aerosol anti-infectives
antitussives
beta2-adrenergic agonists
corticosteroids
decongestants
expectorants
leukotriene modifiers
mast cell stabilizers
mucus inhibitors
xanthines.
Monitor the patient for bronchospasm and reduction of lung function, especially if the patient has asthma or COPD.
Make sure that the patient understands how to use the aerosol correctly.
Caution the patient to report adverse effects immediately.
Advise the patient taking inhaled tobramycin to report episodes of tinnitus, changes in hearing, or voice alteration.
benzonatate (Tessalon)
codeine
dextromethorphan hydrobromide (Robitussin)
hydrocodone (Vicodin).
Obtain a history of the patient’s cough before giving the drug, and reassess the patient after giving the drug.
Look for adverse reactions and drug reactions.
Assess the patient’s and his family’s knowledge of drug therapy.
adenosine monophosphate through the stimulation of the beta2-adrenergic receptors in the smooth muscle, resulting in bronchodilation. Inhaled beta2-adrenergic agonists are preferred because they act locally in the lung, resulting in fewer adverse reactions than systemic drugs.
Caution the patient about possible adverse reactions, which may include tremors, nervousness, dizziness, headache, nausea, tachycardia, palpitations, electrocardiogram (ECG) changes, bronchospasm, and cough.
Make sure that the patient taking a long-acting beta2-adrenergic agonist knows that he can’t use this drug to treat acute symptoms because the onset isn’t quick enough.
Excessive use of a short-acting beta2-adrenergic agonist may indicate poor asthma control, requiring reassessment of the patient’s therapeutic regimen.
asthma that’s refractory to other measures. Systemic corticosteroids, such as dexamethasone (Decadron), methylprednisolone (Medrol), and prednisone, are given to manage an acute respiratory event, such as acute respiratory failure or exacerbations of COPD. These drugs should be used at the lowest effective dose and for the shortest period possible to avoid adverse reactions. These drugs are initially given I.V. and, when the patient stabilizes, the dosage is tapered and an oral form may be substituted.
DRUG | INDICATIONS | ADVERSE | PRACTICE |
|---|---|---|---|
SYSTEMIC CORTICOSTEROIDS • Dexamethasone (Decadron) • Methylprednisolone (Medrol) • Prednisone (Prednisone) | • Anti-inflammatory in acute respiratory failure, acute respiratory distress syndrome, and chronic obstructive pulmonary disease • Anti-inflammatory and immunosuppressor in asthma | • Heart failure, cardiac arrhythmias, edema, circulatory collapse, thromboembolism, pancreatitis, peptic ulcer | • Use cautiously in patients with recent myocardial infarction, hypertension, renal disease, and GI ulcer. • Monitor blood pressure and blood glucose levels. |
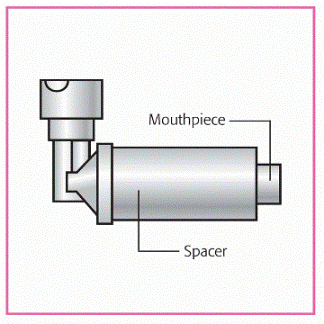
INHALED CORTICOSTEROIDS • Beclomethasone (Qvar) • Budesonide (Pulmicort) • Flunisolide (Aerobid) • Fluticasone (Flonase) • Triamcinolone (Azmacort) | • Long-term asthma control | • Hoarseness, dry mouth, wheezing, bronchospasm, oral candidiasis | • Don’t use to treat an acute asthma attack. • Use a spacer to reduce adverse effects. • Rinse mouth after use to prevent oral fungal infection. |
To reduce the risk of adverse effects occurring with inhaled drugs, use the lowest possible doses to maintain control.
Advise the patient to rinse his mouth with water after each dose to prevent oropharyngeal fungal infections.
Caution the patient that inhaled corticosteroids may cause hoarseness, throat and nose irritation, dry mouth, and headache or dizziness.
Monitor the patient for serious adverse effects, which may include dyspnea, wheezing, or bronchospasm.
Discourage the use of over-the-counter decongestants in a patient who’s hypersensitive to other sympathomimetic amines. Such a patient may also be hypersensitive to decongestants.
Monitor the patient’s blood pressure, pulse, and ECG, as instructed, particularly noting hypertension and an irregular heartbeat or tachycardia.
Maintain seizure precautions during decongestant therapy.
Note if the patient uses drugs that alter urine pH because alkaline urine increases renal tubular reabsorption of sympathomimetic amines.
Don’t give a monoamine oxidase inhibitor, a beta-adrenergic blocker, methyldopa (Aldomet), reserpine (Hiserpia), or guanethidine (Ismelin) at the same time as a topical decongestant.
Warn the patient that transient burning and stinging of the nasal mucosa may occur during administration of the topical decongestant.
Monitor the patient receiving a topical decongestant for signs of rebound nasal congestion such as red, swollen, boggy nasal mucosa. If rebound nasal congestion occurs, withhold the drug and notify the prescriber.
Encourage the patient taking a decongestant to report difficulty urinating, which is especially common in the patient with prostatic hypertrophy.
Caution the patient that the drug may produce vomiting if taken in doses larger than necessary for the expectorant action. Administer with a full glass of water.
Monitor the patient for dyspnea or ineffective cough. Instruct him to cough effectively.
Teach the patient about the prescribed drug.
Monitor the patient for adverse effects, such as diarrhea, drowsiness, nausea, vomiting, and abdominal pain.
long-term control of mild asthma. They may also be used as steroid-sparing drugs in some patients.
Zafirlukast’s absorption is decreased by food (especially highfat or high-protein meals); therefore, give the dose 1 hour before or 2 hours after meals.
Headache is the most common adverse reaction experienced with these drugs. Asthenia, dizziness, dyspepsia, gastroenteritis, and fever may also occur.
The drug isn’t used to treat acute bronchospasm.
The drug is used in conjunction with corticosteroids and other antiasthmatics.
Patients with liver impairment may require a dosage adjustment if taking zafirlukast. Monitor the patient closely for adverse reactions. Monitor liver enzyme levels in the patient taking zafirlukast because the drug may cause an increase in these levels.
process. They’re also useful for the prevention of exerciseinduced asthma.
Mast cell stabilizers shouldn’t be used for an acute asthmatic attack.
These drugs are used in combination with an inhaled beta2-adrenergic agonist or inhaled corticosteroid.
Reduce dosage gradually to the lowest effective dosage.
Discontinue the drug if eosinophilic pneumonia or pulmonary infiltrates with eosinophilia occur.
Instruct the patient to follow his practitioner’s and the manufacturer’s directions closely.
Warn the patient about the drug’s “rotten egg” smell, which may cause nausea.
Give acetylcysteine via nebulizer. Because acetylcysteine reacts with iron, copper, and rubber, frequently monitor the patient’s nebulizer equipment for reactive effects. The drug doesn’t react with glass, plastic, aluminum, or stainless steel.
Be ready to give a beta2-adrenergic agonist by aerosol, as prescribed, if the patient experiences bronchospasm.
Use 10% and 20% acetylcysteine solutions undiluted, as prescribed. If further dilution is needed, use normal saline solution or sterile water for injection.
Avoid contamination of the solution, and refrigerate an opened vial. Discard opened vials after 96 hours.
Assess the patient’s respiratory status before and after each dose, particularly noting any breathing difficulty, unproductive cough, wheezing, or dyspnea. Follow acetylcysteine administration with chest physiotherapy and postural drainage, as prescribed, and encourage coughing and deep breathing to facilitate removal of respiratory secretions. Suction the patient as needed.
Have the patient gargle after administration to relieve the unpleasant odor and dryness; wash the patient’s face to eliminate stickiness caused by the drug.
Monitor the patient closely for signs of stomatitis, such as swollen, tender gums that bleed easily, papulovesicular ulcers in the mouth and throat, malaise, irritability, and fever.
sensitivity of the brain’s respiratory center to carbon dioxide and to stimulate the respiratory drive.
asthma
chronic bronchitis
emphysema.
Instruct the patient that smoking cigarettes or marijuana increases theophylline elimination, decreasing its serum level and effectiveness.
Advise the patient that taking adrenergic stimulants or drinking caffeinated beverages may result in additive adverse effects to theophylline or signs and symptoms of xanthine toxicity.
Instruct the patient about possible adverse effects, including cardiovascular effects, such as tachycardia and palpitations, and to notify the physician if they occur.
Monitor the patient’s theophylline level during treatment.
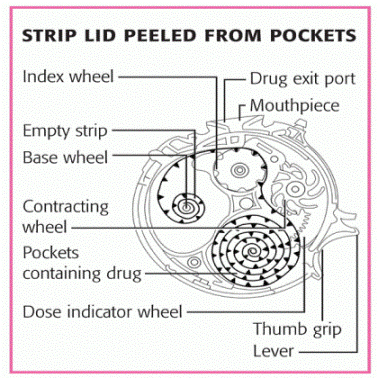
and places his mouth over the dispenser and inhales the medication. The dispenser has a dose counter so that the patient knows when he has 20 doses remaining.
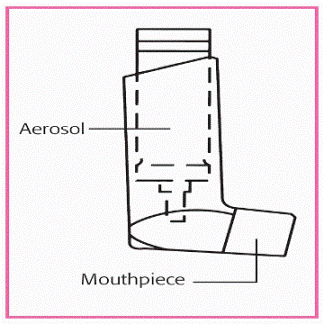
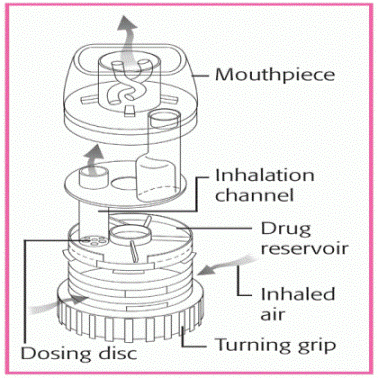
Metered-dose inhaler | Inhaler with built-in spacer |
|
|
Turbo-inhaler | Diskus dry powder inhaler |
|
|
Instruct the patient how to use the device, and encourage him to practice before actually using it to develop hand-breath coordination.
Inform the patient of possible adverse reactions to each drug.
Instruct the patient to rinse his mouth after drug administration to prevent stomatitis.
If the patient is using a steroid inhaler along with a bronchodilator, instruct him to use the bronchodilator first, wait 5 minutes, and then use the steroid inhaler.
Instruct the patient to exhale completely before using the inhaler. This increases his inspiratory effort, giving him better drug administration and distribution.
Monitor the effectiveness of the medication.
Because proper drug dosage depends on the correct use of the equipment, assess the patient’s ability to perform the medication administration.
Assess the patient’s breath sounds before and after inhaler use.
Explain the procedure to the patient.
Take the patient’s vital signs and auscultate his lung fields to establish a baseline. If possible, place the patient in a sitting or high Fowler’s position to encourage full lung expansion and promote aerosol dispersion. Encourage the patient to take slow, even breaths during the treatment.
Before using an ultrasonic nebulizer, give an inhaled bronchodilator (MDI or small-volume nebulizer) to prevent bronchospasm.
Check the patient frequently during the procedure to observe for adverse reactions. Watch for labored respirations because ultrasonic nebulizer therapy may hydrate retained secretions and obstruct airways. Monitor the patient’s vital signs and auscultate his lung fields for adventitious breath sounds and effectiveness of therapy.
Encourage the patient to cough and expectorate, or suction as needed.
Check the water level in a large-volume nebulizer at frequent intervals and refill or replace as indicated. When refilling a reusable container, discard the old water to prevent infection from bacterial or fungal growth, and refill the container to the indicator line with sterile distilled water.
Change the nebulizer unit and tubing according to your facility’s policy to prevent bacterial contamination.
If the nebulizer is heated, tell the patient to report warmth, discomfort, or hot tubing because these may indicate a heater malfunction.
Be especially careful when using ultrasonic nebulization in children. Monitor the child’s weight and note any changes. (See Nebulizer therapy in children.)
Nebulized particles can irritate the mucosa in some patients and result in bronchospasm and dyspnea. Other complications include airway burns (when heating elements are used), infection from contaminated equipment (although rare), and adverse reactions from medications.
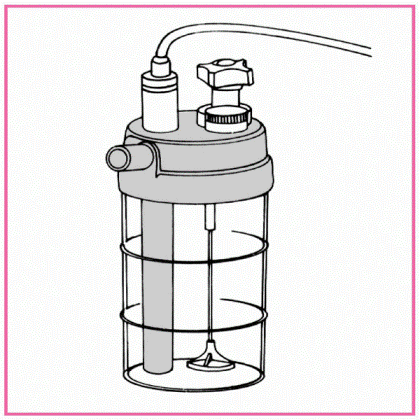
NEBULIZER | CHARACTERISTICS |
|---|---|
ULTRASONIC | Uses high-frequency sound waves to create an aerosol mist Advantages
Disadvantages
|
LARGE VOLUME (VENTURI JET)
| Works by passing air through a Venturi opening, drawing liquid up through feeding tubes, and nebulizing the solution Advantages
Disadvantages
|
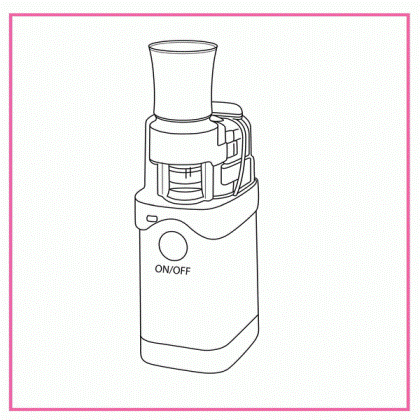
SMALL VOLUME (MINI-NEBULIZER, MAXI-MIST)
| Handheld device that disperses a moisturizing agent into microscopic droplets and delivers it to the lungs with inhalation Advantages
Disadvantages
|
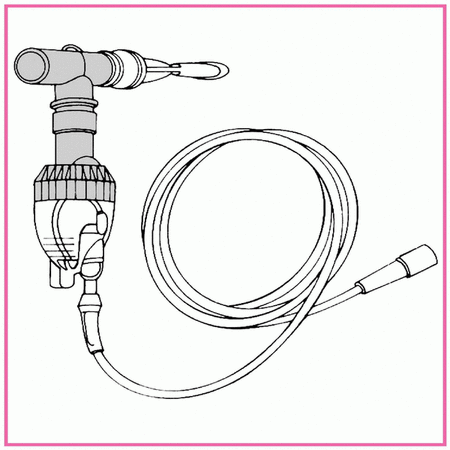
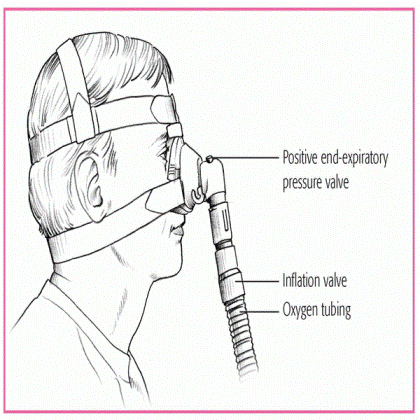
airway, a mask, or nasal prongs by means of a ventilator or a separate high-flow generating system. (See Using nasal CPAP.)
If the patient is intubated or has a tracheostomy, you can accomplish CPAP with a mechanical ventilator by adjusting the settings. Assess his vital signs, oxygen saturation, and breath sounds during CPAP.
If CPAP is delivered through a mask, a respiratory therapist usually sets up the system and fits the mask. The mask should be transparent and lightweight, with a soft, pliable seal. A tight seal isn’t required as long as pressure can be maintained. Measure arterial blood gas (ABG) analysis and bedside pulmonary function studies to establish a baseline.
Check for decreased cardiac output, which may result from increased intrathoracic pressure associated with CPAP.
Watch closely for changes in respiratory rate, rhythm, and effort. Uncoordinated breathing patterns may indicate severe respiratory muscle fatigue that can’t be helped by CPAP. Report this to the physician; the patient may need mechanical ventilation.
Check the CPAP system for pressure fluctuations, which may affect oxygenation.
Keep in mind that high airway pressures increase the risk of pneumothorax; monitor the patient for chest pain and decreased breath sounds.
Use oximetry, if possible, to monitor oxygen saturation, especially when the CPAP mask is removed to provide routine care.
If the patient is stable, remove his mask briefly every 2 to 4 hours to provide mouth and skin care along with fluids. Don’t apply oils or lotions under the mask—they may react with the mask seal material. Increase the length of time the mask is off as the patient’s ability to maintain oxygenation without CPAP improves.
Check closely for air leaks around the mask near the eyes (an area difficult to seal); escaping air can dry the eyes, causing conjunctivitis or other problems.
If the patient is using a nasal CPAP device for sleep apnea, watch for decreased snoring and mouth breathing while he sleeps. If these symptoms don’t subside, notify the physician; either the system is leaking or the pressure is inadequate to provide relief.
bronchospasm or laryngospasm
cardiac arrhythmias
hypoxemia (if attempts at intubation are prolonged or oxygen delivery is interrupted)
injury to the lips, mouth, pharynx, or vocal cords
tooth damage or loss
tracheal stenosis, erosion, and necrosis.
extubation. It’s also uncomfortable for conscious patients because it stimulates salivation, coughing, and retching. Orotracheal intubation is contraindicated in patients with orofacial injuries, acute cervical spinal injury, and degenerative spinal disorders.
If possible, explain the procedure to the patient and his family.
Obtain the correct size ET tube. The typical size for an oral ET tube for women is 7.5 mm (indicates the size of the lumen) and 8 mm for men.
Give medication as ordered to decrease respiratory secretions, induce amnesia or analgesia, and help calm and relax the conscious patient. Remove dentures and bridgework, if present, to prevent aspiration.
After securing the ET tube, reconfirm tube placement by noting bilateral breath sounds and end-tidal carbon dioxide (ETCO2) readings. (See Securing an ET tube, page 130.)
Auscultate breath sounds and watch for chest movement to ensure correct tube placement and full lung ventilation.
A chest X-ray may be ordered to confirm tube placement.
Disposable ETCO2 detectors are commonly used to confirm tube placement in emergency departments, postanesthesia care units, and critical care units that don’t use continuous ETCO2 monitoring. Follow the manufacturer’s instructions for proper use of the device. Don’t use the detector with a heated
humidifier or nebulizer because humidity, heat, and moisture can interfere with device function. (See Analyzing CO2 levels.)
Follow standard precautions, and suction through the ET tube as the patient’s condition indicates, to clear secretions and prevent mucus plugs from obstructing the tube.
After suctioning, hyperoxygenate the patient being maintained on a ventilator with the handheld resuscitation bag.
If available, use a closed tracheal suctioning system, which permits the ventilated patient to remain on the ventilator during suctioning. (See Closed tracheal suctioning, pages 132 and 133.)
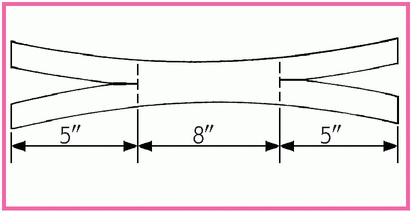
Cut one piece of 1″ cloth adhesive tape long enough to wrap around the patient’s head and overlap in front, and then cut an 8″ (20.3-cm) piece of tape and center it on the longer piece, sticky sides together.
Cut a 5″ (12.7-cm) slit in each end of the longer tape (as shown).
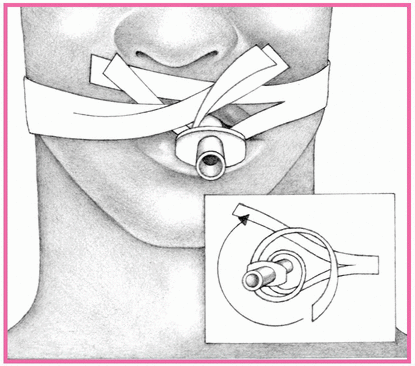
Apply benzoin tincture to the patient’s cheeks, under his nose, and under the lower lip. (Don’t spray benzoin directly on the patient’s face; the vapors can be irritating if inhaled and can harm the eyes.)
Place the top half of one end of the tape under the patient’s nose and wrap the lower half around the ET tube. Place the lower half of the other end of the tape along his lower lip and wrap the top half around the tube.
|
|
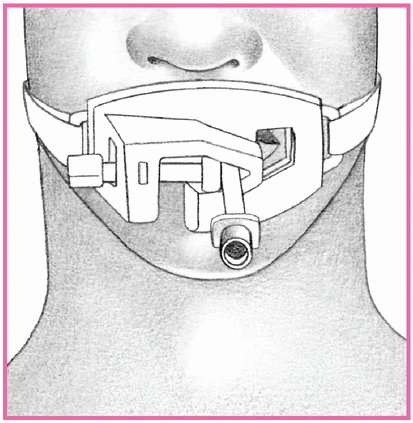
ET tube holders are available that can help secure an ET tube.
Made of hard plastic or of softer material, the tube holder secures the ET tube in place. The tube holder is available in adult and pediatric sizes. Some models come with bite blocks attached.
Place the strap around the patient’s neck and secure it around the tube with Velcro fasteners (as shown).
Because each model is different, check the manufacturer’s guidelines for correct placement and care.
|
The rim of the Easy Cap is divided into sections A, B, and C. Their control colors range from purple (in section A), signifying the absence of carbon dioxide (CO2), to beige, tan and, finally, yellow (in section C). The numbers in the sections range from 0.03 to 5 and indicate the percentage of exhaled CO2.
The color in the center rectangle reflects the patient’s CO2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree