Chapter 11 Thoracic Aorta
There are four main lesions of the thoracic aorta that present for management: dissection, aneurysm, rupture, and aortic coarctation. The focus in this chapter is on the first two of these conditions; traumatic aortic rupture is covered in Chapter 25, and aortic coarctation is covered briefly in Chapter 15.
ANEURYSMS OF THE THORACIC AORTA
Etiology
The causes of thoracic aortic aneurysms are summarized in Table 11-1. Atherosclerotic degeneration is the most common cause of aneurysms involving the descending thoracic and thoracoabdominal aorta. Risk factors include increased age, smoking, and hypertension.
Table 11-1 Causes of Thoracic Aortic Aneurysms
| Degeneration |
| Hypertension |
| Atherosclerosis |
| Cystic medial necrosis |
| Genetic or congenital origin |
| Marfan syndrome |
| Ehlers-Danlos syndrome |
| Bicuspid or unicuspid aortic valve |
| Inflammation |
| Takayasu arteritis |
| Behçet arteritis |
| Kawasaki disease |
| Polyarteritis |
| Infection |
| Aortic stenosis |
Aneurysms of the proximal ascending aorta may result from chronic flow turbulence due to aortic valve stenosis (poststenotic dilatation). In addition, patients with bicuspid or unicuspid aortic valves are at increased risk for aortic aneurysm formation due to primary structural abnormalities of the aortic wall.1 Thoracic trauma, usually a sudden deceleration injury, is a rare cause of chronic aneurysm formation. This is usually caused by intimal disruption in the area of the aortic isthmus. A pseudoaneurysm (false aneurysm) is a collection of thrombus and connective tissue outside the aortic wall that occurs as a result of a contained rupture. Pseudoaneurysms typically occur secondary to infection, trauma, or previous aortic surgery.
Classification
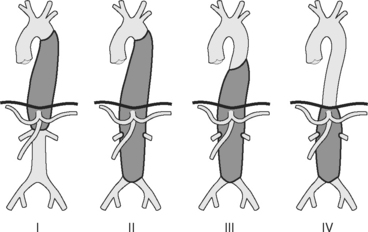
Aneurysms of the thoracic aorta can be classified on the basis of their anatomic position. Ascending aortic aneurysms arise anywhere from the aortic valve to the innominate artery. Aortic arch aneurysms involve aorta bounded by the brachiocephalic vessels. Descending thoracic and thoracoabdominal aneurysms arise distal to the left subclavian artery. Thoracoabdominal aneurysms are further divided according to the Crawford classification (see Fig. 11-1).
Natural History
An aortic aneurysm is a slowly progressive but intrinsically lethal condition that eventually undergoes rupture or dissection. The primary determinant of adverse outcome is aneurysm size: a patient with a maximal aortic dimension of 6 cm has an annual risk for rupture, dissection, or death of 14%.2
The growth rate of aneurysms is not linear, tending to accelerate as the aneurysm increases in size (see Wall Stress and Aneurysm Growth in Chapter 1). Aneurysms grow faster in patients who smoke, in patients who are hypertensive, in aortas with dissections, and in the thoracic aorta rather than the abdominal aorta.
Surgical intervention is recommended when the maximal aortic diameter exceeds 5.5 cm in the ascending aorta and 6 to 6.5 cm in the descending aorta.2,3 These recommendations are based on the relative risks for rupture or dissection compared with the risks involved in surgery.
Aneurysms caused by Marfan syndrome display accelerated unpredictable growth patterns and have a tendency to rupture or dissect at a smaller size than do aneurysms in patients without Marfan syndrome. This is particularly the case if there is a family history of early complications. Surgery is recommended for patients with Marfan syndrome when the maximal diameter exceeds 5 cm in the ascending aorta and 6 cm in the descending aorta.2
Clinical Features and Investigations
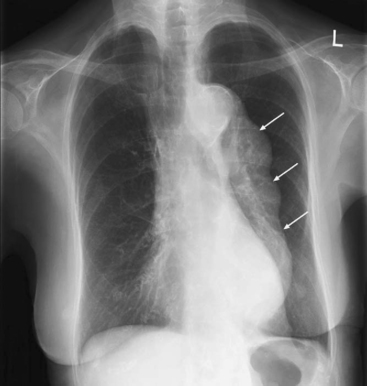
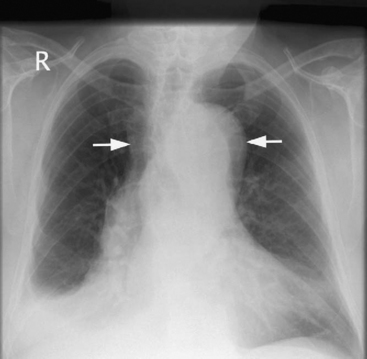
The aneurysm may be apparent on a chest radiograph. With an ascending aneurysm, there may be a prominent right aortic border on the frontal projection and filling in of the upper substernal space on the lateral projection. With an arch aneurysm there may be widening of the mediastinum on the frontal projection. An enlarged descending thoracic aorta may be seen behind the heart on the frontal and lateral projections (Fig. 11-2).
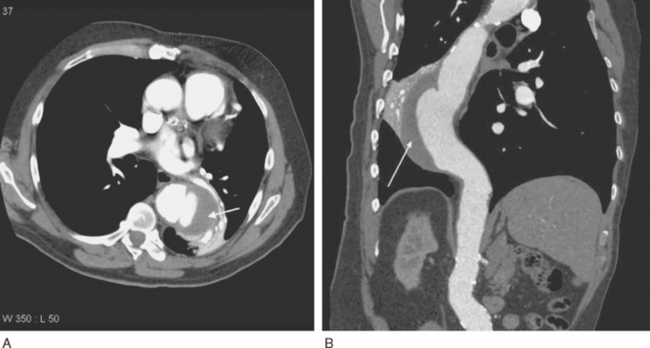
Imaging of thoracic aortic aneurysms may be undertaken by echocardiography, computed tomography (CT), or magnetic resonance (MR) imaging. Echocardiography allows accurate assessment of aortic regurgitation, aortic leaflet morphology, and ventricular function, but it may not fully delineate the anatomic extent and relationships of the aneurysm. Echocardiography is particularly poor at imaging the distal ascending aorta and aortic arch. To image the aneurysm itself accurately, either a contrast CT scan (Fig. 11-3A) or MR imaging scan is required. For patients undergoing aneurysm surveillance, conventional axial CT scanning is sufficient. For operative planning, CT or MR imaging with three-dimensional reconstruction is extremely helpful (Fig. 11-3B).
Treatment of Thoracic Aneurysms
In patients with small aneurysms, regular surveillance by CT scanning is indicated; the frequency of scanning is determined by the size and growth pattern of the aneurysm. Medical treatment primarily involves control of hypertension. β Blockers are a good choice for blood pressure control because they reduce tension in the aneurysm wall and, unlike arteriolar vasodilators, do not increase shear forces in the aorta.4 Drug treatment of hyperlipidemia and diabetes may also be indicated. Smoking cessation, diet, and exercise are all important preventive strategies for atherosclerosis.
Preoperative Assessment
Aortic aneurysms and dissections typically occur in older patients with histories of smoking, hypertension, and chronic obstructive pulmonary disease. There is frequently coexisting coronary artery, carotid artery, and peripheral vascular disease. Furthermore, open repair of thoracic aortic aneurysms imposes a huge physiologic insult on patients. Thus, it is essential to fully investigate and optimize patients prior to surgery.
An echocardiogram should be performed on all patients; with particular emphasis on aortic valve and ventricular function. Patients over 40 years of age and those with risk factors for coronary artery disease should undergo coronary angiography.5
More than one third of patients undergoing surgery for thoracic aortic aneurysms have either a diagnosis of chronic obstructive pulmonary disease or a history of heavy smoking.6 These patients should have spirometry and arterial blood gases performed preoperatively. They are also likely to benefit from a period of smoking cessation, chest physiotherapy, and appropriate treatment of the infective and bronchospastic components of their respiratory diseases. The management of patients with obesity, renal failure, carotid disease, and diabetes is similar to that outlined in Chapter 9.
AORTIC DISSECTION
Intramural hematoma is due to a burst vessel in the media, causing a hematoma, which may then lead to a tear and communication with the aortic lumen. A penetrating atherosclerotic ulcer is ulceration within an atherosclerotic plaque that extends down to the level of the media. Both intramural hematoma and penetrating atherosclerotic ulcer have high incidences of dissection and rupture.7,8
Etiology
The causes of aortic dissection are similar to the causes of aortic aneurysm (see Table 11-1). Indeed, dissection, intramural hematoma, and atherosclerotic plaque rupture can all complicate an aortic aneurysm. An additional cause of aortic dissection is iatrogenic aortic injury due to surgical manipulations such as the placement of aortic cannulas during cardiopulmonary bypass.
Classification
Most aortic dissections begin in the ascending aorta and extend distally, although between 5% and 10% begin in the arch, and 30% to 35% begin in the first part of the descending aorta. There are two main classification systems, based on the extent of aortic involvement (Fig. 11-4). The Stanford classification is used here.9
Clinical Features and Investigations
Type A Dissection
Type A aortic dissections can result in the following complications:
Patients commonly present with shock due to the combined effects of pericardial tamponade and aortic regurgitation. In the absence of these complications, patients may be hypertensive. Patients may develop a major neurologic deficit, such as impaired consciousness, hemiplegia, paresthesia, or paraplegia. Pulses (brachial, carotid, femoral) may be weak, absent, or asymmetric. Four-limb blood pressure measurements may show marked variability. The chest radiograph may demonstrate widened mediastinum and loss of the aortic knuckle (Fig. 11-5).
Imaging
Patients who present with symptoms and signs consistent with aortic dissection require urgent diagnostic imaging. Options include transesophageal echocardiography (TEE), CT scanning, MR imaging, and aortography, all of which have a sensitivity and specificity greater than 90%.10 Intramural hematoma may be difficult to diagnose with any of these techniques. The preferred initial investigation varies according to the institution, but CT scanning is the most widely used modality.11 CT scanning has the advantage of being rapid (unlike MR imaging) and does not require sedation or general anesthesia (unlike TEE). Aortography is rarely indicated other than as part of a stenting procedure. CT scanning demonstrates the extent of the dissection (Fig. 11-6) and the presence of any pericardial blood but does not usually demonstrate the entry tears or any associated aortic regurgitation.
TEE is the most useful investigation for determining the severity of any associated aortic regurgitation (Fig. 11-7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree