From Yang YJ, Kandzari DE, Gao Z, et al. Transradial versus transfemoral method of percutaneous coronary revascularization for unprotected left main coronary artery disease: comparison of procedural and late-term outcomes. JACC Cardiovasc Interv. 2010;3:1035–1042.
Among TR bifurcation cases treated with a two-stent technique (N = 67, 19%), bifurcation stent technique included stepped crush (72%), T-stenting (22%), and culotte (6%). In this study, all TR cases were performed using a 6F guiding catheter, an observation consistent with other nonleft main TR trials. In the RIVAL (RadIal Vs femorAL access for coronary intervention trial) study, for instance, PCI using a ≥7F guiding catheter occurred in only 1% (35/3,507) of cases.43 Nevertheless, transradial PCI using ≥7F guiding catheters and larger-caliber sheathless guiding catheters that permit simultaneous two-stent techniques have also been described.44,45 In contrast to a TR access method, the use of hemodynamic support and IVUS were more common with TF PCI. Despite such differences, left main-specific angiographic and procedural success rates were very high in each cohort and were similar between treatment strategies.
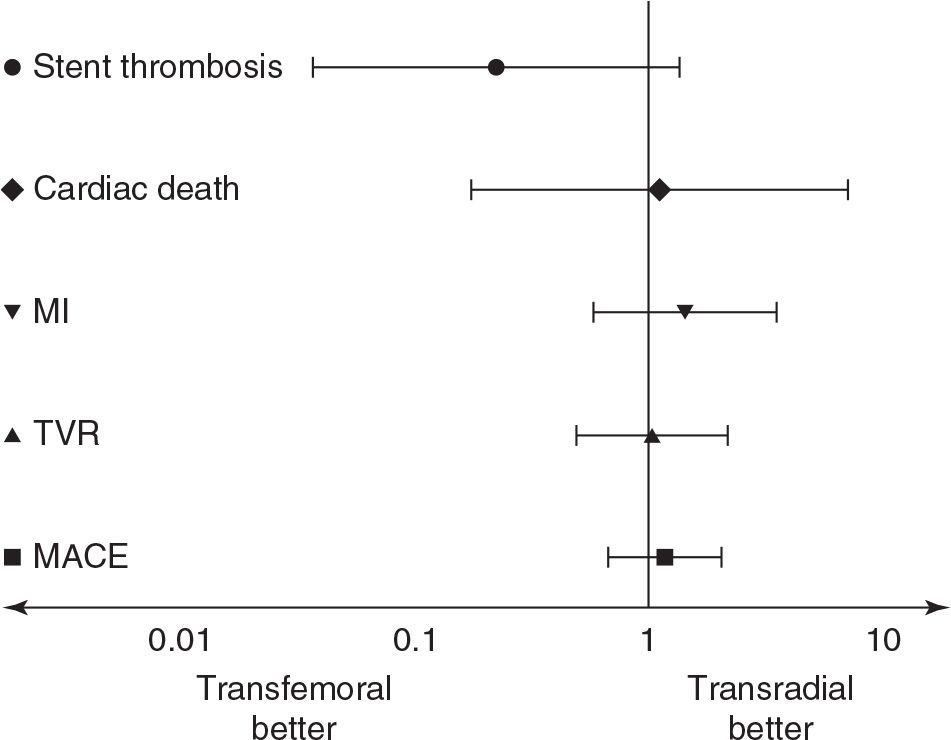
FIGURE 19-1 Multivariable matched propensity analysis of major adverse events following transradial or transfemoral unprotected left main PCI. (From Yang YJ, Kandzari DE, Gao Z, et al. Transradial versus transfemoral method of percutaneous coronary revascularization for unprotected left main coronary artery disease: comparison of procedural and late-term outcomes. JACC Cardiovasc Interv. 2010;3:1035–1042.)
Conclusion
Evidence from clinical trials of varied design and size consistently support the consideration of ULM PCI as an alternative revascularization strategy to CABG in selected patients. In particular, trials reporting late-term safety outcomes of cardiovascular death, myocardial infarction, and stroke comparable to CABG have fostered renewed enthusiasm for ULM PCI. Forthcoming trials designed with careful attention to patient selection, timing of end-point ascertainment, and relevance of safety and efficacy end points should inform clinical decision making and treatment guidelines.
In parallel, application of DES and advances in technique and strategy have enhanced the rates of early procedural and long-term clinical success of ULM PCI. However, although several studies have demonstrated the superiority of TR vascular access compared with a TF approach for reductions in vascular access and bleeding complications, expansion of TR PCI to more high-risk and complex coronary anatomy has been limited by lack of evidence and operator inexperience. Specific to ULM PCI, perceptions related to the challenges of guiding catheter support, equipment limitations, and consequences of procedural failure have challenged the advancement of TR vascular access in this indication.
More recently, our understanding of a TR strategy versus TF vascular access has advanced specifically in ULM PCI. Percutaneous ULM revascularization, including the treatment of distal bifurcation disease, is feasible by the TR method and is associated with high procedural success. Bleeding events are significantly less common with ULM TR PCI compared with TF, and hospital stay is abbreviated. Finally, TR PCI for ULM disease is associated with similar early and late outcomes of major cardiovascular events compared with TF access.
Altogether, these findings are consistent with other studies not only comparing vascular access methods for PCI but also ULM PCI in general. Altogether, favorable outcomes with ULM PCI reported in recent large observational studies may be attributed to technique, including high stent deployment pressure, kissing balloon postdilation, and the use of IVUS guidance, all of which are feasible with TR PCI. These results not only inform our understanding of TR PCI in more challenging and complex coronary anatomy, but also add to the evidence associating TR PCI with reduced bleeding events and yet similar procedural and clinical efficacy compared with TF vascular access.
REFERENCES
1. Mann T, Cubeddu G, Bowen J, et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J Am Coll Cardiol. 1998;32:572–576.
2. Kiemeneij F, Laarman GJ, Odekerken D, et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269–1275.
3. Mann T, Cowper PA, Peterson ED, et al. Transradial coronary stenting: comparison with femoral access closed with an arterial suture device. Catheter Cardiovasc Interv. 2000;49:150–156.
4. Jolly SS, Amlani S, Hamon M, et al. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–140.
5. Chase AJ, Fretz EB, Warburton WP, et al. Association of the arterial access site at angioplasty with transfusion and mortality: the M.O.R.T.A.L study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart. 2008;94:1019–1025.
6. Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv. 2009;2:1047–1054.
7. Rao SV, Ou F, Wang TY, et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


