Marked increases in the awareness, treatment, and control of high low-density lipoprotein (LDL) cholesterol occurred among United States (US) adults from 1988–1994 to 1999–2004. An update to the Third Adult Treatment Panel guidelines was published in 2004, and it is unknown if these improvements have continued since the publication of these revised treatment recommendations. The aim of this study was to determine trends in the awareness, treatment, and control of high LDL cholesterol among US adults from 1999–2000 to 2009–2010 using nationally representative samples of US adults aged ≥20 years from 6 consecutive National Health and Nutrition Examination Surveys (NHANES) in 1999–2000 (n = 1,659), 2001–2002 (n = 1,897), 2003–2004 (n = 1,698), 2005–2006 (n = 1,692), 2007–2008 (n = 2,044), and 2009–2010 (n = 2,318). LDL cholesterol was measured after an overnight fast, and high LDL cholesterol and controlled LDL cholesterol were defined using the 2004 updated Third Adult Treatment Panel guidelines. Awareness and treatment of high cholesterol were defined using self-report. Among US adults, the prevalence of high LDL cholesterol did not change from 1999–2000 (37.2%) to 2009–2010 (37.8%). Awareness of high LDL cholesterol increased from 48.9% in 1999–2000 to 62.8% in 2003–2004 but did not increase further through 2009–2010 (61.5%). Among those aware of having high LDL cholesterol, treatment increased from 41.3% in 1999–2000 to 72.6% in 2007–2008 and was 70.0% in 2009–2010. Among US adults receiving treatment for high LDL cholesterol, the percentage with controlled LDL cholesterol increased from 45.0% in 1999–2000 to 65.3% in 2005–2006 and had decreased slightly by 2009–2010 (63.6%). In conclusion, high LDL cholesterol remains common among US adults. Additional efforts are needed to prevent high LDL cholesterol and increase the awareness, treatment, and control of high LDL cholesterol among US adults.
Analyses have shown that marked increases in the awareness, treatment, and control of high low-density lipoprotein (LDL) cholesterol among United States (US) adults occurred after the publication of the Third Adult Treatment Panel (ATP III) cholesterol guidelines in 2001. However, in 2003–2004, <50% of US adults with high LDL cholesterol were receiving lipid-lowering treatment, and <25% had controlled their LDL cholesterol to the levels recommended by the ATP III guidelines. Several randomized trials have been published since the release of the ATP III guidelines, and an update to the ATP III guidelines with revised treatment recommendations was published in 2004. A recent analysis of National Health and Nutrition Examination Survey (NHANES) data found that the mean LDL cholesterol among US adults decreased from 1988 to 2010. However, this report did not evaluate the prevalence and trends of high LDL cholesterol and awareness, treatment, and control among US adults. Documenting these trends may provide a useful benchmark given the forthcoming update to the Adult Treatment Panel cholesterol guidelines. The main goal of our study was to document trends in high LDL cholesterol prevalence, awareness, treatment, and control among US adults from 1999–2000 to 2009–2010. To achieve this goal, we analyzed data from 6 serial population-based NHANES.
Methods
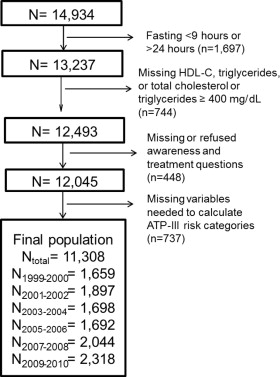
NHANES 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, and 2009–2010 were conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. Each 2-year period included a sample of the noninstitutionalized civilian US population identified through a stratified, multistage probability sampling design. This approach allows nationally representative prevalence estimates to be generated. The present analysis was limited to adult participants aged ≥20 years who were assigned to attend a morning study visit (n = 14,934). Participants are assigned for a morning study visit such that national estimates can be generated from this sample. After excluding subjects who did not fast or were missing data, 11,308 participants were included in these analyses ( Figure 1 ). The protocol for each NHANES was approved by the Institutional Review Board of the National Center for Health Statistics. Informed consent was obtained from each participant.
Data for the present analysis were collected through standardized procedures that included questionnaires, a medical examination, and phlebotomy. Participant awareness of the presence of high LDL cholesterol was defined by an affirmative response to the question “Have you ever been told by a doctor or other health professional that your blood cholesterol was high?” Use of lipid-lowering treatment was defined by affirmative responses to the following 2 questions: “To lower your cholesterol, have you ever been told by a doctor or other health professional to take prescribed medicine?” and “Are you now following this advice to take prescribed medicine?” On the basis of the average of 3 blood pressure measurements taken during the study visit, hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or self-reported use of antihypertensive medication. Waist circumference was measured to the nearest 0.1 cm at the level of the iliac crest at the end of normal respiration.
Blood collection and processing are detailed in the NHANES Laboratory/Medical Technicians Procedures Manuals. Diabetes mellitus was defined as a fasting plasma glucose level ≥126 mg/dl or self-report of a history of diabetes with concurrent antidiabetic medication use. Total and high-density lipoprotein (HDL) cholesterol and triglycerides were measured using the Hitachi 704 Analyzer (Hitachi Corporation, Tokyo, Japan) and reagents purchased from Roche/Boehringer Mannheim Diagnostics (Indianapolis, Indiana). LDL cholesterol was calculated using the Friedewald equation. Using measurement of glucose, blood pressure, waist circumference, HDL cholesterol, and triglycerides from the in-home study visit, the metabolic syndrome was defined using the harmonized definition.
For the purpose of diagnosis, treatment, and control of LDL cholesterol, the 2004 updated ATP III guidelines classify subjects on the basis of their global coronary heart disease (CHD) risk into 1 of 4 mutually exclusive CHD risk categories: (1) no CHD or CHD risk equivalents and 0 or 1 major CHD risk factors, (2) no CHD or CHD risk equivalents and 2≥ major CHD risk factors, (3) CHD not at very high risk and/or CHD risk equivalents, and (4) CHD at very high risk. CHD risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, family history of CHD (history of myocardial infarction or angina before age 50 years in first-degree relatives), and low HDL cholesterol (<40 mg/dl). HDL cholesterol ≥60 mg/dl is considered protective and offsets the presence of 1 of these risk factors. Participants who reported previous diagnoses of CHD or myocardial infarction were defined as having histories of CHD. Risk equivalents included a 10-year risk for CHD >20% estimated by the Framingham equation in the ATP III report or a history of stroke or diabetes mellitus. Data on other ATP III risk equivalents (e.g., peripheral arterial disease, aortic aneurysm) were not routinely collected in NHANES and were not used in the present analyses. In patients with CHD, current smoking, diabetes mellitus, and metabolic syndrome place them in the very high risk category. High LDL cholesterol and LDL cholesterol control were defined using the 2004 update of the ATP III treatment guidelines ( Table 1 ).
| Variable | High LDL Cholesterol | Control |
|---|---|---|
| History of CHD at very high risk ∗ | ≥70 mg/dl or use of lipid-lowering therapy | <70 mg/dl |
| History of CHD † or risk equivalent ‡ | ≥100 mg/dl or use of lipid-lowering therapy | <100 mg/dl |
| ≥2 CHD risk factors § and | ||
| 10-yr Framingham risk 10%–20% | ≥100 mg/dl or use of lipid-lowering therapy | <100 mg/dl |
| 10-yr Framingham risk <10% | ≥130 mg/dl or use of lipid-lowering therapy | <130 mg/dl |
| 0 or 1 CHD risk factor | ≥160 mg/dl or use of lipid-lowering therapy | <160 mg/dl |
∗ History of CHD and diabetes mellitus, cigarette smoking, and/or the metabolic syndrome.
† Not including subjects at very high risk.
‡ CHD risk equivalents included diabetes mellitus and stroke.
§ CHD risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, family history of CHD (history of myocardial infarction or angina before age 50 years in a first-degree relative), and low HDL cholesterol. HDL cholesterol ≥60 mg/dl is considered protective and offsets the presence of 1 of these risk factors.
Participant characteristics and the prevalence of high LDL cholesterol were calculated for each 2-year NHANES period. In subjects with high LDL cholesterol, we calculated the percentage who were aware of their diagnoses. Prevalence of treatment was calculated for all subjects with high LDL cholesterol and those aware of their diagnoses. The proportion of US adults with controlled LDL cholesterol was calculated for all subjects with high LDL cholesterol and for those receiving treatment. Trends over time were calculated using logistic regression with calendar period as an ordinal independent variable. Deviations from linearity were assessed by modeling calendar period as a quadratic term. Trends were calculated overall and for subgroups defined by age, race or ethnicity, gender, and CHD risk category. We calculated the number of US adults from 2007 to 2010 with high LDL cholesterol, overall and by CHD risk categories. To identify reasons participants did not have controlled LDL cholesterol, we calculated the number and percentage of US adults with high LDL cholesterol (1) not aware of their diagnoses of high LDL cholesterol, (2) aware but not treated, (3) treated but not controlled, and (4) with controlled LDL cholesterol. Many individuals with uncontrolled LDL cholesterol may be close to achieving their goals. Therefore, for US adults with uncontrolled high LDL cholesterol, we calculated the percentage whose LDL cholesterol levels were ≥30 mg/dl higher than their goals. Next, we used Poisson regression models to calculate the multivariate-adjusted prevalence ratios for having high LDL cholesterol and awareness, treatment, and control of this condition associated with CHD risk categories (0 or 1 risk factor [referent], ≥2 risk factors, CHD or risk equivalents, and CHD at very high risk) in the 2 most contemporary NHANES pooled together (2007 to 2010). We pooled NHANES 2007–2008 and 2009–2010 to achieve more reliable estimates (n >50 participants in every subpopulation). Prevalence ratios included adjustment for age, gender, race or ethnicity, income, education, and health insurance status.
All analyses were performed using SUDAAN 10.1 (Research Triangle Institute, Research Triangle Park, North Carolina) accounting for the NHANES sampling design. To obtain US nationally representative prevalence estimates, morning fasting sampling weights were applied to all calculations. NHANES sampling weights were recalibrated on the basis of the proportion of participants missing data by 10-year age group, gender, and race or ethnicity. Recalibration of the sampling weights corrects for differences in missing data across age, gender, and race or ethnicity strata and assumes that data within strata are missing randomly.
Results
Characteristics of participants are listed by 2-year period (1999–2000 through 2009–2010) in Table 2 . In more recent time periods, the population on average was older, less likely to have an annual household income <$20,000, more likely to have graduated from high school, and less likely to be current versus never smokers. Also, in the more recent time periods, a higher percentage of participants had government or no health insurance. Body mass index was higher and the prevalence of diabetes increased, and the prevalence of ≥2 versus 0 or 1 CHD risk factor decreased over time. Mean LDL cholesterol decreased from 125.6 to 116.9 mg/dl from 1999–2000 to 2009–2010.
| Characteristic | Calendar Period | Linear p Value | Quadratic p Value | |||||
|---|---|---|---|---|---|---|---|---|
| 1999–2000 (n = 1,659) | 2001–2002 (n = 1,897) | 2003–2004 (n = 1,697) | 2005–2006 (n = 1,692) | 2007–2008 (n = 2,041) | 2009–2010 (n = 2,316) | |||
| Age (yrs) | ||||||||
| <50 | 64.6% | 63.0% | 60.9% | 60.0% | 58.2% | 56.9% | Referent | Referent |
| 50–64 | 20.6% | 22.8% | 23.6% | 22.8% | 24.9% | 25.0% | 0.012 | 0.753 |
| ≥65 | 14.8% | 14.2% | 15.6% | 17.2% | 16.9% | 18.1% | <0.001 | 0.978 |
| Male gender | 48.0% | 48.0% | 48.0% | 47.6% | 48.4% | 48.3% | 0.812 | 0.822 |
| Race or ethnicity | ||||||||
| Non-Hispanic white | 70.8% | 72.3% | 71.8% | 71.7% | 69.9% | 68.0% | Referent | Referent |
| Non-Hispanic black | 10.2% | 10.8% | 11.5% | 11.1% | 11.0% | 11.2% | 0.574 | 0.918 |
| Hispanic | 15.0% | 12.2% | 10.9% | 11.5% | 13.3% | 13.8% | 0.912 | 0.270 |
| Other | 4.0% | 4.8% | 5.8% | 5.6% | 5.8% | 7.0% | 0.054 | 0.937 |
| Household income <$20,000 | 18.0% | 16.8% | 16.8% | 12.1% | 14.2% | 14.8% | 0.020 | 0.172 |
| High School graduate | 76.9% | 81.2% | 82.3% | 82.6% | 81.5% | 81.9% | 0.026 | 0.048 |
| Health insurance | ||||||||
| Private | 63.7% | 61.6% | 55.8% | 57.1% | 58.6% | 53.2% | Referent | Referent |
| Government | 19.6% | 22.1% | 25.7% | 24.3% | 24.1% | 25.7% | <0.001 | 0.205 |
| None | 16.7% | 16.4% | 18.6% | 18.5% | 17.3% | 21.1% | 0.007 | 0.861 |
| Smoking status | ||||||||
| Never | 49.4% | 50.0% | 51.8% | 50.6% | 54.7% | 56.0% | Referent | Referent |
| Current | 23.2% | 25.0% | 24.1% | 24.4% | 20.2% | 18.4% | 0.002 | 0.096 |
| Former | 27.5% | 25.0% | 24.1% | 25.1% | 25.1% | 25.7% | 0.179 | 0.583 |
| Body mass index (kg/m 2 ) | ||||||||
| <25 | 40.3 ± 1.9 | 34.4 ± 1.4 | 33.6 ± 1.3 | 33.6 ± 1.7 | 33.1 ± 1.1 | 31.3 ± 1.7 | Referent | Referent |
| 25–30 | 31.2 ± 0.9 | 37.1 ± 1.9 | 34.6 ± 2.0 | 31.9 ± 1.5 | 34.5 ± 1.0 | 32.7 ± 1.4 | 0.042 | 0.139 |
| ≥30 | 28.6 ± 1.8 | 28.5 ± 1.4 | 31.8 ± 1.5 | 34.6 ± 1.8 | 32.4 ± 1.4 | 36.0 ± 1.5 | <0.001 | 0.378 |
| Hypertension | 26.7% | 28.6% | 30.4% | 28.9% | 30.1% | 29.5% | 0.289 | 0.369 |
| Diabetes mellitus | 6.6% | 8.4% | 8.5% | 9.2% | 10.7% | 10.6% | <0.001 | 0.517 |
| CHD at very high risk ∗ | 67.7% | 64.5% | 70.3% | 73.8% | 78.3% | 68.9% | 0.202 | 0.436 |
| CHD risk category † | ||||||||
| 0 or 1 risk factor | 62.9% | 61.6% | 62.8% | 66.1% | 62.1% | 63.9% | Referent | Referent |
| ≥2 risk factors | 23.9% | 23.7% | 22.5% | 18.0% | 20.9% | 20.0% | 0.008 | 0.380 |
| CHD or risk equivalent | 10.6% | 11.6% | 11.3% | 12.2% | 12.8% | 12.9% | 0.174 | 0.995 |
| CHD at very high risk | 2.7% | 3.0% | 3.4% | 3.7% | 4.2% | 3.1% | 0.158 | 0.168 |
| Ever had cholesterol checked | 70.4% | 67.9% | 70.8% | 76.1% | 74.5% | 73.9% | 0.005 | 0.559 |
| LDL cholesterol (mg/dl) | 125.6 ± 1.1 | 120.9 ± 1.6 | 116.8 ± 1.2 | 115.0 ± 1.3 | 116.0 ± 1.0 | 116.9 ± 1.1 | <0.001 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


