19 Total Anomalous Pulmonary Venous Connection
I. CASE
A. Fetal echocardiography findings
1. Fetal echocardiography reveals situs solitus of the atria, levocardia, left aortic arch, and a normal heart rate of 140 bpm.
2. The four-chamber view is abnormal, with mildly enlarged right heart and a normal cardiac axis and position.
3. Cardiac size is normal (cardiothoracic ratio = 0.24).
4. The proximal pulmonary venous flow pattern is abnormal by Doppler sampling in the lung near the hilum.
5. The pulmonary artery is normal.
6. There is a small aneurysm of the fossa ovalis, and the entry of the pulmonary veins into the LA could not be visualized by two-dimensional Doppler; however, there was a gap between the descending aorta and the posterior wall of the left atrium (LA).
7. The umbilical artery Doppler is normal.
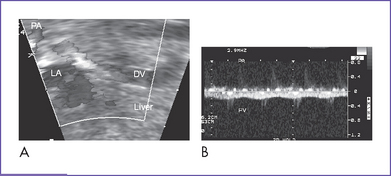
8. A descending vein near the aorta was seen with flow toward the liver (Fig. 19-1A).
9. Diagnosis of total anomalous pulmonary venous return with obstruction was also suspected due to the intracardiac disproportion and the abnormal (flat) pulmonary venous Doppler (Fig. 19-1B), and failure to identify the pulmonary veins.
D. Fetal management and counseling
1. Amniocentesis was offered but declined.
2. Follow-up included serial antenatal studies at 4- to 6-week intervals.
a. There is evidence of abnormal pulmonary Doppler (increased pulsatility index), which could suggest high pulmonary vascular resistance due to pulmonary venous obstruction.
b. Attempts at further defining the anatomy of the pulmonary venous connection are important, and in the case of the present patient, a descending vein pathway below the diaphragm was identified at follow-up studies consistent with a subdiaphragmatic connection. It is important as well that the pulmonary veins and confluence are reassessed for evidence of progressive obstruction or reduced growth. The branch pulmonary artery diameters also might not grow normally if there is high downstream resistance to flow due to pulmonary venous obstruction.
c. RV size (shortening), function, and Tei index (myocardial performance index) are monitored serially. Left ventricle (LV) growth is followed.
d. Adequacy of the foramen ovale is imaged to exclude obstruction at that level due to the increased flow.
e. The ductus venosus velocity is monitored for signs of portal hypertension.
F. Neonatal management
a. After birth, the baby will be assessed by the cardiac team. A low level of oxygenation (pulse oximeter <50% with low pressure and high oxygen ventilation) and progressive pulmonary hypertension and edema are the primary indications for intervention.
b. Management of the pulmonary hypertension includes assisted ventilation, although hyperventilation can also worsen the pulmonary edema and thus make oxygenation more difficult. For the most severe cases, an exit type of procedure with extracorporeal membrane oxygenation (ECMO) available for resuscitation may be necessary.
c. For total anomalous pulmonary venous connection (TAPVC) to the ductus venosus with obstruction, some have advocated the use of prostaglandin E1 (PGE1) infusion, but this is controversial.
d. Severely obstructed TAPVC requires emergency surgery because it cannot be medically managed.
a. Corrective repair consists of:
b. Nitric oxide might be helpful to treat associated persistent pulmonary hypertension, especially after surgery.
G. Follow-up
1. The long-term outcome after surgical repair of TAPVC is excellent. Because the surgical repair results in a normal circulation, these children are typically expected to grow and develop normally.
2. Long-term survival depends in part on the development of pulmonary vein stenosis, which is a rare but lethal complication.
a. Stenosis can occur within weeks or months after the repair.
b. Obstruction can occur at the site of surgical repair or can result from abnormalities of the pulmonary veins themselves. Such pulmonary vein obstruction can lead to a shortness of breath or wheezing, particularly on exertion.
c. The diagnosis can be somewhat difficult but can be made at echocardiography and confirmed at cardiac catheterization.
d. In the first year after a neonatal repair, the infant should be seen at more frequent intervals to exclude progressive pulmonary venous obstruction. Thereafter, yearly cardiology assessments that include echocardiography should be provided.
3. Abnormal cardiac rhythm is another late complication of TAPVC.
a. Because of the extensive atrial surgery involved in the repair, some patients experience abnormal electrical impulses arising in the atrium.
b. If such impulses occur in isolation, they are typically benign.
c. On rare occasions, sustained episodes of tachycardia or bradycardia could require treatment.
H. Risk of recurrence
1. Some reports have shown that TAPVC can run in families.
2. Bleyl and colleagues (1993) reported on a large Utah–Idaho family in which nonsyndromic TAPVC appeared to be inherited as an autosomal dominant trait with incomplete penetrance and variable expression. The family contained 14 affected members.
3. Solymar and colleagues (1987) reported three pairs of siblings with TAPVC. The types of the anomalous venous return (supra- or infracardial connections) varied within the families, indicating that genetic regulation deals with the LA connection to the intrapulmonary veins.
I. Outcome of this case
1. The baby was born weighing 3.5 kg and had Apgar scores of 8 at 1 minute and 8 at 5 minutes.
2. Venous and arterial lines were placed, and the baby was taken immediately to the neonatal intensive care unit.
3. Pulse oximeter reading was 75% to 80%.
5. Postnatal transthoracic echocardiogram confirmed the diagnosis of obstructed TAPVC (infradiaphragmatic).
6. The baby had no dysmorphic features.
7. The baby was stabilized and taken to cardiac surgery, where he had successful repair.
8. His postoperative course was marked by persistent transient pulmonary hypertension.
9. He was discharged home 10 days postoperatively with a normal feeding pattern.
II. YOUR HANDY REFERENCE
A. Total anomalous pulmonary venous connection
a. TAPVC affects about 1 in 17,000 live births.
b. It is not a common antenatal diagnosis. In the fetal series of Allan and Sharland (1994), only three isolated cases of TAPVC were reported.
c. Given the subtle abnormalities in TAPVC, the diagnosis could be missed even during a targeted fetal exam.
d. TAPVC is often identified prenatally when it occurs in combination with significant cardiac defects such as coarctation, hypoplastic left heart syndrome, or heterotaxy syndrome.
e. The Baltimore–Washington Infant Study (BWIS), a population-based exploratory case-control study of cardiovascular malformations, identified 41 cases of TAPVC during the period 1981 to 1987. These constituted 1.5% of all cardiovascular malformations (N = 2659), with a regional prevalence of 6.8 per 100,000 live births.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree