Translumbar Approach for Coiling of Type II Endoleaks
Courtney J. Warner
Claire L. Griffin
Eva M. Rzucidlo
Over the last two decades, endovascular aneurysm repair (EVAR) has emerged as the first-line therapy for abdominal aneurysm repair. While its intrinsic low risk profile and tolerability appeal to patients, endoleaks remain a relatively frequent complication necessitating careful CT follow-up. A type II endoleak refers to ongoing perfusion of the aneurysm sac from back bleeding lumbar or inferior mesenteric arteries, occurring after 10% to 20% of EVAR procedures. In general, Type II endoleaks have a benign natural history, with up to 35% thrombosing spontaneously on follow-up imaging by 6 months and up to 60% thrombosing by 4 years. There are no consensus guidelines dictating when intervention for persistent type II endoleaks should be undertaken but most would agree that aneurysm expansion >5 mm in the presence of a Type II endoleak warrants intervention to mitigate pressurization of the aneurysm sac.
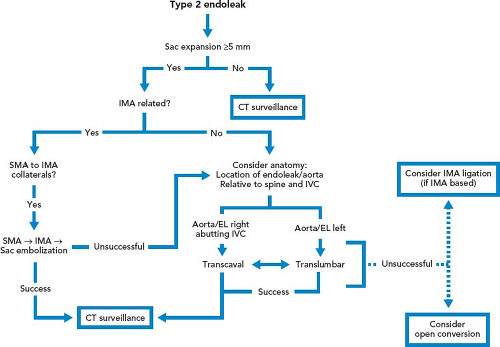
Multiple techniques are available to treat Type II endoleak with sac expansion, including translumbar, transarterial, and transcaval approaches. Selection of the optimal approach depends on the branch vessel involved and anatomical factors, including the location of the aneurysm sac (and the endoleak channel within the sac) and its relationship to other periaortic structures. The translumbar approach to Type II endoleak embolization has been shown to be safe and effective, with a low risk of complications and durable success rate based on the current literature. This technique is preferred when the endoleak is accessible from the left side of the aneurysm sac, there is an adequate soft tissue window in the left retroperitoneum, and the IMA is not involved. A transarterial approach may be optimal if the culprit branch vessel is the IMA or a hypogastric branch with a direct pathway to the aneurysm sac, although this technique can be technically challenging and embolizing one branch may not adequately treat the endoleak. The transcaval approach is another option, and may be preferable if the aneurysm sac and endoleak site are adjacent to the IVC. Please see Figure 40.1 for a proposed treatment algorithm, as documented by Scali et al. in the Journal of Vascular Surgery.
Successful translumbar coil embolization is predicated on careful planning and angle calculation based on preoperative imaging. CT arteriography of the abdomen and pelvis with a delayed phase allows for diagnosis, and often localization, of the branch vessel source. Additionally, CT imaging allows for gantry angle determination and planning the needle pathway based on metallic endograft and osseous landmarks. Required preprocedure measurements include:
Depth measurement from skin to aneurysm sac
Distance from lumbar vertebral body to aneurysm sac
Gantry angle permitting “end-on” view for needle approach to the aneurysm sac
Gantry angle permitting orthogonal view for needle approach to aneurysm sac (should be 90 degrees from “end-on” view)
In addition to requisite CT imaging, duplex ultrasound with color flow may also be used to localize the endoleak and can provide useful information regarding direction of flow. Duplex ultrasound has the advantage of avoiding contrast administration, but study quality may be limited by body habitus and bowel gas. Vascular lab imaging applications like VNAV (volume navigation technology) merge CT images with ultrasound to allow for the creation of detailed endoleak imaging as well as real-time comparison between the CT and duplex ultrasound.
Translumbar Approach
Positioning
The patient is positioned prone on the angiography table under moderate sedation. Antibiotic prophylaxis is administered prior to the procedure.