CHAPTER 5 Transoesophageal and stress echo and other echo techniques
5.1 TRANSOESOPHAGEAL ECHO
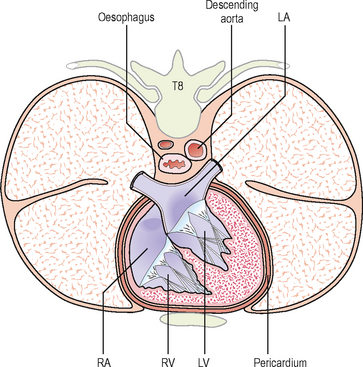
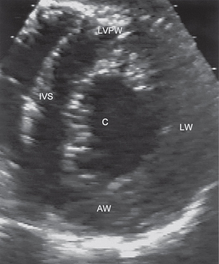
The echo techniques described so far have used ultrasound directed from the chest wall – transthoracic echo (TTE). The oesophagus in its mid-course lies posterior to and very close to the heart and ascending aorta and anterior to the descending aorta (Fig. 5.1).
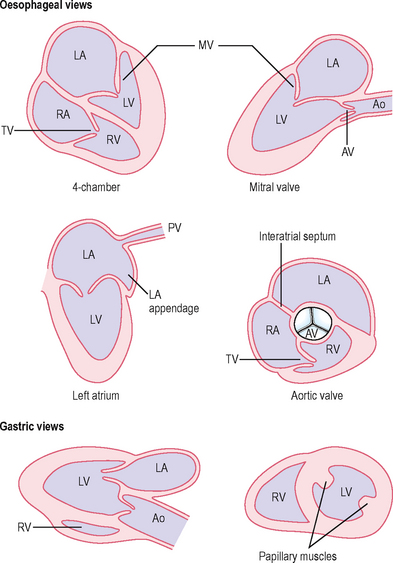
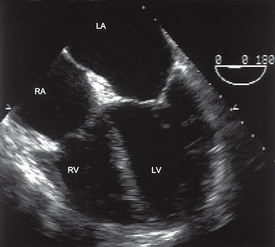
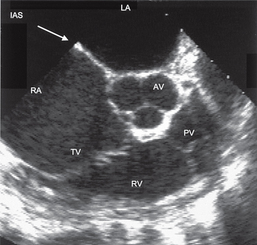
An echo technique exists for examining the heart with a transducer in the oesophagus – transoesophageal echo (TOE) (Figs 5.2, 5.3, 5.4, 5.5). In some countries, the abbreviation used is TEE. This uses a transducer mounted upon a modified probe similar to those used for upper gastrointestinal endoscopy and allows examination of the heart without the barrier to ultrasound usually provided by the ribs, chest wall and lungs. By advancing the probe tip to various depths in the oesophagus and stomach, manoeuvring the tip of the transducer and by altering the angle of the ultrasound beam with controls placed on the handle, a number of different views of the heart can be obtained.
Advantages of TOE
Uses of TOE
Patient preparation and care during TOE
The patient should give informed consent being aware of the potential risks which include:
Contraindications to TOE
Specific uses of TOE
1. Cardiac or aortic source of embolism
Risk factors for LA thrombus include:
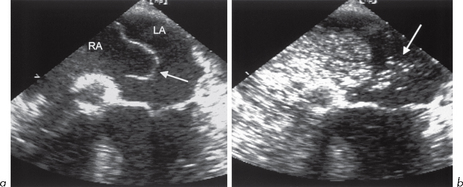
In some studies of patients with cerebral ischaemia (TIA and stroke), up to 5% had LA thrombus and in 75% of cases this was in the LA appendage (Fig. 5.6). Thrombus may appear as a rounded or ovoid mass that may completely fill the appendage. False-positive diagnosis of thrombus may occur due to misinterpretation of LA anatomy:
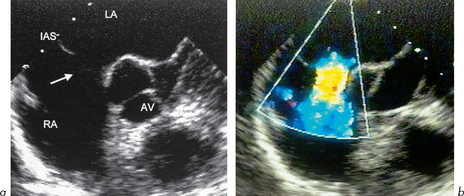
Atrial septal aneurysm (Fig. 5.7)
This is a bulging of the fossa ovalis and is found at autopsy in 1% of individuals. For echo purposes, the bulge must involve 1.5 cm of the septum and protrude 1.1 cm into either atrium. It is found in 0.2% of TTE series. In suspected cardiac source of embolism, it occurs in up to 15% of cases. The association with TIA/stroke may be because the aneurysm is thrombogenic and/or due to its frequent association with PFO and ASDs, which may allow paradoxical right to left embolization. TOE can help to detect all of these. A bubble contrast study during TOE can help to identify a small ASD or PFO and show a small shunt (section 6.4).
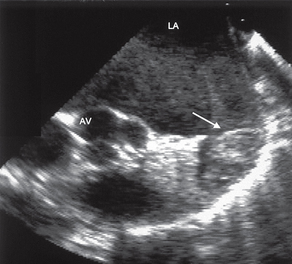
2. Examination of the aorta
TTE only gives good images of the ascending aorta, aortic arch and proximal descending aorta in a small minority of adults. TOE can add to this by providing excellent imaging of the aortic root, proximal ascending aorta, distal aortic arch and descending thoracic aorta. The interposition of the trachea between the oesophagus and ascending aorta limits the ability to image the upper ascending aorta and proximal aortic arch.
3. Endocarditis
TTE should always be used in the initial assessment of suspected or definite endocarditis. The superior spatial resolution provided by TOE allows small vegetations of only 1–2 mm to be identified and their location and morphology to be examined. All valves can be examined, but TOE is especially useful for the mitral and aortic valves (right-sided vegetations are often large and can be detected by TTE). In aortic subacute bacterial endocarditis (SBE), TOE is especially useful for aortic root abscess (TOE shows over 85% of such cases, TTE less than 30%), fistula or aneurysm of the sinus of Valsalva.
TOE is of use in endocarditis:
TOE should be considered in the majority of cases of suspected endocarditis.
4. Native valve assessment
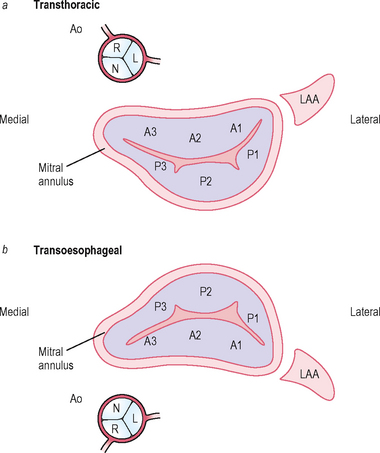
Mitral valve
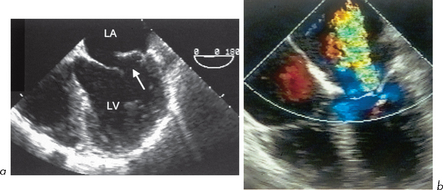
TTE is good but some aspects may be hard to assess. The posterior leaflet may be poorly visualized, especially if calcified or in the presence of mitral annular calcification. TOE can provide essential information in planning intervention such as MV repair (Figs 5.9 and 5.10).
In MR, quantitative assessment of severity by TTE is difficult. TOE allows a more thorough assessment by Doppler and colour flow of the degree of MR within the LA. Severity can also be assessed by the pattern of pulmonary venous flow (severe MR may be associated with reversal of flow). The morphology of the valve can be examined to assess if suitable for valve repair rather than replacement. The exact segment of the valve which is causing regurgitation can be identified.
TOE can be used intraoperatively to assess the adequacy of valve repair.
Balloon valvuloplasty for MS is not suitable if:
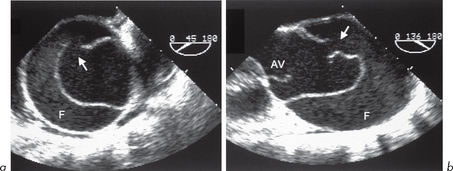
5. Prosthetic valve assessment (see section 6.3)
For aortic prostheses, TOE also has advantages over TTE, especially in biological valve degeneration, obstruction of prosthesis, regurgitation, abscesses or mass lesions (vegetations, thrombus). There are still some limitations even with TOE. The imaging planes are limited and as a result the acoustic shadow generated by mechanical prostheses may hide lesions in some areas. Aortic prostheses leave a portion of the aortic annulus immune from interrogation which may lead to underdiagnosis of root abscess.