Chapter 25 Thoracic Trauma
All types and severity of trauma can involve thoracic injury, and the mechanism of injury often provides little guidance to the nature of the injury that has been sustained. Acutely life-threatening thoracic injuries include tension pneumothorax, large open pneumothorax, massive hemothorax, and cardiac tamponade.
CHEST WALL INJURIES
Rib Fractures
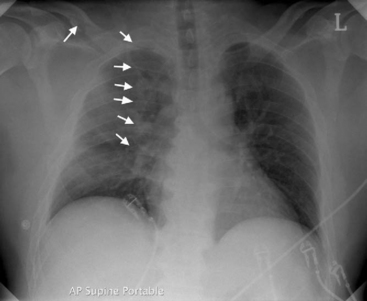
Rib fractures are the most common significant injury to the thorax. They occur after a wide range of injuries and become increasingly common as age increases and the flexibility of the rib cage decreases. Diagnosis is largely clinical because one or two fractures are not always apparent on a chest radiograph. Multiple rib fractures usually can be seen (Fig. 25-1). Rib fractures may be associated with underlying lung injury such as pneumothorax, hemothorax, or pulmonary contusion.
Flail Chest
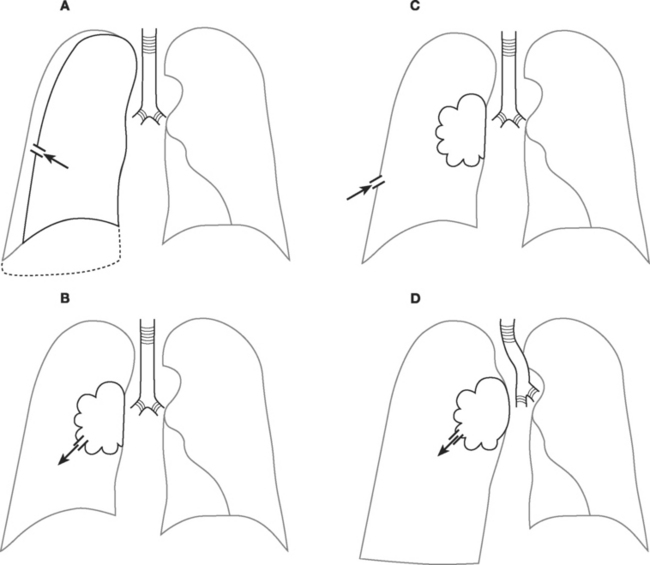
Multiple rib fractures may result in a flail chest (Fig. 25-2), in which a section of the chest wall moves paradoxically with respiration. Flail chest is almost always associated with significant underlying pulmonary contusion and severe respiratory compromise. Treatment is supportive: oxygen or ventilatory support for hypoxemia and respiratory distress along with physical therapy and adequate analgesia. Some data show that open reduction and internal fixation of the flail segment is associated with less pain and a shorter hospital stay than is a conservative approach.1
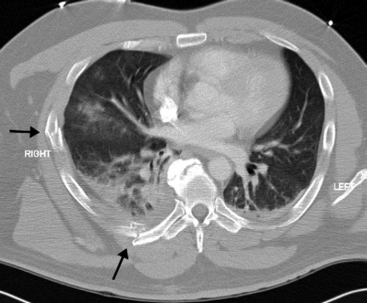
Figure 25.2 Transverse CT scan of the patient in Figure 25-1. On the right side, posteriorly, a fractured rib is seen. This fracture is seen on the radiograph. However, laterally a further fracture is seen, which is not apparent on the plain radiograph. This patient has a substantial flail segment of the right chest wall. A small right pleural collection and contusion of the right lung is also seen.
LUNG INJURIES
Pulmonary Contusion
Pulmonary contusion is common following severe blunt thoracic trauma and blast injury. The presence of a significant chest wall injury indicates a high likelihood of an underlying pulmonary contusion. Radiographically, pulmonary contusion appears as a region of dense alveolar shadowing (see Fig. 25-1), often underlying chest wall soft-tissue swelling and rib fractures. Treatment is supportive.
Pneumothorax
Pneumothoraces may be open or closed, large or small, simple or under tension (Fig. 25-3). With an open pneumothorax, there is a breach in the chest wall that allows air to enter the chest cavity through the defect (rather than through the trachea, as occurs with a closed pneumothorax). Patients present with a “sucking” chest wound and severe respiratory distress. The pneumothorax is likely to be large and there may be an associated hemothorax and flail segment. Immediate intubation and invasive ventilation may be required. Treatment involves urgent surgical repair. If immediate surgical repair is not possible, the wound should be covered with an impermeable dressing and a thoracostomy tube should be inserted and connected to an underwater seal drain. The dressing should be sealed on only three sides, with the lower side left unsealed to allow air under tension to escape from the chest while preventing air entrainment through the wound. Once the thoracostomy tube is inserted, the dressing should be completely sealed. Surgical repair should be arranged as soon as possible.
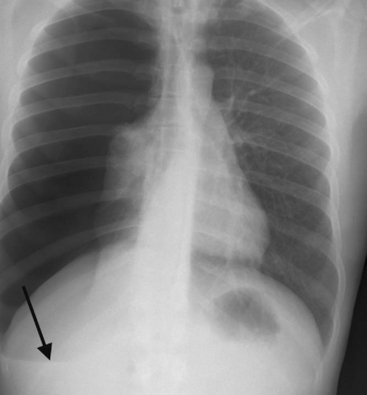
Tension and large simple pneumothoraces are usually diagnosed clinically. Both present with respiratory distress, reduced breath sounds on the affected side, and hyperresonance to percussion. With a tension pneumothorax (Fig. 25-4), the patient may be in shock because of compression of the mediastinal structures and obstruction to venous return. The trachea may be deviated to the unaffected side and there may be displacement of the apex beat. A simple pneumothorax (see Fig. 6-21) may be converted into a tension pneumothorax with the institution of positive pressure ventilation. With severe respiratory distress or shock, needle thoracocentesis should be performed without delay, commonly before the chest radiograph is available. Needle thoracocentesis should be followed immediately by tube thoracostomy and underwater seal drainage (see Chapter 40). With simple pneumothoraces, lung reinflation is usually rapid and, providing there is no ongoing air leak, the tube can be removed in as short a time as a few hours in cases of penetrating trauma or in 1 to 2 days after blunt trauma.2 Whenever a large pneumothorax occurs after penetrating trauma, the possibility of an airway injury must be considered.
Small, simple pneumothoraces are commonly diagnosed incidentally on a chest radiograph or on an abdominal computed tomogram (CT).3 Whether these incidentally identified pneumothoraces require tube thoracostomy is debatable. As a general rule, if positive pressure ventilation is required4 or if the patient is to be transported by air, drainage is mandatory.
Hemothorax
Isolated hemothorax typically presents with hypovolemic shock, with or without respiratory distress. Breath sounds are reduced on the affected side but, unlike in pneumothorax, the chest is dull to percussion. The diagnosis is confirmed by chest radiography (see Fig. 6-26). Initial treatment involves ensuring that large-bore intravenous cannulas are placed above and below the diaphragm. Insertion of at least one and sometimes two thoracostomy tubes is necessary, and they should be of large size (28F or larger) so as to reduce the chances of their occlusion by clot. The initial and subsequent blood loss must be carefully monitored. When initial blood loss is more than 1500 ml in penetrating trauma or 2000 ml in blunt trauma, immediate thoracotomy should be considered.5 If the patient is grossly unstable or moribund, thoracotomy should be undertaken in the emergency department. Regardless of the initial amount of blood loss, thoracotomy should be considered if blood loss exceeds 800 ml in 4 hours. If the placement of one or more thoracostomy tubes fails to clear the thoracic cavity of blood in 2 to 3 days, surgical evacuation should be considered. This can often be performed thoracoscopically,6 but if the clot is well organized, thoracotomy will be required.
Surgical exploration of thoracic stab wounds (unlike abdominal stab wounds) is not mandatory. Similarly, there is no indication for thoracotomy to remove bullets unless they have embolized to pulmonary vessels or are lodged in the myocardium in a way likely to cause functional problems.
Lung Laceration
Lung laceration is common in penetrating trauma and has also been described after major blunt trauma. It is difficult to diagnose but is often associated with ongoing blood loss or air leak, in which case thoracotomy is indicated. At the time of surgery there is no need to repair the laceration specifically, but there should be no ongoing air leak or bleeding from the cut surface of the lung. If the lung laceration results from penetrating trauma, “tractotomy” may be required, in which the lung tissue overlying the penetrating tract is divided by a cutting stapler so that the bleeding and air leak from the deep parts of the tract can be seen and dealt with.7
Tracheal Injury
Tracheal injury is rare in blunt trauma but may occur in penetrating trauma. It represents a life-threatening airway problem. Depending on the location of the injury, it may present with dramatic subcutaneous or mediastinal emphysema or with a profuse air leak into one or both hemithoraces. In cases of nonpenetrating trauma, tracheal injury may be difficult to diagnose because the signs—respiratory distress, cough, hemoptysis, and subcutaneous emphysema—are relatively nonspecific.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree