Thoracoscopic Sympathectomy
Brett Broussard
Douglas Minnich
Benjamin Wei
DEFINITION
Hyperhidrosis is a medical condition that involves the overproduction of sweat/perspiration in the palms, axillae, face, or feet.
Diagnostic criteria include focal sweating of greater than 6 months and two of the following characteristics: bilateral and symmetric nature, impairs daily activities, occurs weekly at a minimum, onset at younger than 25 years of age, significant family history, and no evidence of focal sweating during sleep.
Eccrine glands innervated by the sympathetic nervous system are responsible for hyperhidrosis. Acetylcholine is the primary neurotransmitter carried by cholinergic autonomic neurons.
Hyperhidrosis can be related to an abnormal central response to emotional stress but also occurs spontaneously and intermittently. Eccrine glands appear histologically and functionally normal under microscopic examination.1 The pathophysiologic basis of hyperhidrosis remains unclear.
DIFFERENTIAL DIAGNOSIS
Generalized, or secondary, hyperhidrosis can be caused by a wide variety of systemic and metabolic reasons. Excessive heat exposure and obesity are the most common causes of generalized hyperhidrosis. Other causes include endocrine disorders, neuroendocrine tumors, infection, malignancy, and toxins. Hodgkin’s disease and tuberculosis are common causes of nocturnal hyperhidrosis.
Localized unilateral, or segmental, hyperhidrosis is rare and can be attributed to gustatory stimuli; eccrine nevus; eccrine angiomatous hamartoma; glomus tumor; polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes (POEMS) syndrome; and pachydermoperiostosis.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients typically present with history of palmar and plantar sweating since childhood. The onset of sweating may be associated with stress or occur during a time of calmness. The timing of palmar and plantar sweating is synchronous.
The presentation of sweating is intense in nature. Patients may complain of puddles of sweat around bare feet, saturation of paper while writing, or the need to change clothes multiple times a day.2
Hyperhidrosis may have a significant impact on the patient’s self-image, occupation, and social interactions.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The diagnosis of primary hyperhidrosis is obtained through a thorough history and physical examination.
If secondary or unilateral hyperhidrosis is suspected, further evaluation is warranted including laboratory studies and imaging.
SURGICAL MANAGEMENT
Various nonoperative treatments such as application of aluminum chloride alcohol solutions (Drysol), iontophoresis (placing of hands and feet in water through which electric current flows), botulinum toxin injections, and oral anticholinergics such as glycopyrrolate and oxybutynin are usually tried prior to consideration of sympathectomy.
The Society of Thoracic Surgeons (STS) expert consensus committee has adopted a nomenclature when describing sympathectomy. For example, R3 refers to a sympathectomy above the 3rd rib space.1
In preparation for sympathectomy, it is important to consider the anatomic presentation of the patient’s symptoms for operative planning.
Palmar hyperhidrosis: Disruption of the sympathetic chain above both the 3rd and 4th ribs (R3 and R4) results in the driest hands but carries an increased risk of compensatory hyperhidrosis (CH). R4 disruption alone decreases the risk for CH but may lead to suboptimal dryness of the hands. The consensus committee therefore recommends R3 disruption alone for palmar hyperhidrosis.
Palmar and plantar hyperhidrosis is best treated with R4 and R5 sympathectomy. R4 disruption alone may decrease the probability of CH, but dividing both R4 and R5 results in an excellent reduction in sweating symptoms.
Axillary hyperhidrosis (including palmar-axillary and palmaraxillary-plantar) is best treated with R4 and R5 sympathetic chain disruption. Simultaneous R3 and R4 disruption was found to increase the incidence and severity of CH.
Craniofacial hyperhidrosis needs to be distinguished from blushing. These patients benefit from R3 chain disruption alone. Studies have shown that R2 chain disruption is associated with an increased incidence of Horner’s syndrome and CH.1
There are different methods in which the sympathetic chain can be disrupted. Options include the following:
Sympathectomy: removal of sympathetic ganglion by transection of chain above and below ganglion
Sympathicotomy: simple transection of sympathetic chain
Clipping: clip placed at indicated level of sympathetic chain
Blocking: Clips are placed above and below ganglion.2
There is no clear advantage to any particular method used to disrupt the chain.
Proponents of clip application believe that sympathectomy can be reversed in the case of intolerable hyperhidrosis by removal of the clip; however, one study has shown that only about 50% of patients experience a significant decrease in CH after clip removal.3 Experimental studies suggest that the damage inflicted on the nerve with clip application leads to degeneration of the nerve within 10 days of clip application. 4 It is more important that the correct level is identified and that enough of a gap is created when the nerve bundle is transected to prevent regrowth of the nerve.1
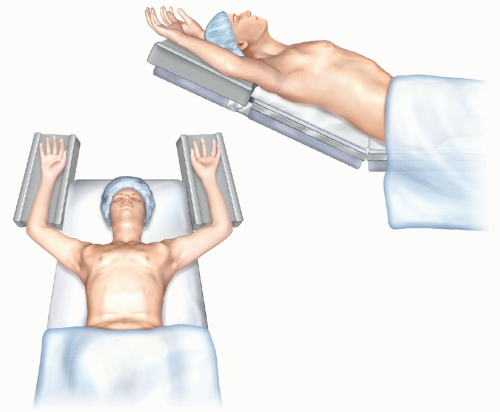
Preoperative Planning
Patients can be intubated with either a double lumen or single lumen endotracheal tube. We prefer a double lumen endotracheal tube, which allows for single-lung ventilation.
If a single lumen endotracheal tube is used, carbon dioxide (CO2) insufflation or intermittent apnea is necessary to displace the lung and gain access to the sympathetic chain.