Transpharyngeal/Upper Transesophageal Examination
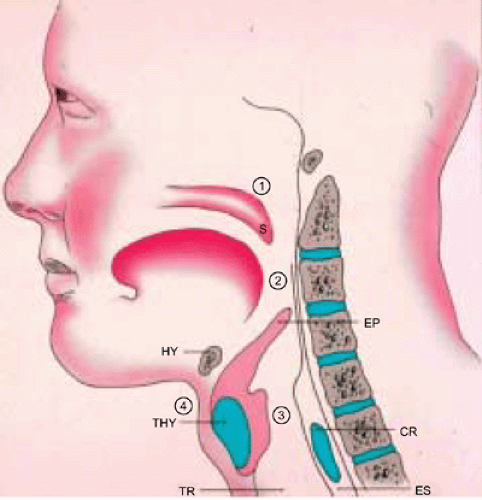
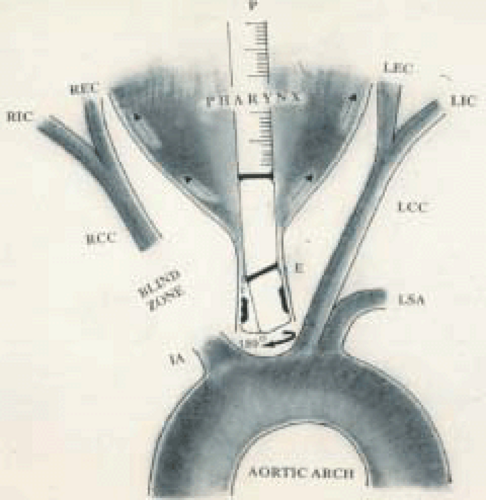
With the transesophageal probe positioned in the upper esophagus, the aortic arch and the proximal extent of its branches can be comprehensively examined in most patients. Longitudinal plane examination (90°) with clockwise rotation at the level of the aortic arch brings the origin of the innominate artery into view. This vessel can be followed in its proximal extent but the bifurcation cannot be imaged in most instances because of interference from the tracheobronchial tree. Counterclockwise rotation identifies the origin of the left common carotid artery and then, with further rotation, the left subclavian artery. If no branches are visualized using this maneuver, the probe is gradually withdrawn, carefully rotating it to detect these vessels. It is important to keep the color Doppler turned on during this procedure as color flow signals are useful in differentiating these vascular structures from the surrounding soft tissue. The left subclavian artery courses anteriorly and Doppler investigation reveals high resistance velocity waveforms with antegrade flow in systole and retrograde flow in diastole. The left subclavian artery gives rise to a number of branches, the most important of which are the left vertebral and left internal mammary arteries. These vessels usually arise opposite each other, generally at the point where the subclavian artery turns to course anteriorly. The internal mammary artery displays high resistance Doppler waveforms, whereas the vertebral artery shows low resistance signals characterized by prominent antegrade flow in both systole and diastole. Both vessels are smaller than the left subclavian artery. The left common carotid artery is generally about the same size as the subclavian artery, but displays low resistance Doppler signals, and none of its branches are visualized distinguishing it from the subclavian artery. Careful slow withdrawal of the probe, from the esophagus into the pharynx, while keeping the left common carotid artery in view, may demonstrate a slight dilatation (carotid bulb) before its bifurcation into the left internal and external carotid arteries. It is noteworthy to mention that the Doppler ultrasound beam can, in most instances, be aligned exactly parallel to flow direction in the internal carotid artery, permitting accurate assessment of velocities in the lumen of this vessel. This is in contrast to the surface approach where the Doppler beam is at a significant angle to the flow direction, which can result in marked underestimation of velocities, leading to erroneous diagnosis of stenosis severity. Both vessels show antegrade flow in systole and diastole, but generally the waveforms from the external carotid artery are sharper and the diastolic antegrade flow is less prominent. Also, the external carotid artery gives off branches that are easily visualized, whereas the internal carotid artery gives no branches in its extracranial course. If the intent is to examine right-sided neck vessels, then the probe, while in the upper esophagus, is rotated so that the face or footprint of the transducer is turned toward the right side of the patient. The probe is then gradually withdrawn and rotated slightly to identify vessels on the right side. Because of interference from the tracheobronchial tree, no vessels may be visualized for a few centimeters during probe withdrawal, but then one or more vessels appear while the probe is still in the esophagus. Doppler interrogation is then used to determine whether the vessel is the right subclavian or right common carotid artery. Similar to the right common carotid artery, the right vertebral artery will also demonstrate low resistance Doppler signals. However, this vessel is much smaller and its origin from the subclavian artery may be identified. In some patients, the right common carotid artery is the only vessel visualized when the probe is facing the right side of the patient. Further withdrawal of the probe into the pharynx will demonstrate its bifurcation into right internal and external carotid arteries. Here also, it is easy to align the Doppler ultrasound beam parallel to the flow direction in the internal carotid artery. Throughout this examination, with the probe positioned in both the upper esophagus and the pharynx, veins of different caliber are noted
adjacent to these arteries. These are easily differentiated by their typical nonpulsatile continuous Doppler flow signals throughout the cardiac cycle. Because of the collapsed nature of the esophagus, the probe is in close contact with the esophageal wall when it is rotated to examine the vessels on both the left and right sides of the patient. However, once the probe has been withdrawn into the pharynx, which is a considerably larger cavity, contact may be lost, making it impossible to see the vessels. The probe will then need to be physically moved to the opposite side for contact with the pharyngeal wall or reinserted into the esophagus, rotated appropriately to the opposite side of the neck, and withdrawn into the pharynx, taking care to maintain contact with the pharyngeal wall. Another alternative is to physically place the probe in the tonsillar fossa either before commencing the transesophageal examination or after completion of the procedure. The carotid artery can be palpitated in the tonsillar fossa and the probe placed directly over it. An important prerequisite for this procedure is adequate topical anesthesia of the pharynx. Otherwise, patient gagging and tongue motion will dislodge the probe. The procedure is easier to perform in older patients without repeating topical anesthesia because many of them have a poor gag reflex. A major advantage of this procedure is examination and assessment of the neck vessels during transesophageal echocardiography without using another probe, and accurate assessment of vessel stenosis severity. In addition to assessing carotid artery stenoses, the technique has been used to detect the patency of stents placed in the internal carotid artery, carotid body ganglioma, distal extracranial segments of vertebral arteries, and reversed diastolic blood flow in the neck vessels in severe aortic regurgitation. Successful transpharyngeal examination depends, among other things, on patient anatomy and cooperation, and on operator experience.
adjacent to these arteries. These are easily differentiated by their typical nonpulsatile continuous Doppler flow signals throughout the cardiac cycle. Because of the collapsed nature of the esophagus, the probe is in close contact with the esophageal wall when it is rotated to examine the vessels on both the left and right sides of the patient. However, once the probe has been withdrawn into the pharynx, which is a considerably larger cavity, contact may be lost, making it impossible to see the vessels. The probe will then need to be physically moved to the opposite side for contact with the pharyngeal wall or reinserted into the esophagus, rotated appropriately to the opposite side of the neck, and withdrawn into the pharynx, taking care to maintain contact with the pharyngeal wall. Another alternative is to physically place the probe in the tonsillar fossa either before commencing the transesophageal examination or after completion of the procedure. The carotid artery can be palpitated in the tonsillar fossa and the probe placed directly over it. An important prerequisite for this procedure is adequate topical anesthesia of the pharynx. Otherwise, patient gagging and tongue motion will dislodge the probe. The procedure is easier to perform in older patients without repeating topical anesthesia because many of them have a poor gag reflex. A major advantage of this procedure is examination and assessment of the neck vessels during transesophageal echocardiography without using another probe, and accurate assessment of vessel stenosis severity. In addition to assessing carotid artery stenoses, the technique has been used to detect the patency of stents placed in the internal carotid artery, carotid body ganglioma, distal extracranial segments of vertebral arteries, and reversed diastolic blood flow in the neck vessels in severe aortic regurgitation. Successful transpharyngeal examination depends, among other things, on patient anatomy and cooperation, and on operator experience.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree