Transient Ischemic Attack
A 44-year-old woman suffered from a transient ischemic attack 2 years ago. An echocardiogram revealed a patent foramen ovale (PFO) in association with an atrial septal aneurysm. No other cause for her ischemic cerebral event could be determined. Therefore, she underwent PFO closure, and a 20-mm Premere device (Velocimed LLC, Minneapolis, Minnesota) was implanted uneventfully. Aspirin (100 mg) daily and clopidogrel (75 mg) daily were prescribed after the procedure.
At her first follow-up echocardiogram, the device position appeared appropriate, and there was no residual shunt through the PFO. However, a small thrombus was seen attached to the right atrial side of the Premere occluder. This is shown in the following image in a long-axis view (live 3D transesophageal echocardiogram [TEE]). (See Fig. 27-1 and Video 27-1.)
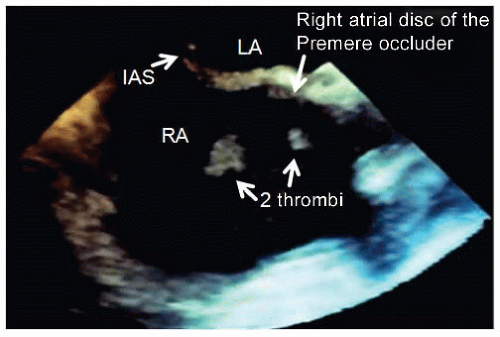 Figure 27-1. Two mobile thrombotic formations attached to the right atrial side of the Premere occluder (IAS, interatrial septum; LA, left atrium; RA, right atrium). |
QUESTION 1. Which therapy would you recommend to treat the thrombus?
A. Continue with aspirin and clopidogrel and perform another follow-up TEE in 4 to 6 weeks
B. Anticoagulation therapy
C. Anticoagulation therapy and aspirin
D. Anticoagulation therapy, aspirin, and clopidogrel
E. Surgery
View Answer
ANSWER 1: C. The overall incidence of thrombus occurrence after transcatheter PFO closure is rare.
Currently, there are no accepted guidelines regarding the best management strategy in case of a thrombus on a device.
In our case, full anticoagulation therapy in combination with aspirin was administered.
The following 3D TEE full volume image shows the situation 2 months later (Fig. 27-2 and Video 27-2).
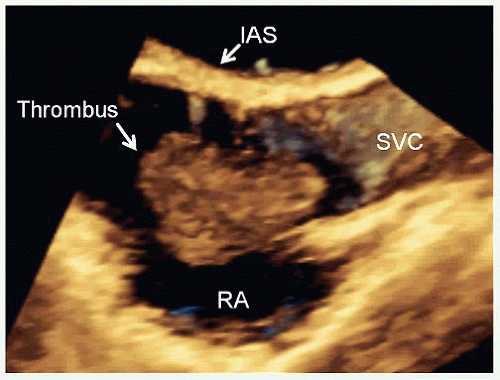 Figure 27-2. Thrombotic mass attached to the right atrial side of the Premere occluder (IAS, interatrial septum; RA, right atrium; SVC, superior vena cava).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|