15 Thromboembolic Phenomena and Vegetations
Background
Thrombus
• Thrombus is predisposed to form in areas of the heart where there is low-velocity blood flow or flow stasis.
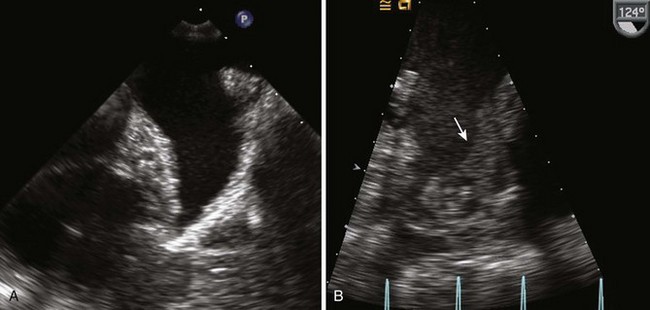
• The left atrium (LA) (especially the left atrial appendage [LAA] [Fig. 15-1]) is a common area of thrombus formation when associated with atrial arrhythmias or mitral stenosis.
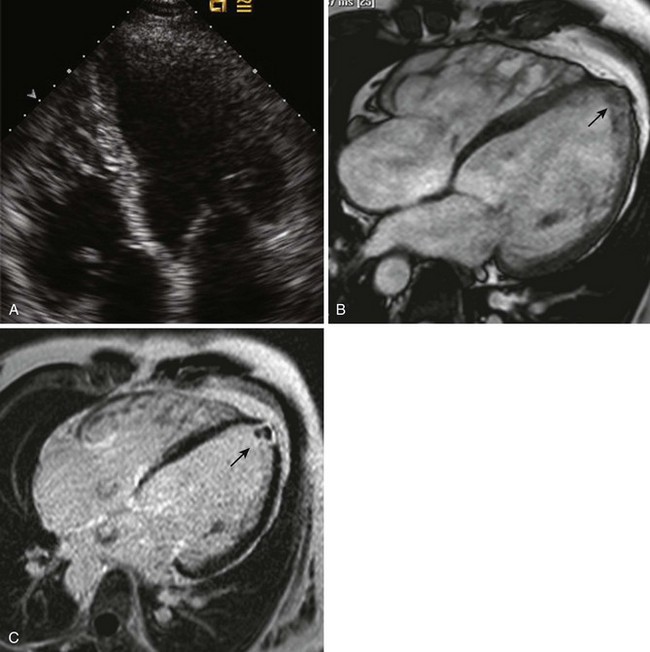
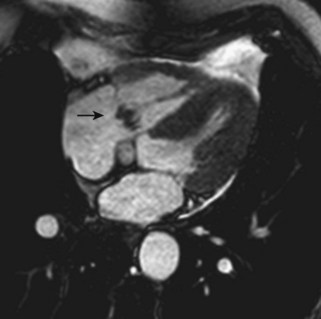
• The left ventricle (LV) is a common area of thrombus formation when associated with left ventricular dysfunction (global or regional) (Fig. 15-2), aneurysm, or pseudoaneurysm (Fig. 15-3). The apex is a common area for thrombus formation.
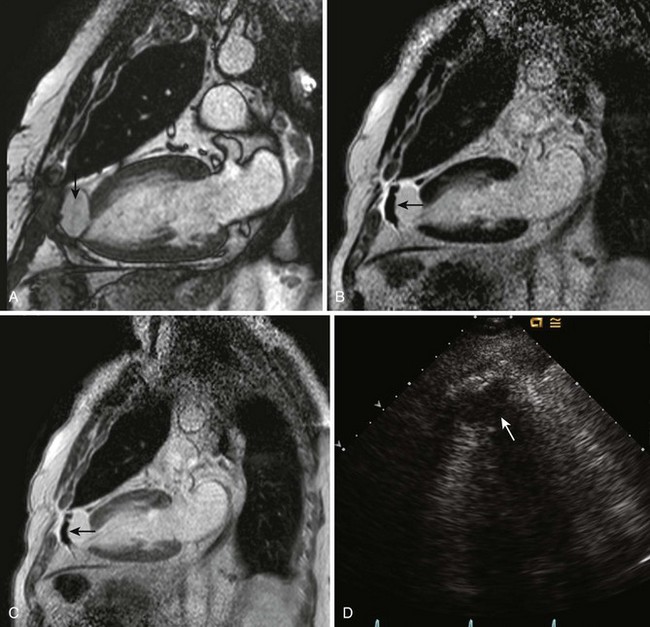
• Thrombus formation within the right heart may occur in cases of severe right atrial enlargement (i.e., atriopulmonary Fontan) or right ventricular dysfunction. More commonly, thrombus formation occurs within veins and embolizes to the right heart. Thrombus may become trapped in the right atrium (RA) (Chiari network or Eustachian valve), in the right ventricle (RV) (tricuspid valve apparatus or right ventricular trabeculations), or pulmonary arteries (PAs) as it embolizes (Fig. 15-4).
• Thrombus formation may occur on intracardiac devices seen within the right heart such as pacing/defibrillator leads and central venous catheters. Thrombus formation can result on intracardiac walls of the right heart if a central venous catheter tip results in local trauma.
• Thrombus formation may occur in surgically placed conduits (Glenn shunt, Fontan shunt, RV-to-PA conduit). Thrombus can be difficult to visualize on echocardiography (echo) due to artifact from conduits or the lack of an ultrasound window. Magnetic resonance imaging (MRI) or computed tomography (CT) may be more helpful in this regard.
• Intracardiac shunting can result in venous thrombi embolizing to the arterial system. The most common shunts for which this may occur are a patent foramen ovale (PFO), atrial septal defects (ASDs), baffle/conduit leaks, and larger ventricular septal defects (VSDs) with right-to-left shunting such as Eisenmenger physiology.
• Thrombus can also occur on prosthetic valves. Clinical presentation may occur as a result of an embolic event or symptomatic valve dysfunction or may be directly visualized by echo in an asymptomatic patient.
Vegetations
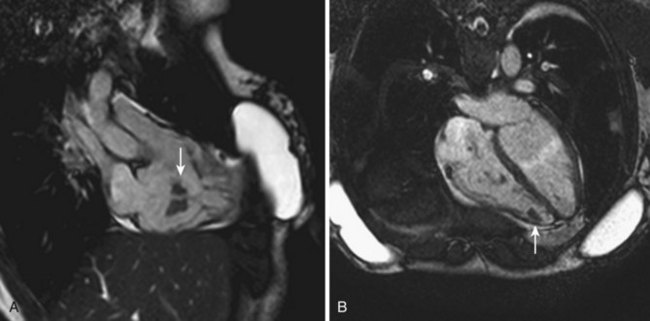
• Noninfectious vegetations may also occur and are commonly referred to as marantic or nonbacterial thrombotic endocarditis (NBTE). NBTE usually occurs in the context of a malignancy or autoimmune disease (Fig. 15-5). A metastatic malignancy does not necessarily have to be present. Although blood cultures and an accurate determination of whether the patient was exposed to antibiotics at the time of blood sampling for culture are essential in identifying vegetations as infectious or noninfectious, there are some imaging characteristics of NBTE: vegetations tend to be less mobile, more sessile, and located toward the base of the leaflets. Because the base of the valve leaflets is more commonly affected, less severe valve regurgitation is noted. Anticoagulation should be considered in patients with NBTE.
• Mobility and location are important distinguishing features of a vegetation. Vegetations have motion independent of a valve leaflet and are most commonly associated with the upstream surface of a valve leaflet (e.g., the right atrial side of the tricuspid valve [Fig. 15-6]) but have also been reported on the Eustachian valve, residual Chiari network, subvalvular apparatus, and chamber wall. Commonly, the vegetations are not rounded in appearance. Vegetations usually have low reflectance of ultrasound waves but over time may become more calcified (high reflectance). Visualization of vegetations in more than one ultrasound window decreases the likelihood of an ultrasound artifact.
• Vegetations can occur on intracardiac devices such as pacing/defibrillator leads and central venous catheters (Fig. 15-7).
• Destruction of the valve apparatus (annulus or leaflet) can result in a fistulous connection between adjacent cardiac chambers (e.g., aorta to RA) or valve regurgitation.
• Paravalvular abscesses may occur as a result of endocarditis and typically occur in the annular part of the valve apparatus. Abscesses may be echogenic or echolucent spaces near the valve annulus.
• Infections of bioprosthetic or prosthetic valves are more typically an annular disease, which can result in valve dehiscence or annular abscess (Fig. 15-8).
• Adequate sampling of blood for culture and obtaining blood cultures before the commencement of antibiotics are critical for the timely diagnosis of infectious endocarditis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree