4 Transthoracic and Transesophageal Echocardiography in the Catheterization Laboratory
Alcohol Septal Ablation
Background
• In the setting of hypertrophic obstructive cardiomyopathy (HOCM), transcoronary alcohol septal ablation by injection of ethanol into the septal perforator supplying the muscle mass adjacent to the point of mitral leaflet-septal contact widens the outflow tract and relieves the obstruction.
Preprocedural Anatomic and Physiologic Imaging
• Confirm left ventricular (LV) anatomy and function:
• Perform routine transthoracic imaging to exclude atypical forms of hypertrophic cardiomyopathy as well as fixed left ventricular outflow tract (LVOT) obstruction.
• Confirm mitral valve (MV) anatomy and function:
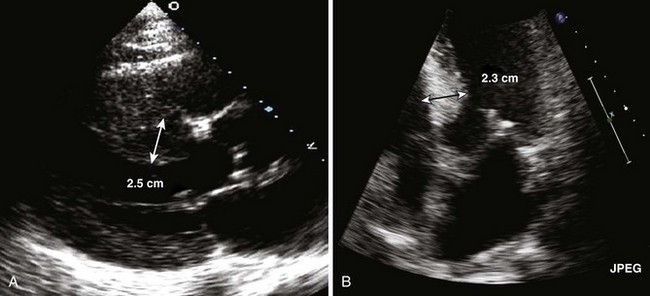
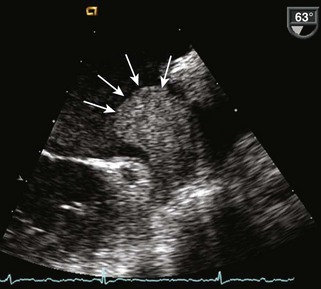
• Document systolic anterior motion (SAM) of the mitral leaflet with proximal MV-septal contact (Fig. 4-2).
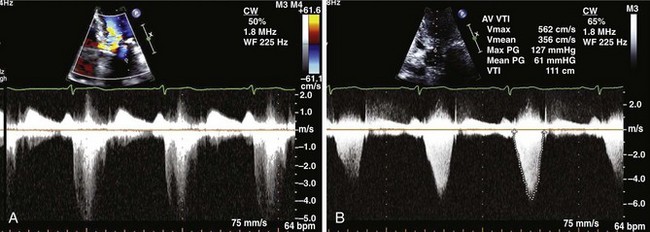
• Determine the subaortic gradient:
Pitfalls
• RV trabeculations merging with the septum should not be included in measurements of the interventricular septum. Low parasternal views are particularly prone to this type of error. If in doubt, angulation of the imaging plane will help demonstrate the plane separating such trabeculations from the septum.
• When endocardial borders are not well imaged, consider using intravenous contrast agents for LV opacification to confirm ventricular anatomy. The apex may be particularly difficult to image.
• Congenital abnormalities of the mitral apparatus (anomalous papillary muscle insertion or malpositioned enlarged papillary muscles) produce more distal muscular obstruction in the mid-cavity. These lesions are not candidates for ablation.
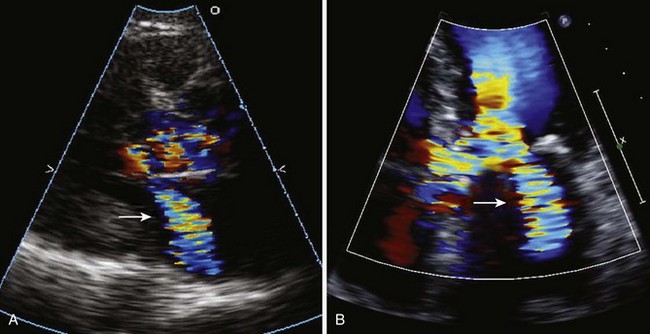
• Avoid contamination of the subaortic spectral Doppler with MR.
• Both MR and LVOT velocities may appear to peak late given the anatomy; however, the duration of MR is typically greater than the duration of systolic ejection (Fig. 4-4).
Intraprocedural Anatomic and Physiologic Imaging
• Identification of the appropriate septal perforator:
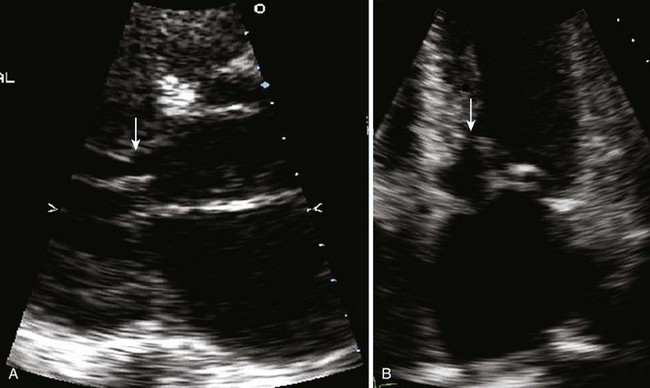
• Balloon occlusion followed by myocardial contrast injection directly into the septal perforator by the angiographer should be performed during continuous transthoracic echocardiographic (TTE) or transesophageal echocardiographic (TEE) imaging.
• Injection of alcohol with limited myocardial infarction:
• Apical four- or five-chamber views are continuously imaged during and following injection of alcohol.
Pitfalls
• The selected septal perforator must perfuse the region of the septum in contact with the MV during SAM but should not perfuse other distant regions of the LV or RV myocardium or papillary muscles.
• Approximately 15% to 20% of patients will not have a successful procedure due to lack of suitable septal arteries in the region of obstruction.
Postprocedural Imaging
• Confirm LV anatomy and function:
• Image basal septum from parasternal and apical views concentrating on septal anatomy following controlled infarction.
• Measure the septal thickness in the region of infarction and, if different, in the region of mitral-to-septal contact.
• Color Doppler imaging to exclude perforation (ventricular septal defect) should include the RV side of the septum.
Key Points
• Confirm LV anatomy (increased basal septal wall thickness) and MV anatomy (SAM) with documentation of a resting or provoked gradient of >50 mm Hg arising from septal-MV contact.
• Identify appropriate septal perforator supplying the region of septal-MV contact using direct injection of myocardial contrast and imaging the hyperechoic region of the septum.
Percutaneous Balloon Mitral Valvuloplasty
Background
• Since the advent of percutaneous balloon mitral valvuloplasty (PBMV) in 1984, the technique has become the treatment of choice for mitral stenosis (MS); it is as effective as open valvotomy and more effective than closed valvotomy. Echocardiographic assessment is essential in patient selection, intraprocedural monitoring, and postprocedural follow-up.
Preprocedural Imaging
• Assess severity and level of MV obstruction.
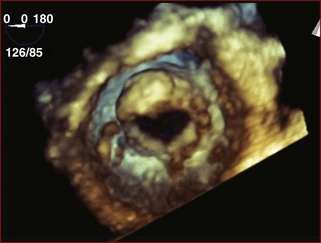
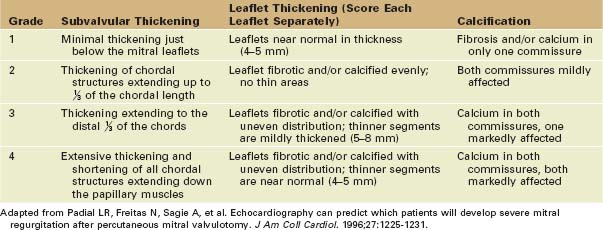
• Apply the Wilkins Echo Score to predict outcome of valvuloplasty (Table 4-1).
• In Wilkins’ original report,1 patients with a score of less than or equal to 8 were more likely to have optimal results following valvuloplasty (post mitral valve area [MVA] >1.5 cm2, left atrial pressure [LAP] <18 mm Hg). Patients with a score of greater than 8 had suboptimal outcomes, and a score of greater than 10 increased the chance of suboptimal results with complications.
• Assess presence of intracardiac thrombus.
TABLE 4-1 THE MV SCORE HELPS PREDICT PERCUTANEOUS BALLOON MITRAL VALVULOPLASTY SUCCESS BY GRADING FOUR CHARACTERISTICS OF THE MV APPARATUS
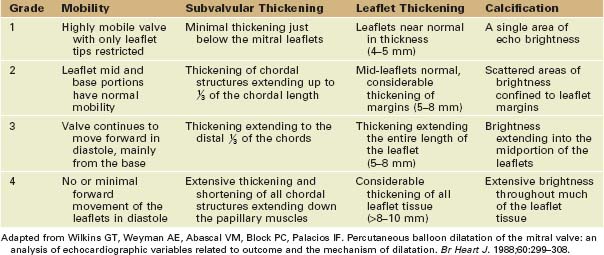
TABLE 4-2 FURTHER SCORING OF THE MV HELPS PREDICT THE OCCURRENCE OF THE PRIMARY COMPLICATION OF PBMV, MITRAL REGURGITATION
Pitfalls
• Pressure half-time calculation of valve area has numerous limitations and should be used with caution in older patients, in atrial fibrillation, and in patients with prior MV interventions. An integrative approach to calculating valve area is always recommended.
• Peak and mean gradients are closely related to the amount of diastolic flow across the valve and the diastolic filling period and should be interpreted in relation to heart rate.
• Patients with degenerative MS (calcification of the annulus or body of the leaflets with little or no commissural fusion) should not undergo PBMV.
Intraprocedural Imaging
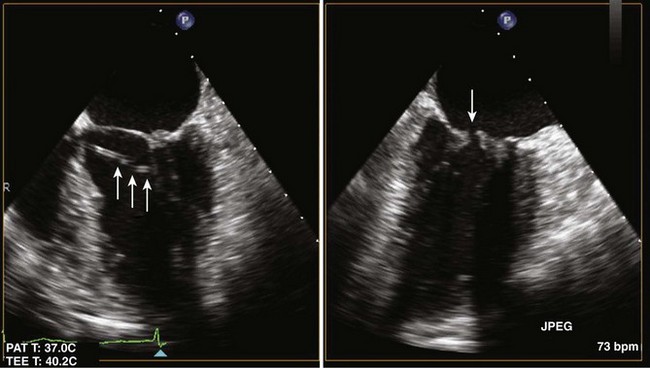
• Transseptal puncture: although typically interventionalists can perform the transseptal puncture under fluoroscopy, occasionally TEE can help interventionalists position the puncture to avoid puncture of the aorta or atrial wall.
• Assessing postvalvuloplasty results by TTE:
• After each balloon inflation, imaging should be performed to assess MR severity, peak and mean transmitral gradients, and MV area by planimetry.
• A suboptimal valvuloplasty result is defined as a final valve area of less than 1.0 cm2, a final transmitral mean pressure gradient greater than 10 mm Hg, or a less than 25% increase in valve area.
• In some cases, intracardiac echocardiography or TEE imaging (see Fig. 4-8) may be utilized to assess MV area.
Percutaneous Valves: Transcatheter Aortic Valve Implantation
Background
• Transcatheter aortic valve implantation (TAVI) has been shown to be superior to medical therapy in a population of patients with severe, symptomatic aortic stenosis at prohibitive risk for surgery.2
• Because echocardiography has largely replaced the invasive assessment of aortic stenosis, it is a necessary tool in the preprocedural, intraprocedural, and postprocedural evaluation of patients undergoing transcatheter valve procedures.
• Because the experience in the United States has to date been limited to the balloon expandable valve, the current review will outline the approach to preprocedural, intraprocedural, and postprocedural echocardiographic assessment of candidates for TAVI with the balloon expandable valve. Both the balloon expandable and a self-expanding valve are commercially available in Europe.
Preimplantation Echocardiographic Imaging for TAVI (Box 4-1)
• Measure the LVOT diameter in systole:
• The LVOT diameter should be measured from parasternal long axis views in systole
• The diameter is measured in parasternal long axis view typically between the annulus and 0.5 cm apical to the aortic annulus in systole. The long axis view is used to measure the diameter of the LVOT since the septum and anterior leaflet of the MV are most parallel in this view; apical views should not be used.