Fig. 12.1
Intimal thickening with preservation of the medial layer. Chronic inflammatory process with recanalization (Courtesy of the Study Group in Correlation Anatomy-Clinic PUCCAMP)
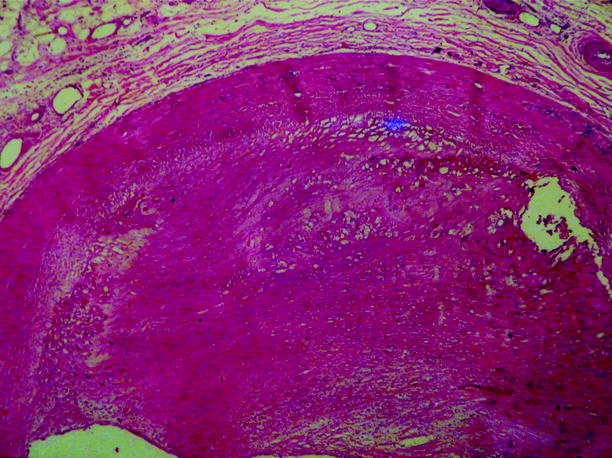
Fig. 12.2
Acute phase with thrombosis (Courtesy of the Study Group in Correlation Anatomy-Clinic PUCCAMP)
Which vascular damage occurs first, thrombotic or inflammatory, is undetermined, but the intense inflammatory infiltration and cell proliferation that are observed in lesions during the acute phase are different, especially when veins are affected. Various stages of lesions may occur in different segments of same vein when the biopsy is carried out in the acute phase with phlebitis and thrombophlebitis. In these stages we can find acute phlebitis without thrombosis, acute phlebitis with thrombosis, and acute phlebitis with thrombus associated with microabscesses and giant cells (Figs. 12.3 and 12.4).
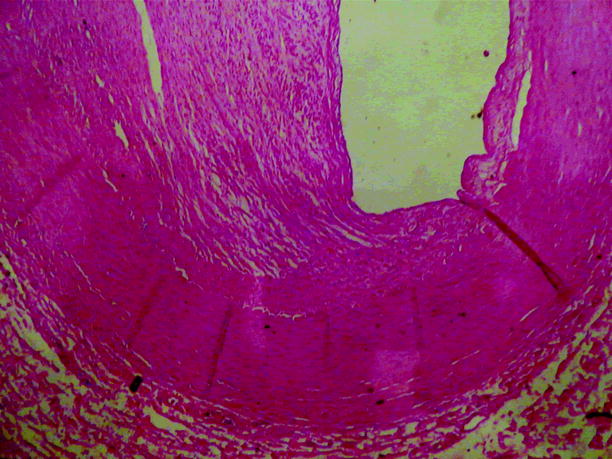
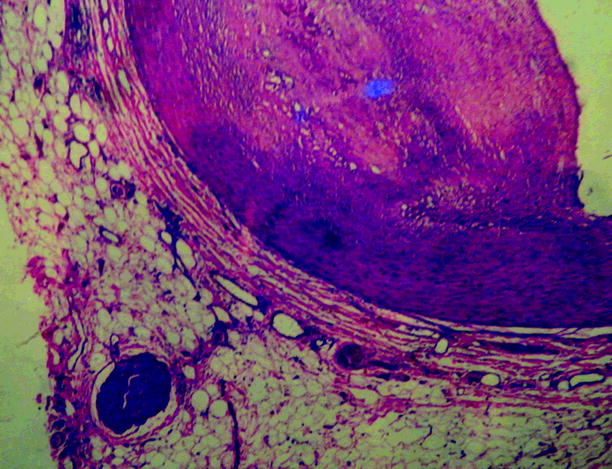
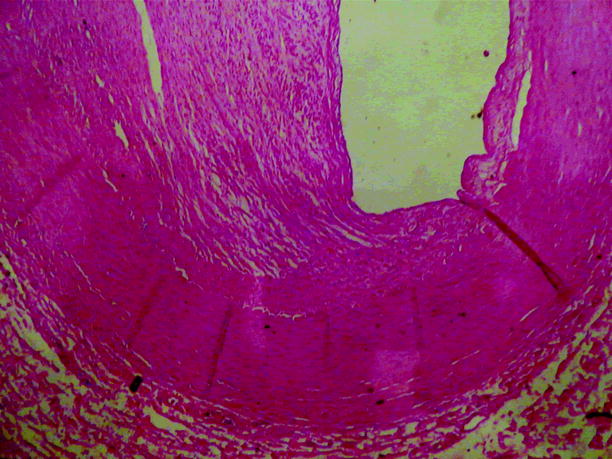
Fig. 12.3
Chronic phase with intimal and medial layer thickening (Courtesy of the Study Group in Correlation Anatomy-Clinic PUCCAMP)
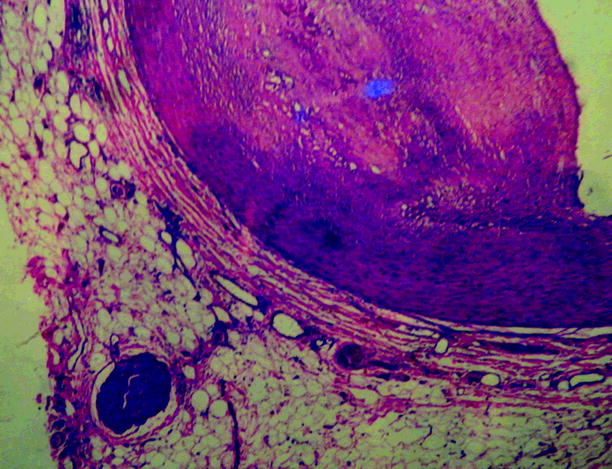
Fig. 12.4
Acute phase: intimal thickening caused by the inflammatory process. Medial layer with muscle fiber hyperplasia. Inflammatory process in the adventitia and perineural area (Courtesy of the Study Group in Correlation Anatomy-Clinic PUCCAMP)
The intermediate stage is characterized by progressive organization of thrombus obstruction in arteries and veins, often with an inflammatory cell infiltrate within the thrombus with no expressive inflammation in the vascular wall. Obstructive thrombus organization with recanalization in various stages, prominent vascularization of the medial layer, and perivascular fibrosis of the adventitia characterize the chronic phase. These lesions are least typical.
Rupture of the internal and medial elastic laminae, which often occurs in arteriosclerosis and in systemic vasculitis, differs from TAO, in which the internal elastic lamina and entire vessel wall remain unchanged in the underlying location of thrombus obstruction in three stages of the disease.
There is no necrosis of the arterial wall in TAO as it presents with parietal architectural integrity, especially in the medial layer, which distinguishes it from other forms of necrotizing arteritis. Also no calcifications or atheromatous plaques are observed, distinguishing it from arteriosclerosis.
Endothelial dysfunction may also be involved in the pathogenesis of disease as high levels of antiendothelial antibodies were detected in diseased patients [22, 31].
Thromboangiitis and Arteriosclerosis
Despite histopathological differences, TAO can coexist with arteriosclerosis, especially in patients over 40 years of age, creating an additional difficulty for diagnosis. Excessive use of tobacco increases the risk of arteriosclerosis.
The histological appearance of thrombus in TAO is the same as that of arteriosclerotic thrombosis, however with an exacerbated inflammatory process, with hypercellular thrombus with intense invasion of the smooth muscle cells from the medial layer and preservation of the internal elastic lamina (Fig. 12.5).
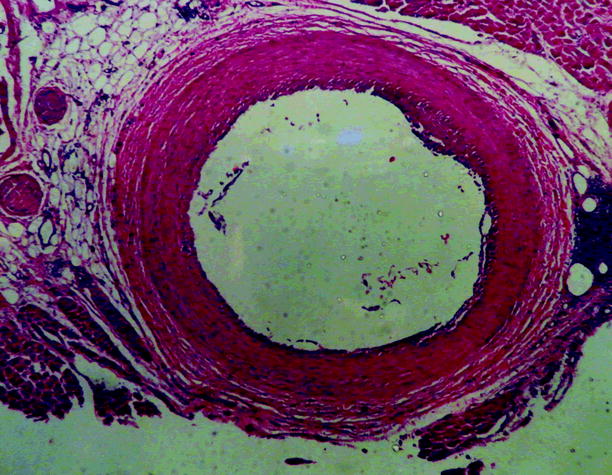
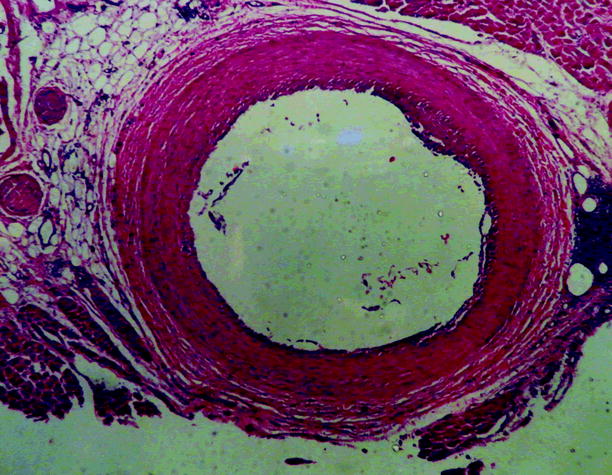
Fig. 12.5
Uniform intimal thickening. Small area of thrombosis with medial layer preservation. Inflammatory process in the adventitia and perineural area (Coronary artery courtesy of the Study Group in Correlation Anatomy-Clinic PUCCAMP)
Etiology, Pathogenesis, and Smoking
TAO is a type of vasculitis [41], but with features that differentiate it from other forms of vasculitis, presenting thrombosis with an exuberant inflammatory process, with less intense cellular activity in the vessel wall, preservation of the internal elastic lamina, and normal immunological markers.
The etiology of TAO is unknown; however, an association with the smoking habit is recognized. However, the time course of the disease can vary [13, 40, 71]. The time of onset of signs and symptoms is also associated with smoking. Manifestations are more severe in individuals who smoke all day and have less time between each cigarette; major injuries are detected in those who started smoking before the age of 20 years or have smoked for over 10 years [66].
Continued use of tobacco is closely related to disease progression, being the main factor for this progression. All researchers believe that tobacco use is a component of the TAO diagnosis. In the literature, there are no clear cases of this disease in non-tobacco-smoking patients.
Several factors have been described about how smoking affects the circulation, causing thrombosis, vasoconstriction, vascular injury produced by the altered metabolism of catecholamines, changes in the oxygen dissociation of hemoglobin in the peripheral circulation, and direct action of tobacco-derived substances in the endothelium [40, 69].
Researchers have attempted to establish an autoimmune etiology for TAO. A hypersensitivity reaction caused by tobacco in the vascular endothelium has been verified by significant amounts of active immune complexes in patients’ serum, which may compromise vessels. Endothelial lesions changing the vessels’ features induce the formation of anti-arterial antibodies, which react with the already exposed antigens to form circulating immune complexes, which are partially removed from the circulation. There is a consequent increase in platelet aggregation in response to the formation of immune complexes [26].
Hypotheses about an autoimmune mechanism haves been considered in studies describing the presence of antinuclear antibodies and increased specific antibodies in the arterial wall [24, 25].
Often found in patients with TAO, hyperhomocysteinemia seems to play an important role in the pathogenesis of the disease [70].
High levels of anti-endothelial antibodies, which are observed even before clinical manifestations of disease, cause endothelial dysfunction [61].
A higher occurrence of disease has been proven in countries with more significant consumption of tobacco, and an allergy or hypersensitivity to some component of tobacco is suspected. This sensitivity would lead to inflammatory obstructive disease of the small blood vessels.
Literature reports indicate that chronic anaerobic periodontal infections may also play a role in the development of TAO as almost two-thirds of patients with this disease also have severe periodontal disease. However, the prevalence of periodontal disease in smokers without TAO is also high [9, 30].
It is believed that other etiological factors with mechanisms for triggering disease onset are present because although tobacco use is predominant in the onset and progression of disease, only a small number of tobacco users worldwide develop the disease.
Epidemiology, Genetics, and Gender
Although the disease has worldwide distribution, it is most prevalent in the Mediterranean region, the Middle East, and Asia than in the West and North America. It occurs more frequently in countries where tobacco is widely used, especially where there is a habit of making cigarettes at home [23, 37, 42].
Recently, the disease has decreased in Europe and the United States because of the adoption of stricter criteria for diagnosis and also because of reducing the number of smokers.
In Japan, a study conducted in 1976 by the Committee for Buerger’s Disease Research of the Ministry of Health and Welfare in analyzed 3,034 patients with the disease, 2,930 men and 104 women, finding an incidence of 5 per 100,000 people [10]. These results were similar to those of a statistical study conducted by the Committee for Research on the Epidemiology of Untreatable Diseases from the Ministry of Health and Welfare in 1986 [54].
Although to date no gene has been identified, there may be a genetic predisposition to disease onset.
Disease incidence in females younger than 70 years is low, in the range of 1–2 %, with a significant increase in the 90s, by about 20 %, probably because of the increasing number of female smokers.
Vasodilation and Coagulation
Literature data indicate reduced endothelium-dependent vasodilation in the peripheral circulation of patients with TAO. There is impaired vasodilation after infusion of the endothelium-dependent vasodilator acetylcholine [45].
In patients with TAO there is also increased platelet response to serotonin [65] and elevated plasma homocysteine [8, 60].
In the pathogenesis of TAO, prothrombotic factors play a remarkable role as mutation of prothrombin gene 20210 and the presence of anticardiolipin antibodies are associated with increased risk and severity of disease [46, 57].
Immunology
Immunological factors have been the subject of several studies in patients with TAO, and several publications suggest that immune responses may be important pathogenic factors in the disease.
On one hand, more intense cellular sensitivity to collagen types I and III has been observed in patients with TAO than in healthy and arteriosclerotic patients [1, 2]. On the other hand, samples analyzed histologically for many arteries were found to have preserved the general architecture of vessel walls, irrespective of disease stage, with significant cellular infiltration in the thrombus and intima. In the acute phase, mainly macrophages and dendritic cells were identified in the intima, turning out to be TAO endarteritis caused by T-cell- and humoral-mediated cellular immunity associated with B-cell activation of macrophages or dendritic cells in the intima [34, 68].
Laboratory Aspects
There is no specific laboratory test for the diagnosis of TAO; however, all laboratory tests that contribute to the differential diagnosis should be performed, such as:
Fasting glucose
Urinalysis
Erythrocyte sedimentation rate
C-reactive protein
Antinuclear factor
Rheumatoid factor
Hemogram
Coagulation
Liver function
Renal function
Protein C
Protein S
Antithrombin III
Factor V Leiden
Prothrombin gene mutation
Toxicology: cocaine, cannabis, amphetamines
Clinical Aspects
The classic description of TAO involves a young patient, about 40 years old, a smoker, male, and often having migratory superficial thrombophlebitis and Raynaud’s phenomenon in the upper and lower limbs. The usual initial involvement is obstruction of the distal arteries and veins of the hands and feet with consequent minor and asymptomatic arterial insufficiency with frequent progression to the proximal vessels, not rarely with involvement of the superficial femoral artery. This progression of arterial lesions is accompanied by worsening clinical symptoms presenting as intermittent claudication. With disease progression, symptoms appear, such as cooling of the extremities and superficial areas of ischemia that evolve into superficial ischemic ulcers on the feet, hands, and fingers. Usually, the initial trophic lesion is periungual and is often treated with excision of the nail, culminating in finger necrosis. There is infrequent involvement of the brachial artery, common iliac artery, and great vessels [4, 5,72].
Involvement of organs is also reported in the literature. The histopathology of the vessels is the same as for the limbs, affecting the veins and arteries [27].
Although TAO affects the small and medium vessels of the extremities, the same histopathological findings have been reported in cerebral, coronary, internal mammary, renal, and mesenteric arteries [20, 36]. Involvement of multiple organs is rare [7, 49].
At least two limbs are often affected, and published reports show involvement of four limbs in 43 % of cases, three limbs in 41 % of cases, and two limbs in 16 % of cases (Figs. 12.6 and 12.7) [32, 58, 71]. In radiological tests performed in patients with disease, arteriographic changes in limb segments that have not had symptoms are frequently found.



Fig. 12.6
Female patient with involvement of all four limbs

Fig. 12.7
Male patient with involvement of all four limbs
Claudication in the legs is a common initial complaint and less frequently in the upper limbs. Plantar claudication is often an early symptom and can be confused with rheumatologic and orthopedic problems, resulting in delayed diagnosis. With disease progression, the claudication becomes more proximal, often up to the calf.
Microscopic pathological examination shows significant inflammation around the nerve fibers, which indicates ischemic neuropathy.
Rheumatological symptoms are frequent in patients with TAO, and the classic Raynaud’s phenomenon is presented in approximately 50 % of patients, even asymmetrically in the limbs [21].
Recurrent arthralgia in the large joints with important local inflammatory signs may indicate prodromal signs of TAO years before the appearance of arterial occlusions [67].
Migratory thrombophlebitis can arise early, even before arterial symptoms, and can distinguish TAO from other diseases (Fig. 12.8). It may also be present in 50 % of cases and often demonstrates local disease activity; biopsies demonstrate the classic histopathological aspects of TAO [62, 64].


Fig. 12.8
Migratory thrombophlebitis
It may present as a first symptom of TAO in approximately 25 % of patients with recurrent episodes in 60 % of cases. Palmar or plantar hyperhidrosis may appear in up to 30 % of patients [13].
Radiological Aspects
Doppler ultrasound can be useful to measure the pressoric indices and locate the occluded artery, but duplex ultrasound mapping is a non-invasive examination that can provide the most data. It quantifies the distal flow of occluded arteries, even showing characteristics of the vessel wall and the location of the distal arterial occlusion.
Ultrasound can be important to rule out an embolic source and aneurysmal disease. Parietal occlusive alterations can be clearly seen on angiography and can confirm the diagnosis of TAO.
There are no pathognomonic arteriographic aspects of TAO, but aspects such as the classic sign of Martorell (corkscrew-shaped collateral vessels) do exist (Fig. 12.9).
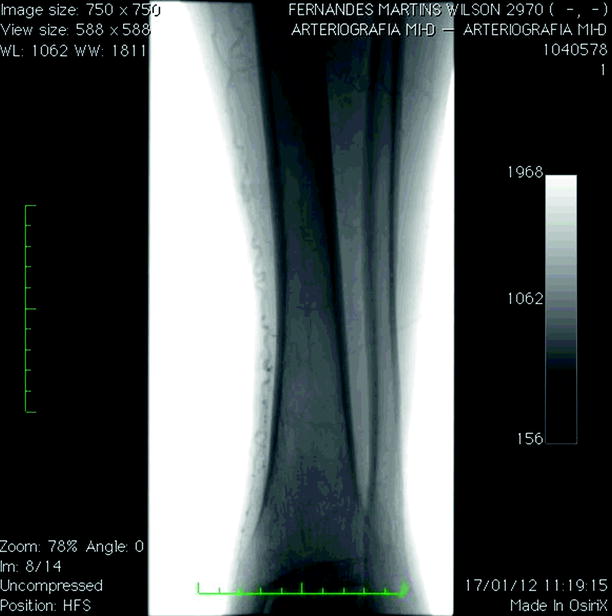
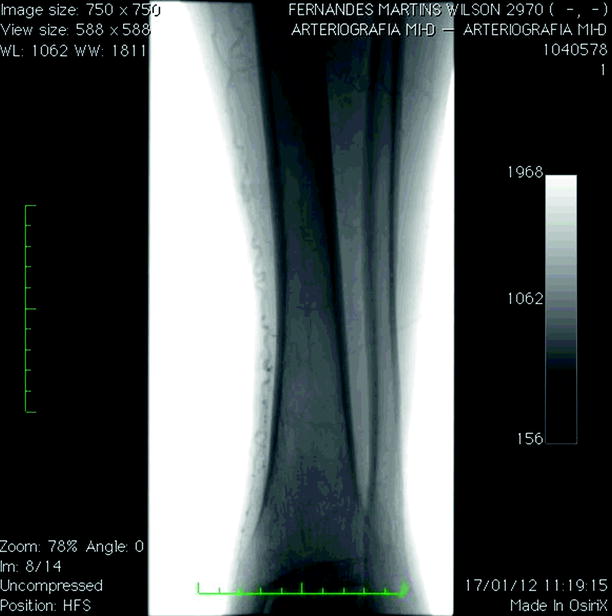
Fig. 12.9
Corkscrew-shaped collateral vessels
Arteriographic aspects of TAO are:
No signs of atherosclerosis
Involvement of vessels of small and medium caliber:
Radial, ulnar, and palmar digital arteries of the hands; tibial, peroneal, and plantar digital arteries.
Obstructive arterial lesions and spastic segmental mixed with normal segments.
Normal proximal circulation with intense distal involvement.
Corkscrew-shaped collateral vessels around sites of obstruction.
Diagnosis and Differential Diagnosis
Many authors have proposed several major and minor diagnostic criteria for diagnosis, but others believe these diagnostic criteria are not useful for diagnosis and treatment of the disease. Association with other diseases should not exclude the diagnosis. Diagnostic criteria proposed are clinical, pathological, and arteriographic [50, 64].
Notable major factors are exacerbated smoking, distal ischemic symptoms before the age of 45 years, brachial and popliteal arteries without disease, arteriographic and/or histopathological signs of disease, absence of embolic sources, absence of autoimmune diseases, no change in coagulation, and no arteriosclerosis. Notable minor factors are plantar claudication, Raynaud’s phenomenon, disease in the upper extremities, and migratory thrombophlebitis.
The most important diseases to consider for the differential diagnosis, with signs and symptoms similar to atherosclerosis, are embolisms and autoimmune diseases.
Other vasculitises should also be excluded, such as Takayasu’s arteritis or giant cell arteritis, because of proximal arterial involvement. Ischemic symptoms are extremely similar to TAO developed because of using cocaine, amphetamines, and cannabis, with frequent reports in the literature [19, 55]. It is necessary to exclude antiphospholipid antibody syndrome, which leads to arterial and venous thrombosis, rheumatoid arthritis, mixed connective tissue disease, and scleroderma.
To rule out these diseases, serological marker tests are very important, and antiphospholipid antibody syndrome may show a positive test for lupic anticoagulant and high levels of anticardiolipin antibodies. The histopathological examination of TAO thrombus shows an intense inflammatory process that differs from those not showing an inflammatory process.
Ergotism, which can also cause ischemia of both the upper and lower limbs, should be investigated and ruled out by detailed investigation.




Shinoya’s Criteria [59]
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


