Chapter 5 Treatment of Tracheobronchial Aspergillosis Superimposed on Post Tuberculosis–Related Tracheal Stricture
Case Description
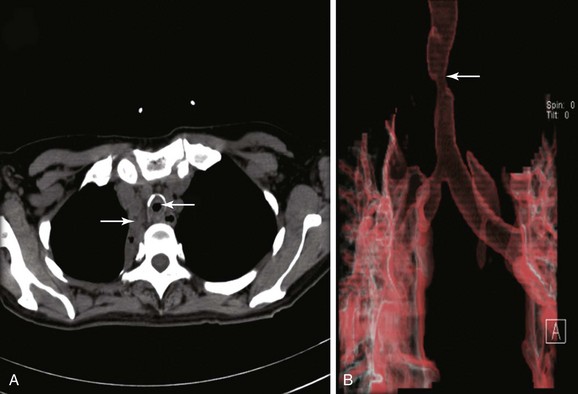
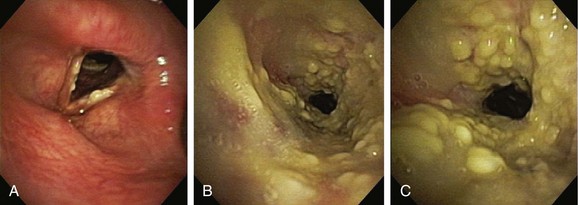
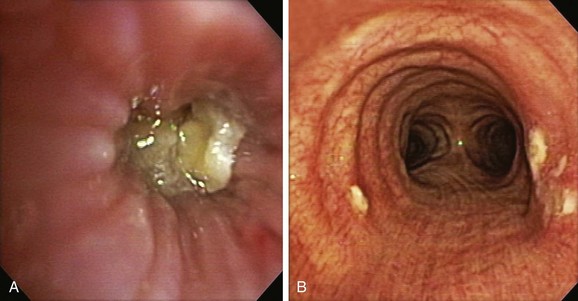
The patient was a 59-year-old female with a remote history of pulmonary tuberculosis with tracheobronchial involvement (details unknown). She had been appropriately treated with antituberculosis drugs for 9 months. Several years before our encounter, but well after her bout with tuberculosis, she had been diagnosed with asthma, but her dyspnea had never truly improved back to her baseline. Within the 2 weeks just before admission to our institution, she had increasing productive cough of yellowish-green sputum, dyspnea, fever with chills, and gradual hoarseness. She did not respond to a 2 week course of levofloxacin and prednisone (40 mg/day with tapering regimen). She was also using inhaled fluticasone 100 µg twice daily. The patient was hospitalized with severe respiratory distress and stridor suggestive of severe airway obstruction and then was transferred to our institution for further management when she developed worsening cough, dyspnea at rest, and complete loss of her voice. She was not married, was not a smoker, and had no other medical problems. Her wish was clearly to relieve the dyspnea and cough and return to work as an office manager. Physical examination revealed blood pressure of 168/86 mm Hg, heart rate of 110 bpm, temperature of 36.9° C, and respiratory rate of 22, along with saturation of 95% (room air). On chest examination, she had coarse breath sounds, wheezing bilaterally, and stridor over tracheal auscultation. Otherwise, her examination was normal. Initial laboratory data were unremarkable. Computed tomography (CT) with external three-dimensional reformation showed a 2 cm long, “hourglass”-shaped tracheal stenosis with a diameter of 7 mm (Figure 5-1). Complete atelectasis of the right upper lobe was noted (see Figure 5-1). Flexible bronchoscopy performed in the intensive care unit showed thick yellow material on the vocal cords and subglottis and white-yellowish pseudomembranes extending down the posterior membrane of the left main bronchus and on the spur of the left upper and left lower lobe bronchi. The right upper lobe bronchus was completely closed; this was probably a sequel of her tuberculosis. Bronchoscopy confirmed the location and degree of stenosis (Figure 5-2).
Discussion Points
1. List three differential diagnoses for the “pseudomembrane” pattern seen on bronchoscopy.
2. Describe the airway findings in acute tracheobronchial aspergillosis.
3. Describe some of the issues to be considered in cases of airway stent insertion in the setting of tracheal stenosis and concurrent active Aspergillus tracheobronchitis.
4. Describe the medical treatment of acute tracheobronchial aspergillosis.
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
This patient likely had infectious tracheobronchitis on a background of previous tracheal stenosis. In the setting of tracheal stenosis, mucosal inflammation associated with even mild respiratory tract infection can cause edema and mucus production, which may further occlude the lumen. In this patient, the presence of white-yellowish necrotic material was contributory to stenosis and likely was responsible for worsening symptoms. Without a confirmatory test such as CT or bronchoscopy, patients with previously undiagnosed tracheal stenosis and acute worsening due to respiratory tract infection may be misdiagnosed as having an exacerbation of chronic obstructive pulmonary disease or asthma. This is especially true when symptoms improve temporarily after therapy with antibiotics or corticosteroids because they reduce mucosal swelling and inflammation, thereby improving airway caliber. Recurrent or persistent symptoms minimally responsive or unresponsive to bronchodilators should raise suspicion for central airway obstruction before the development of critical stenosis requiring intensive care unit (ICU) admission.1
CT scanning* might thus be preferred for the initial evaluation of patients with suspected severe central airway narrowing to assess the length of the stenosis and the distal airways, which may not be accessible by flexible bronchoscopy in cases of severe airway lumen narrowing. In our patient, CT images quantified the degree of obstruction (i.e., severe, >70% reduction in cross-sectional area) and the extent of the narrowed tracheal segment (i.e., 2 cm), revealed the morphology of the stricture (i.e., hourglass), ruled out extrinsic compression as being responsible for the tracheal narrowing, and revealed other associated parenchymal findings (e.g., right upper lobe [RUL] atelectasis). CT is preferably performed before bronchoscopy because it might guide additional diagnostic procedures when parenchymal abnormalities or mediastinal lymphadenopathy is present. However, CT does not offer information about mucosal abnormalities that can be detected only on bronchoscopy (e.g., pseudomembranous tracheobronchitis).
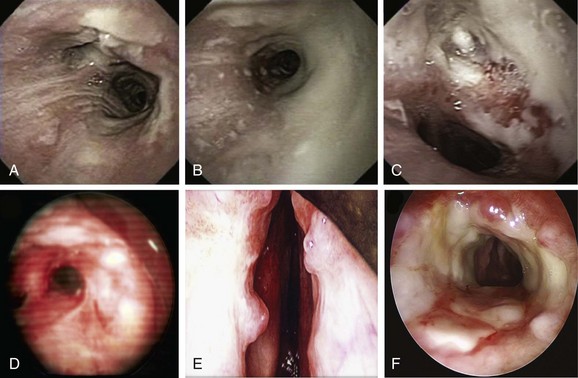
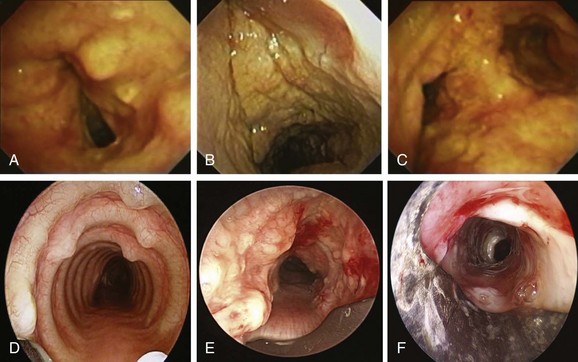
Given the frail status of this patient, bronchoscopy was performed in the ICU. We were prepared to endotracheally intubate and stabilize her airway had she developed worsening respiratory failure during or after the procedure. To avoid a decrease in respiratory drive and potential hypercarbic respiratory failure, bronchoscopy was performed with only local laryngeal analgesia.* Bronchoscopy revealed large, “cheese-like,” white-yellowish necrotic pseudomembranes on a background of hourglass (funnel-shaped) tracheal stenosis (see Figure 5-2). This type of mucosal abnormality can be seen in patients with mycobacterial or fungal infection, including tuberculosis, aspergillosis, candidiasis, mucormycosis, Pseudallescheria boydii, and Scedosporium prolificans (Figure 5-3)2; in addition, necrotizing bacterial tracheobronchitis, severe smoke inhalation injury with superimposed infection, infiltrating adenocarcinoma, and sometimes aggressive active tracheobronchial Wegener’s granulomatosis or radiation tracheatis present in a similar fashion (Figure 5-4).3,4 Awareness of these diagnoses is important when approaching a patient with pseudomembranous tracheobronchitis because airway biopsies are necessary to confirm most of these disorders, and treatments are disease specific.
This pseudomembranous pattern of airway mucosa in fact is commonly seen in the actively caseating type of endobronchial tuberculosis (TB).* This form of TB appears to be highly contagious, with a reported rate of AFB sputum positivity that exceeds 50%.5 In addition to this actively caseating form of endobronchial TB, a bronchitic type identified as airway erythema and edema, a granular type with associated submucosal tubercle formation, a mucosal ulcerative type, an edematous-hyperemic type with significant mucosal inflammation and bronchial narrowing, and a fibrostenotic type causing cicatricial airway strictures may occur.5 It is unclear whether true stepwise progression occurs from one type to another, or whether each particular type may occur independently without required passage through the other histopathologic forms.5 Given her history of tuberculosis with airway involvement, we believe that our patient had developed acute infection on a background of post tuberculosis fibrostenotic stricture.
Aspergillus tracheobronchitis is an uncommon but well-described manifestation of Aspergillus infection, occurring in less than 7% of patients with pulmonary aspergillosis.6,7 Three types of tracheobronchial aspergillosis have been identified on the basis of bronchoscopic pattern: obstructive, ulcerative, and pseudomembranous. The obstructive type is characterized by thick mucus plugs without gross evidence of bronchial inflammation.8 The ulcerative type has plaque-like inflammatory lesions (Figure 5-5). The pseudomembranous type is characterized by extensive inflammation with formation of a pseudomembrane overlying the mucosa and containing Aspergillus organisms.9 This type is most prevalent in immunocompromised patients,8 is diagnosed by evidence of Aspergillus on microscopic specimens of material obtained at bronchoscopy, and has been reported to be refractory to antifungal therapy.9
Other differential diagnoses of diffuse infiltrating white-yellowish central airway lesions may include amyloidosis, infiltrating adenocarcinoma, tracheobronchial amyloidosis, atypical forms of tracheopathica osteochondroplastica, and rhinoscleroma. Amyloidosis is caused by overexpression and extracellular deposition of specific proteins.*10 Airway involvement in amyloidosis (AL) is seen with the AL type in which the specific protein deposition comprises κ and λ light chains of monoclonal immunoglobulins. Women are affected earlier (52 vs. 59 years of age), slightly more often (10 : 9 ratio), and more extensively than men, and cough, wheezing, dyspnea, and occasionally hemoptysis are the usual symptoms that precede histologic diagnosis by an average of 17 months.11 In fact, patients are often treated before diagnosis for recurrent pneumonia, tracheobronchitis, or asthma. At bronchoscopy, two patterns of amyloid deposition are described: a nodular or unifocal disease, and a diffuse submucosal disease (see Figure 5-4).†12 Low-dose external beam radiation is a reported treatment alternative‡13; however, excisional therapy is the standard treatment for upper and central airway amyloidosis, which may often progress to respiratory failure. Frequent laser excisions (≈5 treatments/yr) sometimes are necessary. In some nodular forms of tracheobronchial amyloidosis, neodymium-doped yttrium aluminum garnet (Nd:YAG) laser treatment removes tissue and eliminates further amyloid deposition in the field. However, the diffuse form usually recurs after laser treatment, and repeated rigid laser bronchoscopies denude airways and promote collagen scar formation. Repeated airway debridement may trade one obstructing disease (amyloidosis) for another (scar stenosis).
Tracheopathica osteochondroplastica (TPO) is another rare nonmalignant disorder of the central airways characterized by multiple dense nodules localized in the submucosa of the tracheobronchial wall.*14,15 TPO is a slowly progressive disease of adulthood with a mean time from presentation to diagnosis of approximately 4 years; it is usually detected incidentally upon intubation, or when CT or bronchoscopy is performed for airway symptoms or for unrelated conditions.16,17 Although TPO may involve the larynx, the disease is usually limited to the central airways (trachea and mainstem bronchi) and does not involve the lung parenchyma or other organs. Mucosal changes (edema, hyperemia), impaired clearance of secretions, and enlarged submucosal nodules may lead to recurrent inflammation, infection, and central airway obstruction. Cough, hoarseness, exertional dyspnea, wheezing, and recurrent lower airway infections are the usual symptoms, and stridor and rhonchi are present in advanced obstructive cases, which can even lead to respiratory failure.14 The disease is usually distinguishable from other disorders, however, because it does not involve the posterior membranous portion of the trachea. In addition, bronchoscopy findings are often considered to be characteristic when focal or diffuse raised, firm nodules overlying the cartilaginous rings are noted (see Figure 5-4).15 Occasionally, however, atypical irregular nodules† and mucosal inflammation may mimic carcinoma or airway infection.15 Although no obvious relationship to malignancy has been noted, a large case series showed that 24 (19%) of 126 patients had associated cancers, especially bronchogenic adenocarcinoma.18 For this reason, bronchoscopic biopsies may still be needed.
Infiltrated tracheobronchial wall by diffuse polypoid lesions covered with thick white secretions, bulging into and narrowing the lumen, can be seen with a chronic, slowly progressive, infectious disease of the respiratory tract caused by the bacterium Klebsiella rhinoscleromatis, a subspecies of Klebsiella pneumoniae that has special affinity for the nasal mucosa.19 In many patients, the disease process (aka scleroma) remains confined to the nasal cavity (thus the name rhinoscleroma), but involvement of other parts of the respiratory tract has been reported (see Figure 5-3). The presentation, similar to that of our patient, is nonspecific and includes chronic productive cough, stridor, and dysphonia.*20,21 The incidence of laryngeal involvement in rhinoscleroma varies between 15% and 80%, but tracheobronchial involvement is far less common. A report from the United States showed that 13 of 22 patients with rhinoscleroma had laryngotracheal disease; of these, 9 had subglottic stenosis and/or glottic stenosis, and only 2 had tracheal involvement limited to the first two tracheal rings.22 In a different study of 56 patients, the nose was affected in 100% of patients; other affected regions were nasopharynx in 13 patients, palate in 7 patients, skin in 2 patients, larynx in 3 patients, trachea in 17 patients, nasolacrimal duct in 2 patients, and premaxilla in 1 patient.21 Given its geographic prevalence in Central America, the Middle East, and central Europe, and its usual nasal involvement, rhinoscleroma was unlikely in our patient. Biopsies are warranted because Gram stains will identify tiny bacilli consistent with K. rhinoscleromatis in the cell cytoplasm.21
Patient Preferences and Expectations
The patient shared with us her emotions and expressed her wish to breathe better so she could go back to work. She desired to stay active and independent. She had no close friends or family, and she did not feel comfortable sharing her illness with her few acquaintances from work. She shared with us her concern that she would lose her job because of her breathing problems and frequent absences. Furthermore, she was terrified by the thought that without a job she would surely lose her insurance and would not be able to undergo further treatment. We made a treatment plan together by deciding to initially determine the exact cause of her problem and to alleviate dyspnea by performing rigid bronchoscopic dilation. We explained that the treating team works to provide care to all individuals, regardless of their socioeconomic status, and that from a medical ethics perspective, we believe that as human beings we are all valuable social entities who have the right, not the privilege, to health care access.23 From a pragmatic standpoint, however, we referred her to a case manager to discuss additional medical insurance options.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree