least 7 years all 2,816 members of the Finnish Armed Forces who developed pleural effusions between 1939 and 1945. They reported that 43% of this large group of young men developed TB during the follow-up period. Even in the 1-year observation period 5 years following the initial episode, 5% of the total population studied developed active TB.
Confirmatory evidence for this large series comes from the series of Roper and Waring (48) in the United States, who followed up 141 military personnel first seen from 1940 to 1944 with a pleural effusion and a positive PPD test. In most patients, the effusions resolved and all the other symptoms disappeared within 2 to 4 months. Nevertheless, 92 of the 141 individuals (65%) subsequently developed some form of active TB. Manifest TB did not develop in the lung or elsewhere in any of the patients within 8 months of the onset of the original pleurisy. The incidence of subsequent TB was 60% in those with initially negative pleural fluid cultures for TB and 65% in those with initially positive pleural fluid cultures. In addition, the size of the original effusions and the presence or the absence of small radiologic residual pleural disease were not correlated with the subsequent appearance of active TB (48). The foregoing series emphasize the importance of making the diagnosis of tuberculous pleuritis.
Because the administration of antituberculous chemotherapy reduces the incidence of subsequent TB (5,49), it is important to establish the diagnosis of tuberculous pleuritis and initiate proper treatment. Moreover, patients in whom the diagnosis cannot be established but is considered likely should also be treated.
DIAGNOSIS
The diagnosis of tuberculous pleuritis depends on the demonstration of tubercle bacilli in the sputum, pleural fluid, or pleural biopsy specimen, or the demonstration of granulomas in the pleura. The diagnosis can also be established with reasonable certainty by demonstrating elevated levels of adenosine deaminase (ADA) or interferon-gamma in the pleural fluid (50). Study of the peripheral blood is not useful; most patients do not have leukocytosis (5). The chest radiograph usually demonstrates only the pleural fluid, but as previously mentioned, approximately 20 to 25% of the patients also have a parenchymal infiltrate due to TB (39).
Tuberculin Skin Testing
In the past, the tuberculin skin test was an important diagnostic aid in patients suspected of having tuberculous pleuritis. However, a negative skin test does not rule out the diagnosis of tuberculous pleuritis. In one series from Spain, the PPD was positive in only 66.5% of 254 patients with tuberculous pleuritis (39). In another series from Hong Kong, more than one half of the patients tested had a negative PPD (14). The factors responsible for the negative skin test in patients with tuberculous pleuritis are discussed earlier in this chapter. If a patient with a negative tuberculin skin test and tuberculous pleuritis is skin tested more than 8 weeks after the development of symptoms, the skin test will almost always be positive. Therefore, in patients with an undiagnosed exudative pleural effusion, a negative tuberculin skin test performed 8 weeks after the development of symptoms can be used to exclude the diagnosis of tuberculous pleuritis. However, if the patient is markedly immunosuppressed with HIV infection or is severely malnourished, the PPD may remain negative.
Pleural Fluid Analysis
Pleural fluid analysis is useful in the diagnosis of tuberculous pleuritis. The fluid is invariably an exudate. Frequently, the pleural fluid protein level is above 5 g/dL, and this finding suggests tuberculous pleuritis. In most patients, the pleural fluid
differential white blood cell (WBC) count reveals more than 50% small lymphocytes (5,39,51,52,53). In one series of 254 patients with tuberculous pleuritis (39), only 17 (6.7%) had fewer than 50% lymphocytes in the pleural fluid. In patients with symptoms of less than 2 weeks’ duration, the pleural fluid differential WBC is more likely to reveal predominantly polymorphonuclear leukocytes (36,54). In a second series of 214 patients, 11% had more than 50% pleural fluid polymorphonuclear leukocytes (54). If serial thoracenteses are performed, the differential WBC usually reveals a change to predominantly small lymphocytes (5). The separation of the lymphocytes into T lymphocytes and B lymphocytes is not useful diagnostically (see Chapter 7). If eosinophils are found in the pleural fluid in significant numbers (>10%), one can virtually exclude the diagnosis of tuberculous pleuritis, unless the patient has a pneumothorax or has had a previous thoracentesis (see Chapter 7).
differential white blood cell (WBC) count reveals more than 50% small lymphocytes (5,39,51,52,53). In one series of 254 patients with tuberculous pleuritis (39), only 17 (6.7%) had fewer than 50% lymphocytes in the pleural fluid. In patients with symptoms of less than 2 weeks’ duration, the pleural fluid differential WBC is more likely to reveal predominantly polymorphonuclear leukocytes (36,54). In a second series of 214 patients, 11% had more than 50% pleural fluid polymorphonuclear leukocytes (54). If serial thoracenteses are performed, the differential WBC usually reveals a change to predominantly small lymphocytes (5). The separation of the lymphocytes into T lymphocytes and B lymphocytes is not useful diagnostically (see Chapter 7). If eosinophils are found in the pleural fluid in significant numbers (>10%), one can virtually exclude the diagnosis of tuberculous pleuritis, unless the patient has a pneumothorax or has had a previous thoracentesis (see Chapter 7).
A useful study for ruling out tuberculous pleuritis is analysis of the pleural fluid for mesothelial cells (Fig. 7.1A). Four separate series have confirmed that pleural fluid from patients with TB rarely contains more than 5% mesothelial cells (51,52,55,56). Unfortunately, the absence of mesothelial cells is not diagnostic of TB because with any condition in which the pleural surfaces are extensively involved by an inflammatory process, mesothelial cells are not found in the pleural fluid. It has been suggested that HIV-infected patients with tuberculous pleuritis may have significant numbers of mesothelial cells in their pleural fluid (57). In one report (57), three HIV-infected patients with tuberculous pleuritis had significant numbers of mesothelial cells in their pleural fluid. Each of the patients had CD4 counts of less than 100/mm3 in their peripheral blood.
Adenosine Deaminase
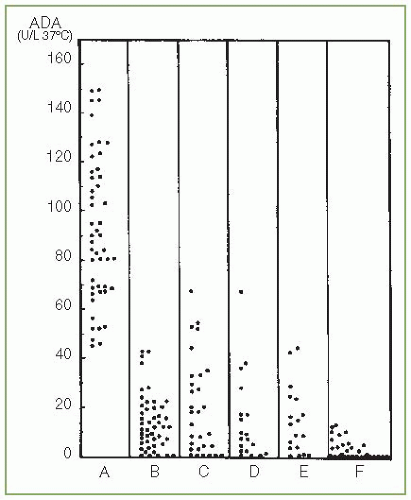
Demonstration of an elevated pleural fluid ADA level is useful in establishing the diagnosis of tuberculous pleuritis. ADA is the enzyme that catalyzes the conversion of adenosine to inosine. ADA is a predominant T-lymphocyte enzyme, and its plasma activity is high in diseases in which cellular immunity is stimulated. In an early study, Ocana et al. (58) measured the pleural fluid ADA levels in 221 pleural or peritoneal effusions (Fig. 13.1). All patients with a pleural fluid ADA level above 70 U/L had TB, whereas no patient with a pleural fluid ADA level below 40 U/L had tuberculous pleuritis. Subsequent studies of larger numbers of patients with tuberculous pleural effusions have demonstrated that the pleural fluid ADA level is higher in patients with tuberculous pleuritis than in patients with other types of pleural effusions (59,60,61,62). Different authors have used various cutoff levels for the pleural fluid ADA between 30 and 70 U/L for the diagnosis of pleural TB. The higher the pleural fluid ADA level, the more likely the patient is to have tuberculous pleuritis. Liang et al. (63) performed a meta-analysis of 63 articles evaluating the diagnostic usefulness of ADA that included 2,796 patients with tuberculous pleuritis and 5,297 patients with other diseases. They reported that the mean sensitivity was 0.92, the mean specificity was 0.90, the mean positive likelihood ratio was 9.03 and the mean negative likelihood ratio was 0.10 (63).
In general, the two main diseases other than tuberculous pleuritis that are associated with a high pleural fluid ADA are empyema and rheumatoid pleuritis. However, it should be easy to differentiate these two diseases from tuberculous pleuritis by the clinical picture and the fact that these latter two diseases do
not have pleural fluid lymphocytosis. Indeed, if the diagnostic criteria for tuberculous pleuritis includes a pleural fluid lymphocyte-to-neutrophil ratio of 0.75 or more, the specificity of the test is increased (64,65,66). This increase in specificity is due to excluding the cases with rheumatoid pleuritis or empyema. The pleural fluid ADA is elevated in patients with tuberculous pleuritis who have predominantly PMNs in their pleural fluid (54).
not have pleural fluid lymphocytosis. Indeed, if the diagnostic criteria for tuberculous pleuritis includes a pleural fluid lymphocyte-to-neutrophil ratio of 0.75 or more, the specificity of the test is increased (64,65,66). This increase in specificity is due to excluding the cases with rheumatoid pleuritis or empyema. The pleural fluid ADA is elevated in patients with tuberculous pleuritis who have predominantly PMNs in their pleural fluid (54).
There are a few other instances in which the pleural fluid ADA level will be elevated. Patients with pleural effusions due to Q fever (67) or brucellosis (68) will have elevated pleural fluid ADA levels. An occasional patient with a pleural effusion due to lymphoma or malignancy will have a lymphocytic effusion with a high ADA (69).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree