FIGURE 16-1 Different angles between distal subclavian and internal mammary arteries and different catheter selection according to the access route (three-dimensional right catheter for radial one vs IM catheter for femoral one).
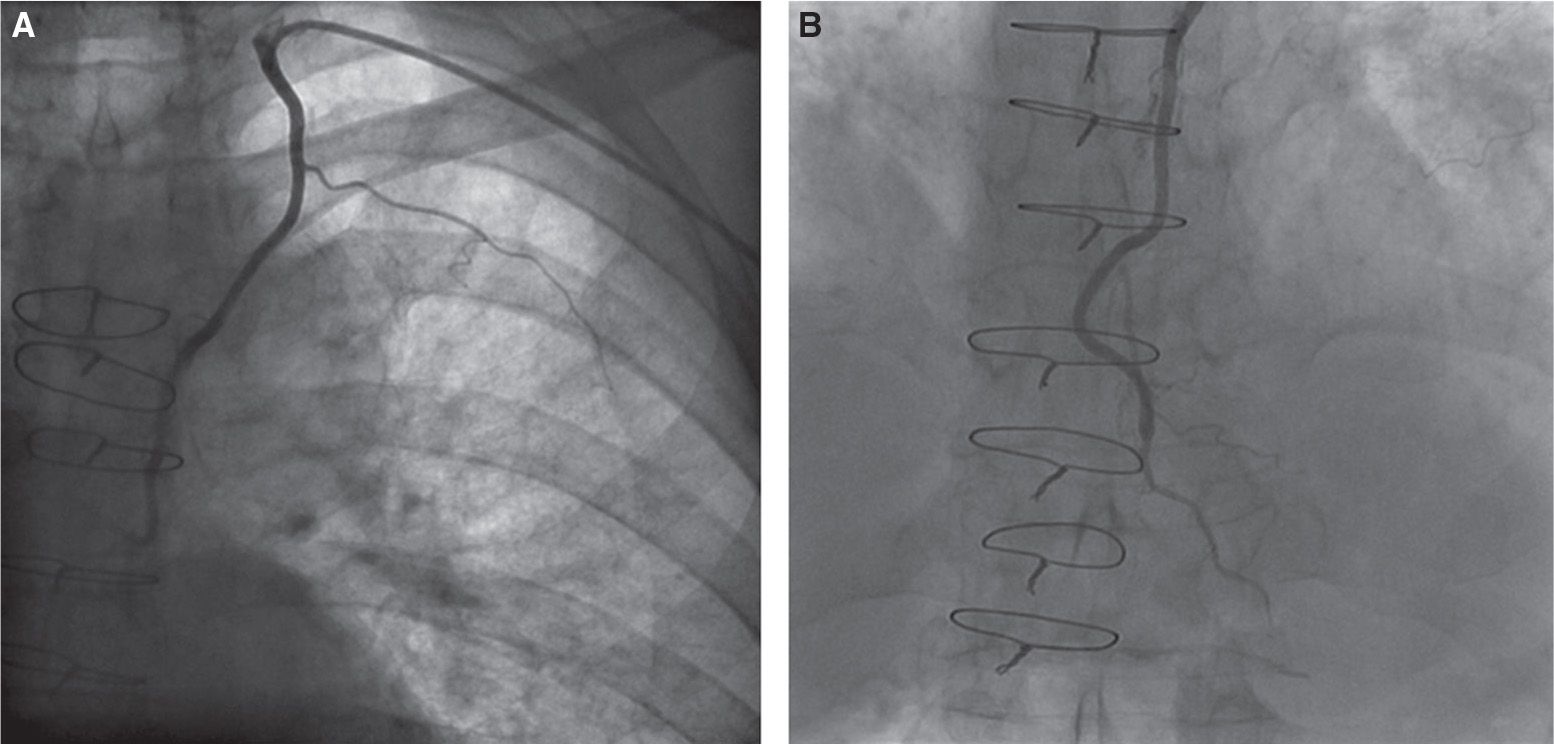
FIGURE 16-2 Selective angiography of left internal mammary artery graft to left anterior descending performed by left radial approach using three-dimensional right catheter (A, B).
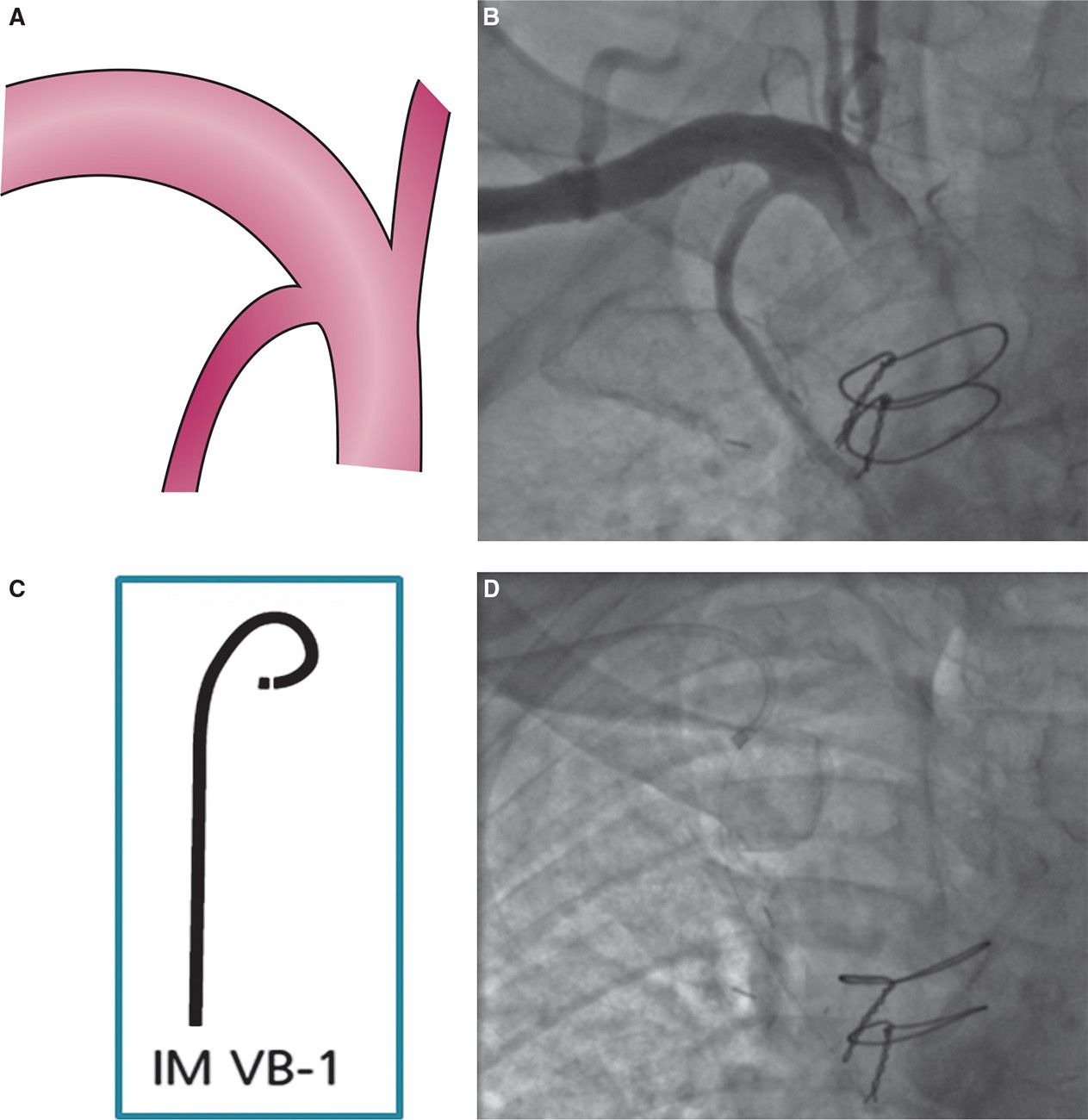
FIGURE 16-3 In rare cases of horizontal internal mammary artery take-off from a “vertical” segment of subclavian artery (more frequent for right mammary artery) (A, B), IM-VB1 catheter may be useful from homolateral radial approach (C, D).
Contralateral Transradial Approach in Patients with Internal Mammary Graft
Preliminary Remarks
In patients with double IMA conduit usage during surgical revascularization, selective angiography of grafts is usually performed by TFA. Indeed, while selection of bilateral radial arterial access is poorly desirable, selective cannulation of IMA from contralateral TRA brings about technical troubles due to high frictions and multiple angulations—without adequate support—which often hamper catheter advancement into the contralateral subclavian artery.
While selecting contralateral TRA in patients with double IMA grafts, it should be taken into account that, even in skilled hands, unselective IMA angiography is sometimes the best achievable result.17
Techniques for Cannulation
If TRA is selected, bilateral radial arterial access or single radial approach may be used; in the latter case, it is preferable to select the right radial approach, as left IMA cannulation by the contralateral radial access has been previously described.18–25 The first step is the achievement of subclavian artery cannulation; aortic arch and/or subclavian artery angiography are sometimes useful to choose the appropriate catheters. Different catheters are often necessary to cannulate the opposite subclavian artery and then (after 0.25-inch-long wire catheter exchange) the IMA. The Judkins left, left coronary bypass (LCB), or Tiger (Terumo, Tokyo, Japan) diagnostic catheters can be used to pass the exchange-length wire through the aortic arch to gain the contralateral subclavian artery; after advancement of the wire as far as possible down to the arm, the Judkins left catheter is exchanged for an IM or JR4 catheter22 (Fig. 16-4). The Simmons catheter has been specifically used for left IMA cannulation by right radial approach, with 89% of selective cannulation rate18; moreover, a dedicated catheter curve—Yumiko catheter (Goodman, Japan), a modified version of Simmons catheter with an atraumatic soft tip—has been realized.19
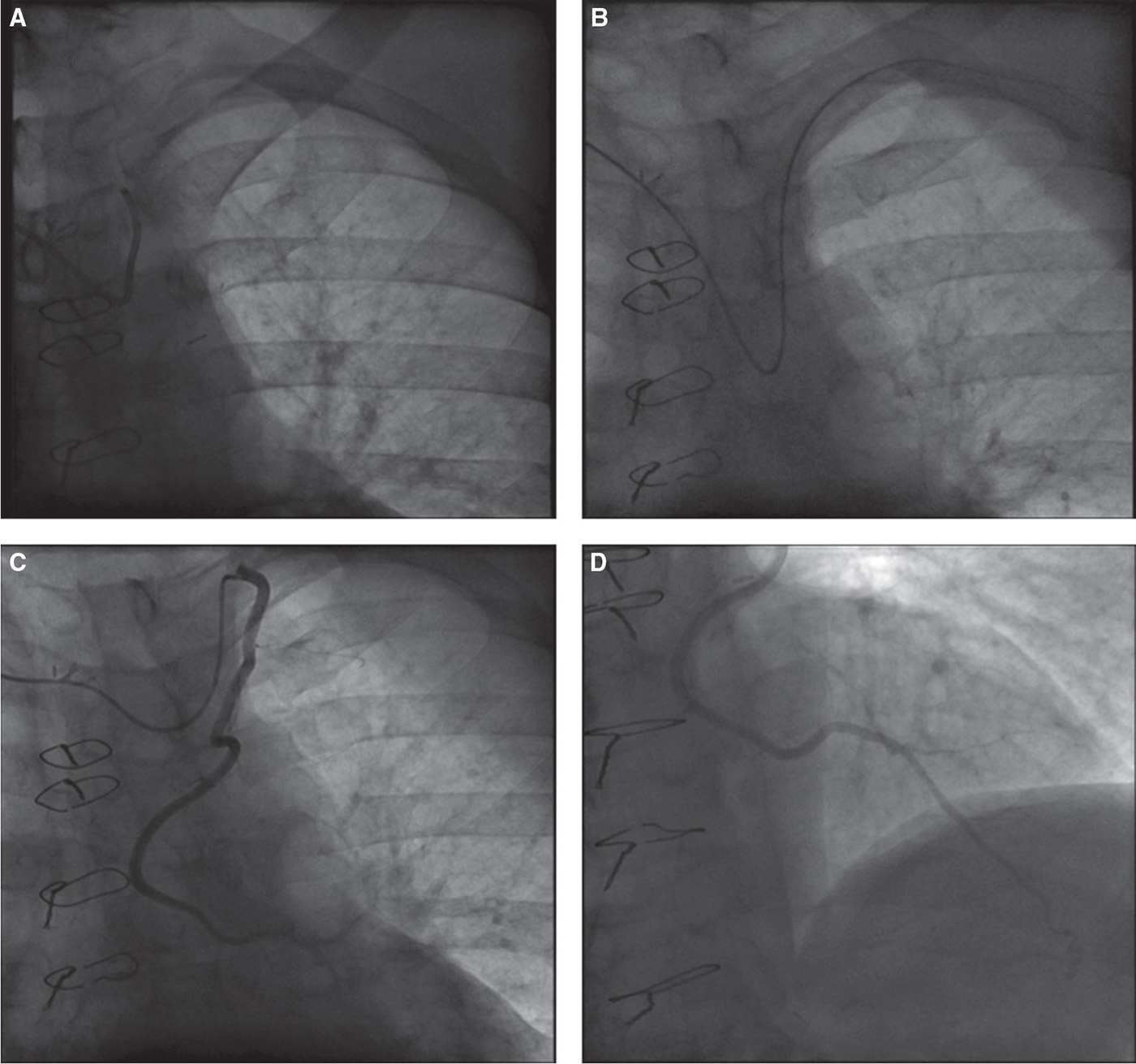
FIGURE 16-4 Cannulation of left IMA graft to left anterior descending from right radial approach. The Judkins left diagnostic catheter is used to pass the exchange-length wire through the aortic arch, gaining the contralateral subclavian artery (A, B); then, the Judkins left catheter is exchanged for a JR4 catheter for selective engagement of left IMA (C, D).
When catheter advancement is particularly challenging, support and stabilization of the wire in the contralateral brachial artery may be obtained by trapping the exchange-length wire in the arm by external compression (either manually or by using an inflated blood pressure cuff) or by elbow flexion.25
Aorto-coronary Grafts
Aorto-coronary grafts have been for years the only type of graft performed during surgical revascularizations and are still contemporarily used. The vast majority of aorto-coronary grafts are SVGs. The reason for referral to coronary angiography is often due to the accelerated degenerative process involving SVGs, so that the clinical suspicion of their failure is high26; when this suspicion is confirmed, in many cases PCI of the degenerated graft is necessary. Thus, obtaining a very high backup support by selecting the appropriate guiding catheter shape may be a key factor for a successful transradial PCI in patients with complex SVG lesions.
Transradial Approach in Patients with Saphenous Vein Grafts
Preliminary Remarks
Owing to the highly variable location within the supra-bulbar ascending aorta of proximal aortic anastomoses of SVGs (according to the technique and the preference of the surgeons), the variability of catheter curves needed to engage the SVG ostium is probably higher was coming from the RA than from the femoral one. In the above-mentioned comparative study between TRA and TFA for CABG patients, the higher the number of SVGs to be assessed, the higher was the additional time needed for their cannulation by TRA.13 According to our experience, ascending aorta angiography may be advisable when more than two SVGs have to be studied and whenever difficulties are encountered for their localization.
Techniques for Cannulation
The multipurpose or the Judkins right catheters are usually selected to cannulate SVGs originating from the right side of the ascending aorta (generally SVG to the right coronary artery) (Figs. 16-5 and 16-6); the efficacy of their curves is smaller from right than from left TRA. Moreover, the right side of the aorta immediately proximal to the anonymous trunk origin is a “black zone” difficult to be explored by right TRA. Such area, represented in black in Figure 16-5, is an infrequent but troublesome location for proximal SVG anastomosis, and should be taken into account while selecting the radial approach side. When this “black zone” is explored by right TRA, unusual guiding catheter curve selections and manipulations may be useful (e.g., Hockey Stick catheter or Voda left 3 rotated with a 0.35-inch wire inside).
Out of the right side of the ascending aorta SVG engagement is usually achieved by the Amplatz left curves (Figs. 16-5 and 16-6). Moreover, pullback of the Judkins left may be successfully used for the cannulation of SVGs located in the left side of the ascending aorta.
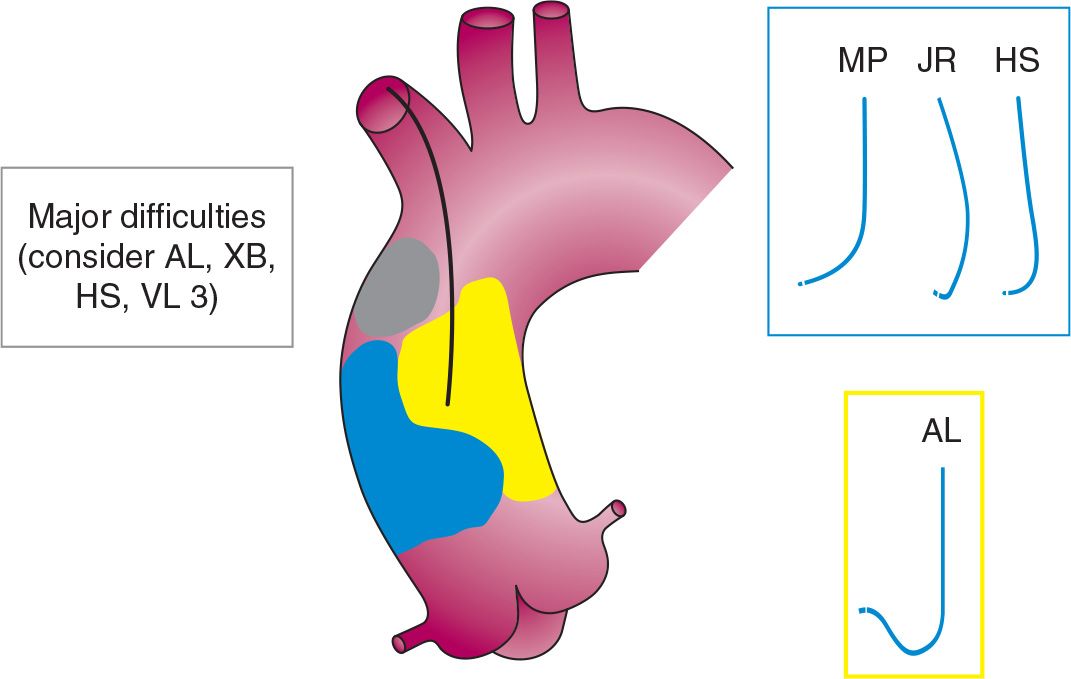
FIGURE 16-5 Catheters for SVG cannulation from right radial approach according to the origin of proximal graft anastomosis from ascending aorta; the troublesome “black zone” is represented in red (AL, Amplatz left; HS, Hockey Stick; JR, Judkins right; MP, multipurpose; VL 3, Voda left 3; XB, eXtra backup).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


