FIGURE 27-1 MitraClip procedure with a single venous access in the right groin, and right radial access for arterial pressure monitoring. A: Sheaths inserted just prior to procedure. B: Six hours postprocedure, showing no vascular issues in the groin or forearm.
A similar approach can be used during percutaneous mitral valvuloplasty. A 4F pigtail catheter is advanced into the left ventricle via the right radial artery. The Swan Ganz catheter is advanced via the right jugular vein for measurements of right heart pressures and cardiac output assessment. Right heart catheterization can also be performed using the basilic or cephalic veins (see Chapter 13). The therapeutic valvuloplasty catheter is advanced through the right femoral vein. Such an approach allows for no catheters to be placed in the other groin and minimizes the vascular complications and allows early mobilization of the patient (Fig. 27-2).
Transradial Catheterization during Aortic Valve Procedures
Over the past decade the technique of transcatheter aortic valve implantation (TAVI) has been embraced as a novel treatment option for inoperable or high-surgical-risk patients with severe symptomatic aortic valve disease. Recent randomized studies have raised major safety concerns because of increased stroke/transient ischemic attack rates with TAVI than with medical treatment and conventional aortic valve replacement. The pathophysiology of ischemic brain defects after TAVI is multifactorial. In addition to intrinsic patient characteristics such as age, previous stroke, atrial fibrillation, and left ventricular dysfunction, mobilization of atherosclerotic material by wire and catheter manipulations or calcified valve particles during balloon valvuloplasty or actual bioprosthesis implantation, as well as hypotension and cerebral hypoperfusion from intraprocedural tachy-pacing maneuvers during valve deployment, especially in patients with carotid disease, could also contribute toward the TAVI-associated stroke risk.6 Embolic protection devices have been developed to reduce these events. Three different devices have been used in experimental studies to reduce the TAVI-associated stroke risk. In general, these devices use two different mechanisms of protection (capture versus deflection of the embolic material). Two of these technologies, the Claret CE Pro system (Claret Medical Inc., Santa Rosa, CA) and the Embrella (Edwards Lifesciences, Irvine, CA), are temporarily introduced via right TR or transbrachial access into the supra-aortic arteries. The SMT-Shimon Embolic protection Filter, or SHEF (SMT Medical, Herzliya Pituach, Israel), which is an embolic deflection device, requires femoral arterial access via a 9F sheath. The Claret CE ProTandem Embolic Protection Device consists of two filter baskets attached in series that capture embolic material during the procedure. This device is 6F compatible and is introduced via the right TR or transbrachial access. The proximal filter is deployed first in the truncus brachiocephalicus for the protection of the right vertebral artery as well as the right common carotid artery, followed by the distal filter in the left common carotid artery. Although there was not a systematic magnetic resonance neuroimaging at baseline and follow-up to discover new TAVI-related brain lesions, in the first-in-human experience of the Claret CE Pro system the proof of concept was at least partly illustrated by the capturing of debris in more than half of the patients, providing evidence for the potential to reduce the procedural cerebral embolic burden utilizing this dedicated filter system during TAVI.7 The Embrella Embolic Deflector Device contains a self-expanding nitinol frame with a heparin-coated polyurethane porous membrane that does not interfere with cerebral perfusion. The system is 6F compatible and is introduced through radial or brachial access over the right side of TAVI patients. The device is designed to cover the ostia of the brachiocephalic trunk (and its right carotid branch) and the left carotid artery originating directly from the transverse aorta, thereby deflecting emboli away from the cerebral circulation. In some patients, the device might also overlie the left subclavian ostium, providing protection for the left vertebral. Because the device is not positioned within the cerebral vessels, the risk of arterial spasm, injury, thrombosis, or transiently impaired cerebral perfusion seems minimal.8
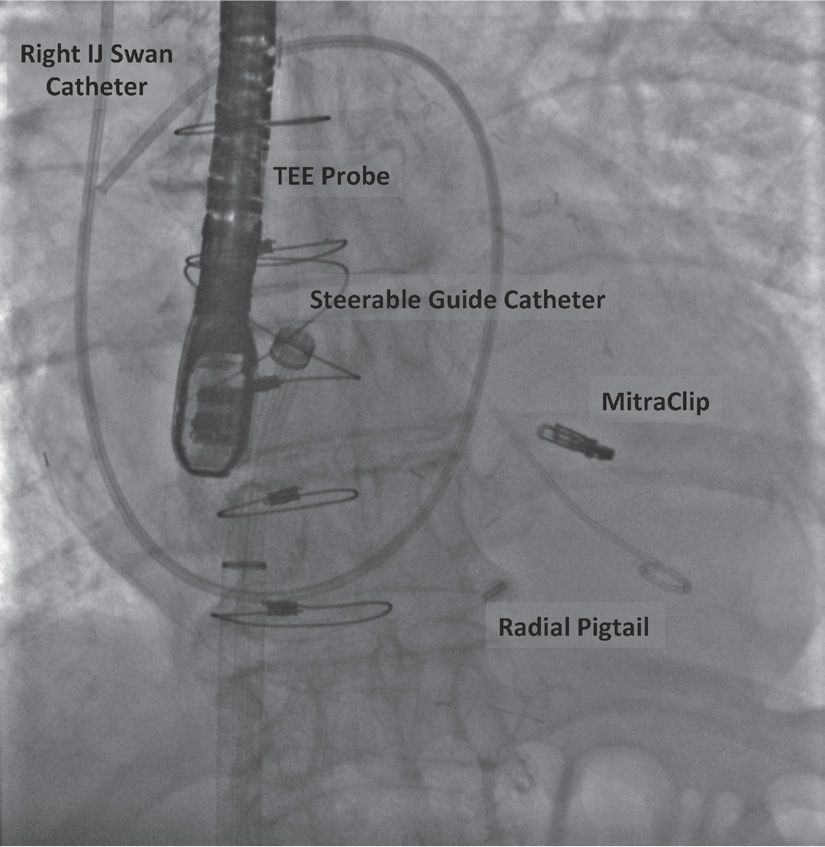
FIGURE 27-2 Fluoroscopic image of a MitraClip showing the use of pigtail catheter inserted via the right radial artery.
Post-TAVI cases of complex PCI for coronary obstructions, jailed left main or new coronary artery lesions have been described.9 Although some cases have been performed by radial approach, the exact benefit of this access has not yet been studied in detail.10
Interestingly, the group of Dr. A. Colombo has also described the radial crossover techniques for secured femoral access management during TAVI procedures.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


