Fig. 8.1
Left-side port placement. Left-side instrument ports are used for grafting the left anterior descending (LAD), diagonal branches (DB), ramus branch (RB), and obtuse marginal (OM1 and OM2) vessels. Instrument trocar insertion sites are shown as follows: (1) endoscopic camera [fifth interspace] (2) right instrument arm , (3) Stabilizer port (left midclavicular line in subcostal area) [seventh interspace] (4) sub-xiphoid stabilizer port for anterior vessels
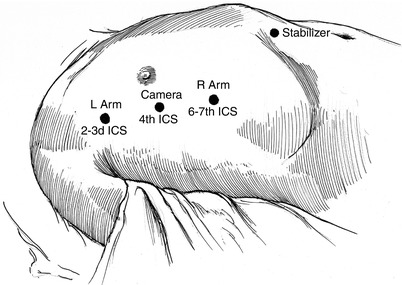
Fig. 8.2
Right-side port placement. Right side instrument ports are used for grafting the right coronary artery (RCA) and sometimes the left anterior descending coronary artery. Instrument trocar insertion sites are shown as follows: (1) endoscopic camera (2) left instrument [second or third interspace], (3) right instrument arm [sixth or seventh interspace], (4) sub-xiphoid stabilizer port for right coronary artery TECAB
For effective coronary revascularization, robot instrument ports should be positioned as follows for the following specific arteries during TECAB surgery:
LAD, diagonal (DB), and ramus (RB) coronary artery arteries. Camera and instrument arm ports should be placed 3–5-cm medial (ventral) to the anterior axillary line. Thereafter, the coronary artery stabilizer is inserted in the mid-clavicular line below subcostal margin. When grafting anterior coronary arteries, instrument arm ports are inserted generally through the left third and seventh intercostal spaces (ICS) (Fig. 8.1).
Ramus branch (RB), first obtuse marginal (OM1), and/or second obtuse marginal (OM2) coronary arteries. In comparison to the instrument positions described above, for posterior and lateral vessels, the camera and the instrument ports are moved 1–2 cm farther posteriorly than with LAD grafting for better access to the target vessels. The stabilizer port remains in the same location as for the anterior vessels.
RCA and/or LAD coronary arteries. Right side instrument ports are placed either in the third and seventh or the second and sixth ICS. The camera port is inserted in either the fourth or fifth ICS. A right subxiphoid port is placed for introduction of the endoscopic stabilizer (Fig. 8.2).
Single Vessel TECAB
LITA to LAD Grafting
Using micro-forceps and the spatula cautery (set at 15 J), the LITA is dissected from the chest wall, beginning at the first rib (Fig. 8.3). Graft harvesting should proceed in a lateral to medial fashion with the endo-thoracic fascia removed from the LITA pedicle. The LITA should be skeletonized from the first rib to the distal bifurcation [11]. Larger LITA side-branches must be clipped with chest wall ends cauterized. The LITA should remain attached to the chest wall by loose connective tissue in few places. Thereafter, the camera is reversed for 30° down viewing, and the mediastinal fat is dissected away from the pericardium. To prevent induction of ventricular fibrillation, prolonged pericardial contact with the cautery should be avoided. The pericardiotomy should start anteriorly with extension cephlad toward the pulmonary artery, exposing the left atrial appendage eventually.
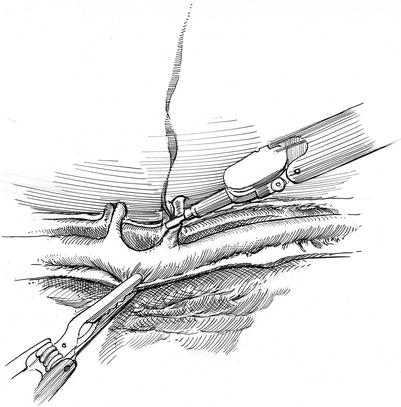
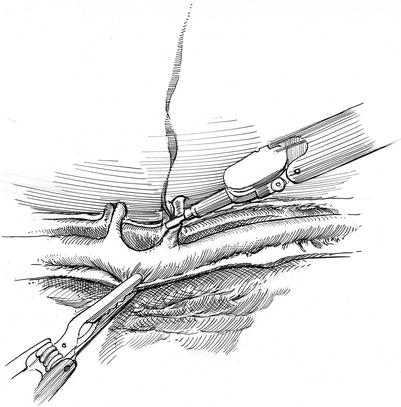
Fig. 8.3
Left internal thoracic artery (LITA) harvest. The LITA (left internal thoracic artery) is harvested from the chest wall and prepared for the anastomosis. Medium size arterial and venous side-branches are cauterized with care to avoid heat transfer to the LITA. Large branches are clipped. The LITA is skeletonized progressively
After the LAD is identified, the camera is reversed to 30° up. The endoscopic stabilizer port is inserted as described above aiming it toward the right shoulder after endoscopically dissecting the connective tissue medial to the diaphragm; a shallow insertion angle is necessary to avoid peritoneal entry. Systemic heparin is given and an activated clotting time (ACT > 300 s) is monitored every 30 min. Topical Papaverine diluted in warm heparinized saline is applied as fine jet on the ITA using a 5 French feeding catheter. Two silastic Saddle Loops (Quest Medical Inc., Allen TX) are inserted through the stabilizer cannula and secured to prevent migration. The LITA is temporarily tacked the to the epicardial fat prior to the anastomosis. A sponge tipped bulldog clamp should be placed on the proximal LITA. An attached silk suture is secured to the chest wall using a surgical clip. After two occlusive surgical clips are placed on the distal LITA, it is divided partially and spatulated (Fig. 8.4). A small portion of the arterial tip should remain attached and suspended from the chest wall. Formerly, we used S-18 flex U-clips (Medtronic, Inc., St. Paul, MN) for the anastomosis; however, they are no longer manufactured [12, 13]. Therefore, we now use two 7-cm double armed 7-0 Pronova™ (Ethicon, Inc., Englewood, NJ) sutures for the anastomosis. Each suture is passed from outside in fashion at the heel and toe while the ITA is still attached to the chest wall (Fig. 8.5). Thereafter, the LITA should be transected completely, allowing it to fall away from the anterior chest wall. This permits the anastomotic end of the LITA and embedded clips to be mobilized toward the LAD.
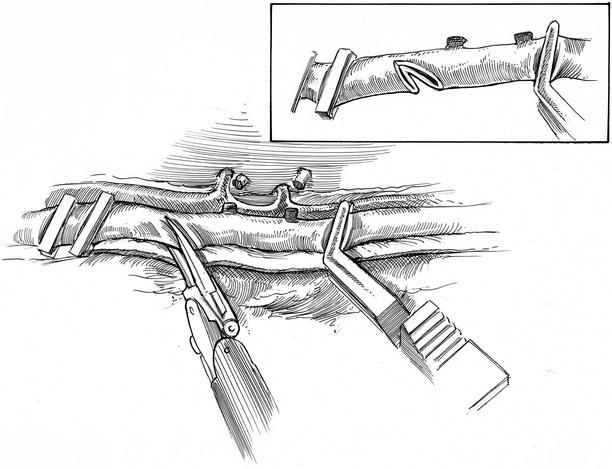
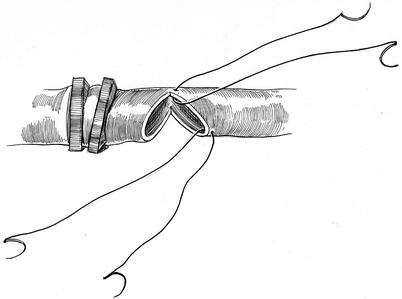
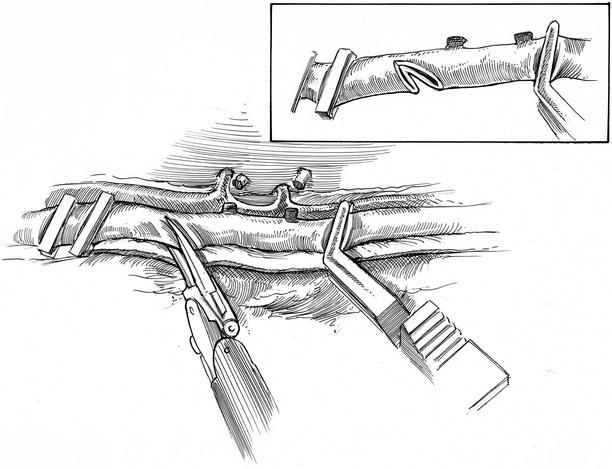
Fig. 8.4
Left internal thoracic artery (LITA) preparation. After heparin administration, two medium size occlusive clips are placed on the distal LITA, and a plastic bulldog clamp is deployed along the proximal segment. Using small robotic coronary scissors the LITA is transected partially and spatulated [Inset], leaving a tiny part of the artery suspended from the chest wall
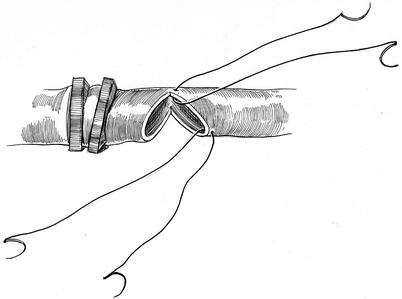
Fig. 8.5
Beginning sutures. Each suture is passed from outside in fashion at the heel and toe while the ITA is still attached to the chest wall. Thereafter, the remaining arterial tip is divided and the graft is lowered toward the anastomotic site
At this point, either the 30° endoscopic camera is rotated down or a 0° telescope is selected. Final camera orientation depends on the LAD position. Thereafter, the endoscopic stabilizer is lowered onto the LAD target epicardium, and suction attachment is activated. Warm Heparinized saline can be injected through the stabilizer catheter tip intermittently to clear the operative field. By carefully dividing the covering epicardium with the small robotic scalpel (“beaver blade”), the LAD is exposed. Thereafter, the LITA is delivered to near the anastomotic site and tacked to the epicardial fat using a hemoclip. To provide a clear operative field, silastic “saddle loops” are passed around the LAD and tightened. If either persistent ischemic changes or hemodynamic instability occur after tightening the proximal loop, intra-coronary shunting should be considered. After making the LAD arteriotomy with sharp knife, it should be extended by 4-mm (Fig. 8.6). Intermittent stabilizer irrigation keeps the anastomotic site view clear.
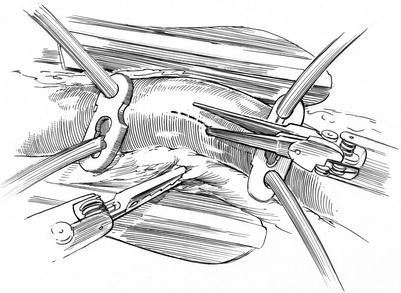
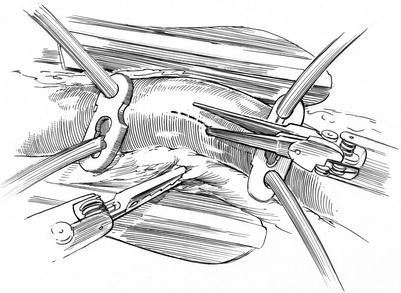
Fig. 8.6
Left anterior descending (LAD) coronary stabilization, occlusion, and arteriotomy: silastic “saddle occluders” have been placed around the proximal and distal LAD. A trans-thoracic endo-stabilizer is shown with the “feet” placed on each side of the LAD to reduce local cardiac motion. The arteriotomy is made with sharp robotic scissors and carried for 3-mm
After the heel and toe 7-0 Pronova™ sutures have been passed through the LAD sites, the LITA is parachuted with gentle traction to the arteriotomy. Heel and toe sutures are then tied with two or three knots. Sutures are then passed serially inside out (intima to adventitia) through the LAD, starting away from the surgeon at the heel and finishing at the toe. Following this one arm of the heal suture is continued from ITA through the surgeon-side LAD wall to the mid-point. Then, the remaining toe suture is passed in the same way to the mid-point, and the two sutures are tied. Alternatively, the remaining heel suture can be continued to the toe and tied to the previous suture (Fig. 8.7). After establishing LITA-LAD graft flow any minor “oozing” generally does not require repair sutures. A Medi-Stim™ Butterfly Flow probe (Medtronic Inc., Minneapolis MN) is delivered through the stabilizer port along with an attached 5 Fr feeding tube [14]. To maintain flow probe contact, during LITA flow measurements, sterile ultrasonic gel is delivered through the port. After adequate graft flow parameters have been established, protamine is given. Thereafter, all remaining surgical materials are removed from the thorax, using manual forceps passed through the right instrument port. For chest drainage, a 19-Fr silastic drain is passed through the left instrument port and positioned behind the left lung prior to re-inflation.
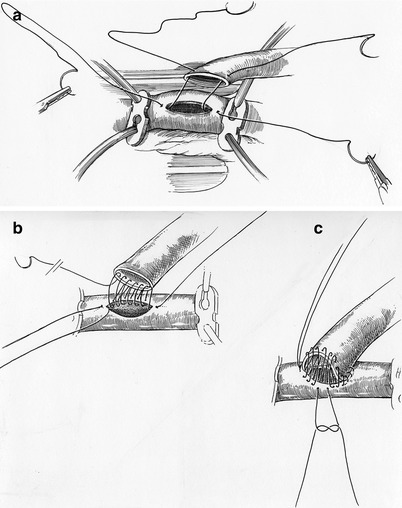
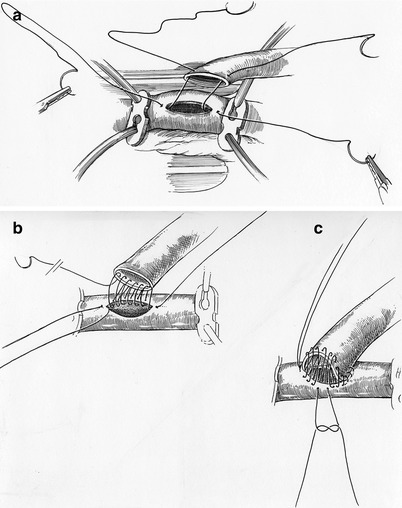
Fig. 8.7




a–c The anastomosis: (a) – 7-0 Pronova™ sutures are passed at the toe and heel inside-out through the LAD and ITA graft. (b) Starting at the heel and proceeding away from the surgeon in a counterclockwise fashion, the back wall suture is continued to the anastomotic toe. (c) This suture is then tied to the previously placed toe suture (see 8.7 a). Thereafter, the remaining heel suture is continued clockwise to the mid-point of the anastomotic front wall. Similarly, the remaining toe suture is continued counterclockwise and tied to the mid-point heel suture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


